Abstract
We report a case of myopic choroidal neovascularization that showed improvement after a single injection of ranibizumab. A 45-year-old Chinese man with high myopia presented with sudden onset painless central scotoma of his right eye of 2 weeks’ duration. There was no history of trauma. His right eye vision on presentation was 6/30 which showed no improvement with pinhole. The right fundus showed myopic maculopathy at the posterior pole with subretinal hemorrhage at the inferotemporal fovea. The optic disc was tilted with inferotemporal peripapillary atrophy. There was a myopic maculopathy appearance in the macula of the left eye. Fundus fluorescein angiography revealed choroidal neovascularization at the fovea of the right eye. A diagnosis of right eye choroidal neovascularization secondary to myopic maculopathy was made. A single intravitreal injection of ranibizumab 0.05 mL was given. Ten weeks following intravitreal injection, vision had improved to 6/7.5, and repeated fundus fluorescein angiography showed absence of choroidal neovascularization. Follow-up at 6 months showed visual acuity had normalized to 6/6 with glasses, which was maintained up to 12 months following treatment. The right fundus showed no further subretinal hemorrhage with no new lesions.
Introduction
Choroidal neovascularization (CNV) is a common cause of vision loss in pathological myopia.Citation1 The pathogenesis of CNV in pathological myopia is still unclear but is postulated to result from axial elongation of the globe causing distension of the posterior segment with greater ocular volume than in the normal eye. This results in stretching of the macula within the staphyloma and induces intraretinal retinochisis. Later on, the formation of lacquer cracks leads to CNV.Citation1
The most appropriate treatment for myopic CNV has not yet been established and the choices are limited.Citation2 Antivascular endothelial growth factor seems to offer a new modality for management of pathological myopia. We report a case of myopic CNV that showed improvement after a single injection of ranibizumab.
Case report
A 45-year-old Chinese man, who was a known case of high myopia with a spherical equivalent refractive error of −5.0 diopter (D), presented with sudden onset painless reduced vision of his right eye of 2 weeks’ duration. He described it as a central scotoma. There was no metamorphopsia, and there was no relationship with headache, jaw claudication, or double vision. He had undergone bilateral cataract surgery 10 years before presentation, and had a good visual outcome postoperatively with glasses. The cataract operation was uneventful and there was no history of eye trauma.
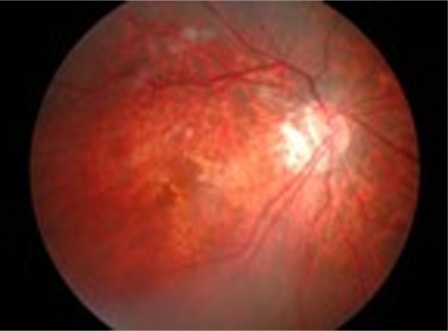
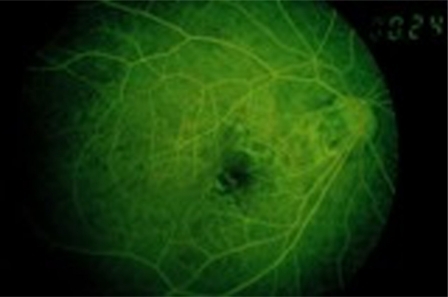
His right vision on presentation was 6/30 which was not improved with pinhole and 6/6 for the left eye. The anterior segments revealed a clear cornea bilaterally, and a deep anterior chamber with intraocular pressures of 14 mmHg (right eye) and 16 mmHg (left eye). There were no vitreous cells and no vitreous hemorrhage. The right fundus showed chorioretinal atrophy at the posterior pole, with a subretinal hemorrhage at the inferotemporal fovea (). The optic disc was tilted, with inferotemporal peripapillary atrophy. The macula of the left eye showed myopic maculopathy with a chorioretinal atrophy appearance and without subretinal hemorrhage. Fundus fluorescein angiography of the right eye revealed a hyperfluorescent area at the fovea which was increasing in intensity and size (). A diagnosis of CNV secondary to myopia of the right eye was made. Due to logistical problems, optical coherence tomography was not performed in this patient.
Figure 1 The right fundus showed subretinal hemorrhage at inferotemporal fovea and tilted disc with inferotemporal peripapillary atrophy.
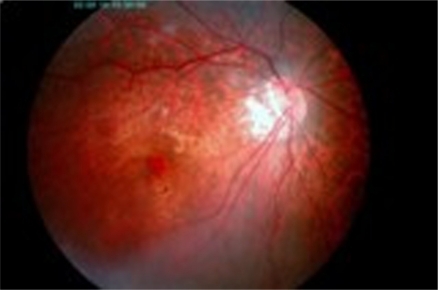
Figure 2 The FFA of the right eye showed the presence of choroidal neovascularisation with the evidence of hyperfluoresence area at the fovea which increased in intensity and size throughout the phase.
