Abstract
Purpose:
To evaluate and record the common complications that face surgeons when they perform their first few series of deep lamellar keratoplasty and measures to avoid these.
Setting:
Dar El Oyoun Hospital, Cairo, Egypt.
Methods:
Retrospective study of the first 40 eyes of 40 patients carried out by two corneal surgeons working in the same center. All patients were planned to undergo a deep anterior lamellar keratoplasty using the big bubble technique. Twelve patients suffered from keratoconus while 28 patients had anterior corneal pathologies. Recorded complications were classified as either intraoperative or postoperative.
Results:
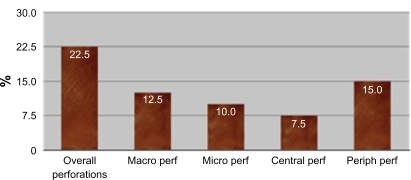
Perforation of Descemet’s membrane was the most common intraoperative complication. It occurred in nine eyes (22.5%): five eyes (12.5%) had microperforations while four eyes (10%) had macroperforations, three eyes (7.5%) had central perforations, and six eyes (15%) had peripheral perforations. Other complications included incomplete separation of Descemet’s membrane and remnants of peripheral stromal tissue. Postoperative complications included double anterior chamber which occurred in four eyes (10%) and Descemet’s membrane corrugations. Postoperative astigmatism ranged from 1.25 to 4.5 diopters with a mean of 2.86 diopters in the whole series, but in the six cases with identified residual stroma in the periphery of the host bed, the astigmatism ranged from 2.75 to 4.5 diopters with a mean of 3.62 diopters.
Conclusion:
Deep lamellar keratoplasty is sensitive to procedural details. Learning the common complications and how to avoid them helps novice surgeons to learn the procedure faster.
Deep anterior lamellar keratoplasty (DALK) is becoming more widely used corneal surgery because of its suitability for corneal opacities that are limited to the corneal stroma not involving Descemet’s membrane, as well as corneal ectatic conditions with no Descemet’s membrane defects or scars. Its superiority over penetrating keratoplasty lies in the fact that the donor graft is transplanted devoid of its main antigenic load, the corneal endothelium. This technique, when performed successfully, nearly eliminates the risk of immunologic rejection.Citation1,Citation2
DALK though is not without problems. First, it is a difficult procedure to learn and is very sensitive to procedural details. Because it is a new procedure, I could not find a comprehensive review discussing the most common complications and how to avoid them, especially for novice surgeons.Citation3
I carried out a survey to summarize the complications that the novice DALK surgeon would encounter, graded them by frequency, and collected suggestions on how best to avoid them.
Methods
This was a retrospective study investigating the recorded video clips and hospital files of the first 40 eyes of 40 patients operated on by two corneal surgeons working in the same center. All patients were planned to undergo a DALK using the big bubble technique proposed by Anwar and Teichmann.Citation4
Twelve patients suffered from keratoconus and 28 patients had anterior corneal pathologies. Complications were classified as intraoperative and postoperative. Common complications were given more weight, and ways to avoid them in the future suggested by the surgeons were recorded as well as the efficacy of these precautions to provide safety in subsequent surgeries.
Details of the operative technique
After marking the center of the cornea, a partial thickness corneal trephination is carried out on 60% of the corneal pachymetry measured preoperatively with a Pentacam® (Oculus GmbH). Trephination is carried out by a Hessburg–Barron suction trephine and then a paracentesis is performed and aqueous is allowed to escape to lower the intraocular pressure and to give space for injecting the air bubble intrastromally. A small air bubble is then injected in the anterior chamber to act as a visual guide for the Descemet’s membrane dissection, as will be described later.
A 29-gauge hypodermic needle fitted on a 5-mm syringe is bent bevel down and introduced at the base of the trephination gutter directed towards the center of the pupil in a plane parallel to the corneal plane and advanced intrastromally for at least 2 mm. No specially designed air cannula was used in this study.
