Abstract
We report herein an unusual case of diffuse infiltrating retinoblastoma involving the brain, which caused a patient’s death 27 months after enucleation. An eight-year-old boy complained of blurred vision in his right eye (OD) in October 2006. Funduscopic examination showed optic disc swelling, dense whitish vitreous opacity, and an orange-colored subretinal elevated lesion adjacent to the optic disc. Fluorescein angiography revealed hyperfluorescence in the peripapillary region at an early-phase OD. Because the size of the subretinal lesion and vitreous opacity gradually increased, he was referred to us. His visual acuity was 20/1000 OD on June 20, 2007. Slit-lamp biomicroscopy showed a dense anterior vitreous opacity. Ophthalmoscopically, the subretinal orange-colored area spread out until reaching the mid peripheral region. A B-mode sonogram and computed tomography showed a thick homogeneous lesion without calcification. Gadolinium-enhanced magnetic resonance imaging showed a markedly enhanced appearance of the underlying posterior retina. Enucleation of the right eye was performed nine months after the initial presentation. Histopathology demonstrated retinal detachment and a huge choroidal mass invading the optic nerve head. The tumor was consistent with diffuse infiltrating retinoblastoma. The patient died due to brain involvement 27 months after enucleation. Ophthalmologists should be aware that diffuse infiltrating retinoblastoma may show an unfavorable course if its diagnosis is delayed.
Introduction
Diffuse infiltrating retinoblastoma, a rare atypical retinoblastoma, is characterized by a diffuse infiltration of tumor cells in the retina without any focal mass. Almost all patients with diffuse infiltrating retinoblastoma show unilateral sporadic retinoblastomas. The prognosis is better than for infantile retinoblastomas, if enucleation is conducted before metastasis.Citation1,Citation2 Herein, we report an unusual case of diffuse infiltrating retinoblastoma involving the brain, which caused the patient’s death 27 months after enucleation.
Case report
An eight-year-old boy complained of blurred vision in his right eye (OD) in October 2006. His visual acuity was 20/63 OD. The left eye was normal. Funduscopic examination showed optic disc swelling, dense whitish vitreous opacity, and an orange-colored subretinal elevated lesion (, arrowhead) adjacent to the optic disc. Fluorescein angiography revealed hyperfluorescence in the peripapillary region at an early phase OD (). Although a diagnosis of atypical retinoblastoma was suspected, it was difficult to differentiate from granulomatous uveitis at this stage. Because the size of the subretinal lesion and vitreous opacity gradually increased, he was referred to us.
Figure 1 Fundus photograph (A), fluorescein angiography (B), slit-lamp biomicroscopy (C), and gadolinium-enhanced T1-weighted MRI of the right eye (D). A) The fundus was blurred due to the dense vitreous opacity. The optic disc was swollen, and there was an elevated orange-colored subretinal lesion situated adjacent to the optic disc (arrowhead). B) Hyperfluorescence in the initial phase (arrowhead) in the orange-colored subretinal lesion and optic disc. C) Whitish dense anterior vitreous opacity. D) A markedly enhanced appearance underlying the posterior retina.
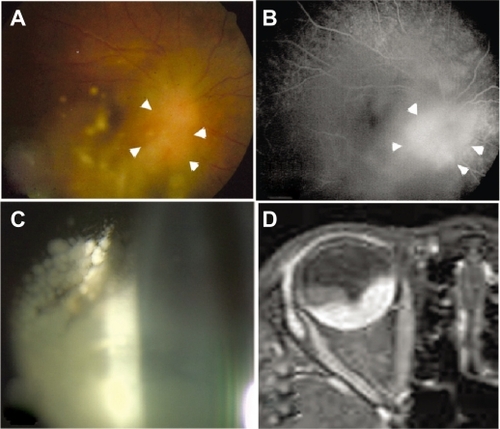
His visual acuity was 20/1000 OD on June 20, 2007. Slit-lamp biomicroscopy showed a dense anterior vitreous opacity (). Ophthalmoscopically, the subretinal orange-colored area spread out until reaching the mid peripheral region. A B-mode sonogram and computed tomography showed a thick homogeneous lesion without calcification. Gadolinium-enhanced magnetic resonance imaging showed a markedly enhanced appearance of the underlying posterior retina (). Because atypical retinoblastoma was suspected, enucleation of the right eye was performed on July 3, 2007.