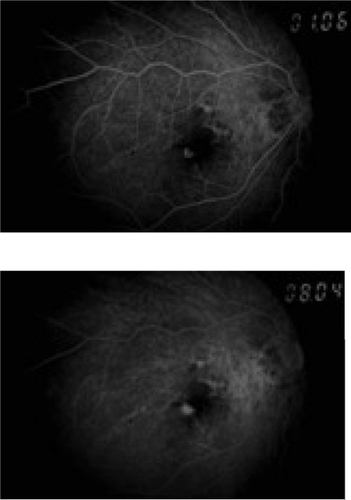
An intravitreal injection of ranibizumab 0.05 mL (Lucentis®, Novartis, Basel, Switzerland) was given to the right eye. The patient was treated with moxifloxacin ophthalmic solution 0.5% (Alcon®, Alcon Laboratories Inc, Fort Worth, TX) at 4-hourly intervals for 3 days following the procedure. After 1 week of intravitreal ranibizumab injections, visual acuity improved to 6/15 with pinhole. The intraocular pressure was normal, and no complications, such as intraocular infection, retinal tear, or vitreous hemorrhage was seen. The fundus showed that the subretinal hemorrhage had become less dense and was reducing in size (). At 10-week follow-up, visual acuity improved to 6/7.5 with glasses, and repeat fundus fluorescein angiography showed the absence of CNV (). Follow-up at 6 months showed that visual acuity had normalized to 6/6 with glasses, which was maintained up to 12 months after treatment. The right fundus showed no subretinal hemorrhage with no new lesions.
Discussion
By definition, pathological myopia is also known as high, degenerative, or malignant myopia which is characterized as excessive elongation of axial length from 25.5 to 26.5 mm and refractive errors of at least −5.0 or −7.5 D.Citation2
The risk factors for development of pathological myopia depend on ethnicity and genetics, whereas increased intraocular pressure and retinal degeneration, such as lacquer cracks and patchy atrophy, are risk factors for developing CNV secondary to pathological myopia. The prevalence is higher in Asian populations, whereas six autosomal dominant loci and one X-linked recessive locus have been reported for pathological myopia.Citation2 In this case, the patient’s spherical equivalent refractive error was −5.0 D which is one of the risk factors for developing CNV secondary to myopia.
Several treatments have been proposed to treat myopic CNV, including laser photocoagulation,Citation2,Citation3 surgical removal of CNV,Citation4,Citation5 macular translocation,Citation4,Citation6 and photodynamic therapy with and without intravitreal triamcinolone acetonide,Citation1,Citation7,Citation8 but the most appropriate treatment has not yet been established.
Laser photocoagulation seemed to cause more harm than no treatment in an early study, but subsequent studies showed more efficacy in preventing irreversible visual loss. Laser photocoagulation should be considered in extrafoveal cases compared with juxtafoveal due to long-term expansion of laser scar causing decrease in visual acuity.Citation2
Photodynamic therapy with verteporfin is the other treatment option for subfoveal CNV in pathological myopia. In one study, a group treated with photodynamic therapy had more stable visual acuity compared with a placebo group.Citation1
There are two main surgical procedures for CNV pathological myopia, ie, macular translocation and surgical removal. Hamelin et al compared these surgical procedures, but no significant difference was found in postoperative best corrected visual acuity. However, recurrence of CNV was more common after surgical removal and the incidence of retinal detachment was similar in both groups.Citation4
Recent reports have suggested that antivascular endothelial growth factor could be a new modality for the management of pathological myopia.Citation9–Citation13 Ranibizumab has been found to be effective in the treatment of exudative age-related macular degeneration.Citation14 CNV due to pathological myopia is not associated with significant retinal edema, so the retinal barriers might be less disturbed in comparison with age-related macular degeneration, and thus a possible higher penetration ability of the small ranibizumab molecule might be a significant advantage.Citation11
summarizes seven reported studies and one case report of intravitreal ranibizumab for myopic CNV in the literature from 2008 to 2011.Citation11,Citation15–Citation21 Based on these studies, intravitreal ranibizumab appears to be effective for the treatment of myopic CNV, resulting in functional and anatomic improvements. A study done by Lai et alCitation19 and a case report by Kumaran et alCitation18 showed that a single injection of intravitreal ranibizumab is effective for the treatment of myopic choroidal neovascularization as was presented in this patient. The number of intravitreal ranibizumab injections required depends on patient characteristics, including location of myopic CNV and prior treatment.Citation15 In conclusion, a single injection of ranibizumab showed improvement in this patient with myopic CNV.