Air is injected via the syringe with a firm and consistent pressure, observing at first intrastromal blanching then the separation wave of the Descemet’s membrane from the stroma and the formation of the posterior descemetocele with the air bubble. This is confirmed by the push of the previously injected small anterior chamber bubble to one side.
The anterior portion of the corneal stroma is dissected and removed using a disposable crescent knife to expose the posterior portion of the corneal stroma overlying the big air bubble.
The roof of the air bubble is punctured at the center of the cornea by carefully using a 15 degree superblade and viscoelastic gel is injected from the puncture site to keep the Descemet’s membrane away from the corneal stroma.
Right and left Fogla Scissors (Bausch and Lomb) with longer lower blades and shorter upper blades are then used to cut the stroma from center to the edge of the trephination circle in the four cardinal directions and then each quadrant of the posterior stroma is removed using the same scissors, exposing the bare Descemet’s membrane.
The donor graft is then prepared by removing its Descemet’s membrane using capsulorhexis forceps after staining the membrane with gentian violet and drying it thoroughly with a Merocel® sponge (Medtronic).
The graft is then placed on the exposed recipient Descemet’s membrane and secured with 16 interrupted ten nylon sutures.
Although we have described a newer technique, namely the early bubble technique, to enhance the safety of the big bubble technique, we did not use our published modification, which we started to apply after these early cases were performed and recorded.Citation6
Results
Intraoperative complications
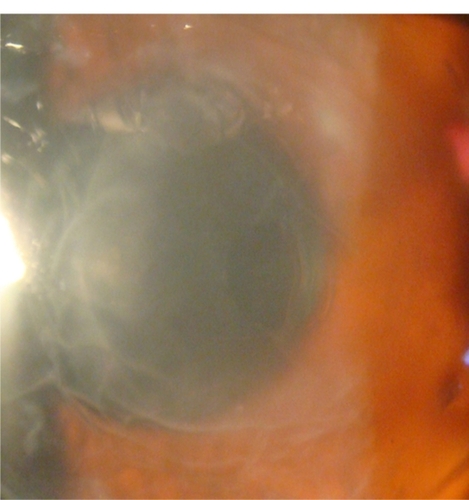
Perforation of Descemet’s membrane ()
This was by far the most common complication in this series of patients. Perforations varied according to their site of occurrence, ie, central or peripheral, their size, ie, small microperforations or macroperforations, and according to the step in which the perforation occurred.
Perforation occurred in nine out of 40 eyes (22.5%). Only three of the nine were corneas with keratoconus. Five eyes (12.5%) had microperforations and four (10%) had macroperforations (); three eyes (7.5%) had central perforations and six (15%) had peripheral perforations. All three central perforations were microperforations and in the six peripheral perforation cases, two were microperforations and four were macroperforations.
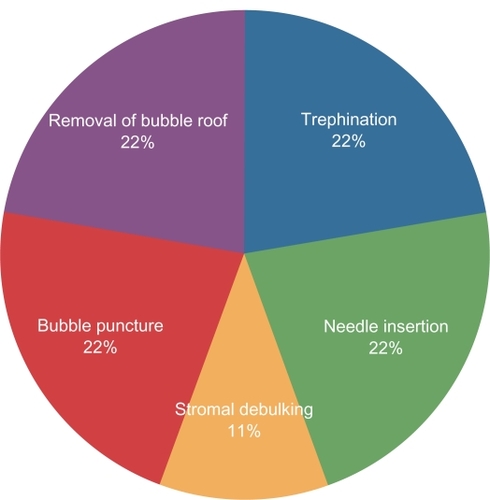
According to the surgical step ()
During partial thickness trephination (two cases) (5%), both resulted in peripheral macroperforations. During needle insertion in the corneal depth (two cases) (5%), both resulted in peripheral microperforations. During lamellar corneal dissection before opening the big bubble, one case (2.5%) was a central microperforation. During central puncture of the big bubble (two cases) (5%), both were central microperforations. During scissor removal of the corneal stoma to leave a bare Descemet’s membrane (two cases) (5%), both resulted in peripheral macroperforations.