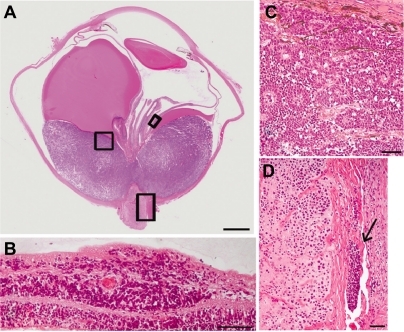
Histopathology demonstrated retinal detachment and a huge choroidal mass invading the optic nerve head (). In the retina, tumor cells invaded the ganglion cell layer without forming masses (). In the choroidal mass, tumor cells were tightly packed, and contained large hyperchromatic nuclei and scant cytoplasm. The tumor cells were consistent with retinoblastoma cells. Rosette formation was frequently observed (), but neither a necrotic area nor calcified lesion was found. There were infiltrating tumor cells in the parenchyma of the optic nerve and subarachnoid space (, arrow). The infiltration of tumor cells extended 10 mm into the subarachnoid space of the optic nerve up to the line of surgical transection. Tumor cells were also observed in the choroidal veins, and along the path of the long posterior ciliary artery in the scleral canal. In contrast, there were no tumor cells in the anterior segments, including the corneal endothelium and anterior chamber. After enucleation, the patient was treated with chemoradiotherapy combined with autologous stem cell support. However, the patient died due to brain involvement 27 months after enucleation.
Figure 2 Histopathology of the enucleated eye. Hematoxylin and eosin staining. A) Retinal detachment with a huge choroidal mass invading the optic nerve head. Bar indicates 3 mm. B) Tumor cells invaded the ganglion cell layer without forming masses. Bar indicates 50 um. C) Tumor cells were tightly packed, and contained large hyperchromatic nuclei and scant cytoplasm. Rosette formation was observed in the choroidal mass. Bar indicates 50 um. D) Tumor cells infiltrated the parenchyma of the optic nerve and subarachnoid space (arrow). Bar indicates 50 um.
Discussion
In this case, funduscopic examination showed no retinal whitish solitary tumor, which is observed in typical retinoblastoma. Histological examination demonstrated that retinoblastoma cells diffusely invaded the ganglion cell layer without forming masses, assuming ill-defined horizontal growth along the retinal tissue with little vertical growth. Taken together, the diagnosis of this tumor was consistent with diffuse infiltrating retinoblastoma. However, this case was considered unusual because an orange-colored subretinal elevated lesion, a huge choroidal mass, and frequent rosette formations were present, which are not typically observed in patients with diffuse infiltrating retinoblastoma. At histological evaluation, an orange-colored subretinal elevated lesion corresponded to retinoblastoma cell infiltration with rosette formation in the choroid.
Histology of the enucleated eye revealed the presence of retinoblastoma cells in the optic nerve, subarachnoid space, choroidal vessels, and trans-scleral canal. The route of brain involvement in this retinoblastoma seems to have been through the optic nerve and subarachnoid space, instead of choroidal vessels or the trans-scleral canal. Therefore, it is consistent with the route of brain involvement in patients with typical retinoblastoma. If the tumor cells had invaded the subarachnoid space, following the choroidal vessels or trans-scleral canal involvement, systemic metastasis would have occurred in the liver and/or lung through blood flow, which was not observed in the present case.
A patient with histologically presumed diffuse infiltrating retinoblastoma was reported, who died due to brain involvement in 1957.Citation3 Subsequent reviews disclosed the outcome of consecutive enucleated eyes with diffuse infiltrating retinoblastoma, in which there were no cases of metastases on long-term follow-up.Citation1,Citation2 However, the present patient subsequently developed brain involvement, leading to the patient’s death 27 months after enucleation. This indicates that a favorable prognosis relies on making a diagnosis much earlier than in this patient. It is known that the presence of a tumor in the subarachnoid space is a risk factor for brain involvement in typical retinoblastoma.Citation4 Ophthalmologists should make sure that diffuse infiltrating retinoblastoma has an unfavorable course if its diagnosis is delayed.
Acknowledgements
This study was supported by the Research Foundation of the Japan Society for the Promotion of Science, and by grants-in-aid from the Scientific Research from The Ministry of Education, Culture, Sports, Science, and Technology.
Disclosure
The authors report no conflicts of interest in this work.
References
- MorganGDiffuse infiltrating retinoblastomaBr J Ophthalmol1971556006064106451
- ShieldsCLGhassemiFTuncerSThangappanAShieldsJAClinical spectrum of diffuse infiltrating retinoblastoma in 34 consecutive eyesOphthalmology20081152253225818962920
- WeizenblattSDifferential diagnostic difficulties in atypical retinoblastoma. Report of a caseArch Ophthalmol195758699709
- FingerPTHarbourJWKarciogluZARisk factors for metastasis in retinoblastomaSurv Ophthalmol20024711611801265