Table 1 Reported studies and case report of intravitreal ranibizumab for myopic choroidal neovascularization
Disclosure
The authors report no conflicts of interest in this work.
References
- BlinderKJBlumenkranzMSBresslerNMVerteporfin therapy of subfoveal choroidal neovascularization in pathologic myopia: 2-year results of a randomized clinical trial – VIP report no. 3Ophthalmology200311066767312689884
- SoubraneGChoroidal neovascularisation in pathologic myopia: recent developments in diagnosis and treatmentSurv Opthalmol200853121138
- SecretanMKuhnDSoubraneGCoscasGLong term visual outcome of choroidal neovascularisation in pathologic myopia: natural history and laser treatmentEur J Ophthalmol199773073169457451
- HamelinNGlacet-BernardABrindeauCMimounGCoscasGSoubraneGSurgical treatment of subfoveal neovascularisation in myopia: macular translocation vs surgical removalAm J Ophthalmol200213353053611931787
- Ruiz-MorenoJMde la VegaCSurgical removal of subfoveal choroidal neovascularisation in highly myopic patientsBr J Ophthalmol2001851041104311520751
- MateoCMorenoJRosalesGTwo-year results of macular translocation with sclera infolding in myopic choroidal neovascularisationSemin Ophthalmol200419294215590532
- MonteroJARuiz-MorenoJMCombined photodynamic therapy and intravitreal triamcinolone injection for the treatment of choroidal neovascularisation secondary to pathological myopia: a pilot studyBr J Ophthalmol20079113113317244656
- ChanWMLaiTYYLiuDTLLamDSCIntravitreal bevacizumab (Avastin) for myopia choroidal neovascularisation: six-month results of a prospective pilot studyOphthalmology20071142190219617599414
- NguyenQDShahSTatlipinarSDoDVAndenEVCampochiaroPABevacizumab suppresses choroidal neovascularisation caused by pathological myopiaBr J Ophthalmol2005891368137016170134
- YamamotoIRogersAHReichelEYatesPADukerJSIntravitreal bevacizumab (Avastin) as treatment for subfoveal choroidal neovascularisation secondary to pathological myopiaBr J Ophthalmol20079115716016870653
- KonstantinidisLMantelIPournarasJACZografosLAmbresinAIntravitreal ranibizumab (Lucentis®) for the treatment of myopic choroidal neovascularisationGraefes Arch Clin Exp Ophthalmol200924731131819043731
- IkunoYSayanagiKSogaKIntravitreal bevacizumab for choroidal neovascularisation attributable to pathological myopia: one year resultsAm J Ophthalmol20091479410018774550
- VoykovBGeliskenFInhoffenWVoelkerMBartz-SchmidtKUZiemssenFBevacizumab for choroidal neovascularisation secondary to pathologic myopia: is there a decline of the treatment efficacy after 2 years?Graefes Arch Clin Exp Ophthalmol201024854355020111971
- RosenfeldPJBrownDMHeierJSRanibizumab for neovascular age-related macular degenerationN Engl J Med20063551419143117021318
- Calvo-GonzalezCReche-FrutosJDonateJFernandez-PerezCGarcia-FeijooJIntravitreal ranibizumab for myopic choroidal neovascularization: factors predictive of visual outcome and need for retreatmentAm J Ophthalmol201115152955421236413
- SilvaRMRuiz-MorenoJMRosaPIntravitreal ranibizumab for myopic choroidal neovascularization: 12-month resultsRetina20103040741220094007
- MonesJMAmselemLSerranoAGarciaMHijanoMIntravitreal ranibizumab for choroidal neovascularization secondary to pathologic myopia: 12-month resultsEye2009231275128019478826
- KumaranNSimDATufailALong-term remission of myopic choroidal neovascular membrane after treatment with ranibizumab: A case reportJ Med Case Reports200938419946560
- LaiTYChanWMLiuDTLamDSIntravitreal ranibizumab for the primary treatment of choroidal neovascularization secondary to pathologic myopiaRetina20092975075619357555
- TorronCEgeaCFerrerERuizOHonrubiaFMRanibizumab as treatment for myopic choroidal neovascularizationArch Soc Esp Oftalmol200984507514 Spanish.19902395
- SilvaRMRuiz-MorenoJMNascimentoJShort-term efficacy and safety of intravitreal ranibizumab for myopic choroidal neovascularizationRetina2008281117112318788102