Incomplete separation of Descemet’s membrane from the stroma
This occurred in only two cases where the Descemet’s membrane was separated partially only by the air bubble but retained its firm adhesion with the back of the corneal stroma at one side central to the trephination site. During attempted stromal tissue removal by scissors, Descemet’s membrane was punctured by the scissors, resulting in peripheral perforations.
Remnants of peripheral stromal tissue under the graft ()
A small amount of residual stromal tissue remained and the graft was implanted over it in six cases (15%). This tissue was deliberately left for fear of Descemet’s membrane rupture during its removal. In these six cases, the resultant astigmatism 6 weeks postoperatively ranged from 2.75 to 4.5 diopters.
Stony hard increase of intraocular pressure after big bubble injection
This occurred in the first three cases (7.5%) where a side port was not performed before injection. In the following cases, aqueous was released before and immediately after air injection to avoid increasing intraocular pressure.
It is noteworthy that all the aforementioned intraoperative complications occurred in the first 19 cases of the series.
Postoperative complications
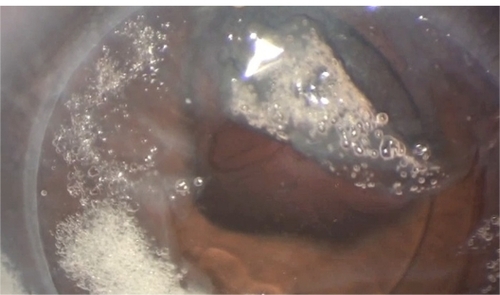
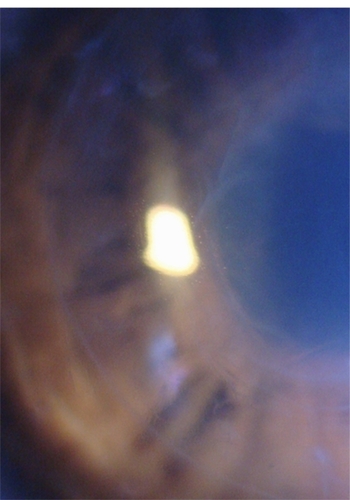
Double anterior chamber ()
This occurred in four eyes (10%), two of which were among the three eyes that suffered from central microperforations. Both patients were taken back to the operating room where they underwent intracameral air injection to push the Descemet’s membrane towards the back surface of the corneal stroma. The double chamber disappeared by the next day.
In the other two patients who had double anterior chamber, no definite cause could be identified. It was probably due to a small amount of residual viscoelastic material that remained on the surface of Descemet’s membrane which was not washed properly. In these two patients, the double anterior chamber cleared spontaneously after 2 days with no sequelae.
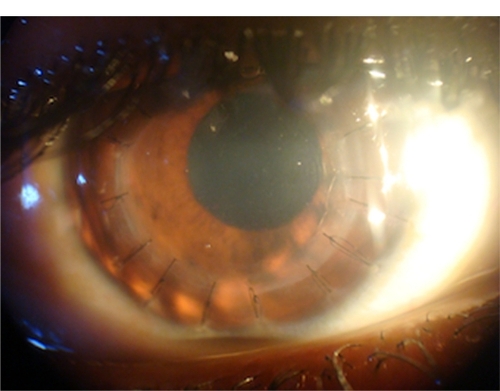
Descemet’s membrane corrugations ()
These were concentric corrugations in the Descemet’s membrane which had no visual sequelae, occurring in only 15 out of the 40 eyes (37.5%). No cause for this finding was identified and even its classification as one of the postoperative complications is doubtful.
Postoperative astigmatism
In the whole series, postoperative astigmatism ranged from 1.25 to 4.5 diopters (mean 2.86 diopters). In the six cases with identified residual stroma in the periphery of the host bed, astigmatism ranged from 2.75 to 4.5 diopters with a mean of 3.62 diopters. The astigmatism was measured 1 week after suture removal in all cases by a TMS 5 combined Scheimpflug Placido corneal topographer (Tomey, Nagoya, Japan).
Discussion
DALK is not without complications. We have mentioned the complications that we encountered in our early phase of learning. Descemet’s membrane perforation, the only complication reported in the literature, seemed the most common and the most frustrating complication faced. In other studies, its incidence varied from 9% to 20%.Citation5 It can happen during different steps of the procedure. During early partial thickness trephination, when only 60% of the measured preoperative corneal thickness is targeted, it may occur due to the softness of the corneal tissue in ecstatic corneal conditions where more cornea is cut by the suction trephine per 90° rotation than the estimated 50 to 60 μm per one-quarter of a turn. It can also happen during insertion of the 29-gauge needle in the stromal depth especially when following the exact steps explained by Anwar and TeichmannCitation4 in their original big bubble technique where the needle is inserted from the depth of the partial thickness trephination gutter in the direction of the central cornea, which is particularly thinned out in keratoconus. It can also occur during debulking of the corneal stroma or during deroofing of the Descemet’s membrane, the latter condition being the most frustrating as the surgeon would have invested more time to execute the DALK before perforation occurs. By consensus of both corneal surgeons who performed this series of cases, the measures to avoid perforation of Descemet’s membrane included paracentesis before the bubble injection and release of aqueous after bubble injection, and performing pachymetry before the procedure to prevent perforation during trephination. The needle should be inserted under magnification and the same level of needle penetration should be maintained. If perforation does occur though, both surgeons agreed that if it is a macroperforation, conversion to penetrating keratoplasty is mandatory. If the perforation is small, peripheral perforations can be ignored and the procedure continued in the normal fashion. Central microperforations should be evaluated individually to assess whether it is safe to continue with the DALK or convert to a penetrating keratoplasty. Continuing with a DALK in these situations carries the risk of postoperative double chamber. To avoid incomplete separation of Descemet’s membrane from the corneal stroma, the surgical emphysema must always be well beyond the trephination zone and if the bubble is small, the needle should be reinserted in a different location to reinject air into the original bubble. Although it seems intuitive that thinner corneas are at higher risk, I found that perforation rate in this study was not higher in keratoconic than in nonkeratoconic corneas. Nevertheless it is logical to recommend that novice surgeons try to select patients with pure stromal pathology but a relatively normal and uniform corneal thickness.
The postoperative complications that were not related to a Descemet’s membrane perforation include postoperative Descemet’s membrane corrugations and host stromal remnants under the graft; the former had no consequences on the postoperative visual acuity while the latter caused higher postoperative astigmatism values. To my knowledge, no comprehensive report about the incidence of complications of DALK and how to avoid them has been published. I have summarized the complications and how they could be avoided in order to help the department as well its trainees perform better DALK, a technique I believe is an important weapon in the armamentarium of the corneal surgeon.
Prior publication
The results in this paper were first presented at the American Society of Cataract and Refractive Surgery (ASCRS) Annual Symposium in San Fransisco, April 3 to 8, 2009.
Disclosure
The author declares no conflicts of interest.
References
- Anita PandaAPangteyM SSonyPKhokharPBig bubble technique in anterior lamellar keratoplastyJ Cataract Refract Surg20022812206712498820
- ColinJVelouSCurrent surgical options for keratoconusJ Cataract Refract Surg200329237938612648653
- SharmaNJhanjiFTitiyalJSAmielHVajpayeeRBUse of trypan blue dye during conversion of deep anterior lamellar keratoplasty to penetrating keratoplastyJ Cataract Refract Surg20083481242124518655971
- AnwarMTeichmannKDBig-bubble technique to bare descemet’s membrane in anterior lamellar keratoplastyJ Cataract Refract Surg200228339840311973083
- LeccisottiADescemet’s membrane perforation during deep anterior lamellar keratoplasty: prognosisJ Cataract Refract Surg200733582582917466856
- HosnyMShalabyABadrElDinNEarly bubble modification of the big bubble technique for deep anterior lamellar keratoplastyEur J Ophthalmol201020228328920213619