Abstract
Background
The purpose of this study was to evaluate pars plana vitrectomy (PPV) with phacoemulsification in the vitreous cavity for treatment of complete posterior dislocation of the lens without any damage to the lens capsule.
Methods
We evaluated factors such as cause of dislocation, scleral fixation of an intraocular lens (IOL), preoperative and postoperative visual acuity, corneal endothelial cell density, and intraoperative and postoperative complications.
Results
Displacement in the eleven eyes studied was mostly caused by ocular trauma and was idiopathic (four eyes each). Scleral fixation of the IOL was performed in seven of the eyes during first-time PPV. Visual acuity was improved in two eyes, unchanged in eight eyes, and worse in one eye. Mean corneal endothelial cell density was 2485 cells/mm2 preoperatively and 2301 cells/mm2 postoperatively. No significant differences were seen before and after the surgeries (P = 0.15, paired t-test). Intraoperative complications included retinal detachment and suprachoroidal hemorrhage in one eye each. The most common postoperative complication was transient ocular hypertension, which occurred in three eyes. IOL dislocation and vitreous incarceration of the anterior chamber in one eye required a second operation, while retinal detachment in one eye required a third operation.
Conclusion
When treating a completely dislocated lens, prevention of retinal detachment which subsequently can affect the visual prognosis is the most important factor to be addressed after PPV with intravitreal phacoemulsification.
Introduction
Extraction of a completely dislocated lens with an intact capsule from the vitreous cavity has long been a difficult surgical problem.Citation1 When the dislocated lens is retained in the vitreous cavity, this can lead to poor visual acuity, along with inflammation, corneal edema, and glaucoma.Citation2
Development of techniques and instruments in the vitreoretinal surgery field has led to improved surgical results along with a decreased number of complications. As a result, more active surgical treatments are now being undertaken in some vitreoretinal diseases, such as treatments for a completely dislocated lens with an intact capsule in the vitreous cavity. This is very different from the very conservative approaches that would have been attempted in such cases in the past.Citation3 Pars plana vitrectomy (PPV) with lensectomy techniques are well suited to cases in which there is complete dislocation of the lens with an intact capsule.Citation4
However, despite current advances, manipulation of the lens intravitreally still involves a potentially high risk of retinal injury.Citation1 The use of perfluorocarbon liquid has made PPV safer, because it allows the lens to float over the retinal surface, thereby avoiding retinal injury.Citation5 In this study, we retrospectively evaluated outcomes in patients with a completely dislocated lens who underwent PPV and intravitreal phacoemulsification using perfluorocarbon liquid.
Methods and materials
We reviewed the medical records of eleven patients (eleven eyes, nine men, two women) who underwent PPV between September 2006 and November 2010 as treatment for a completely dislocated lens with an intact anterior and posterior capsule. All surgeries were performed by one experienced surgeon at the Dokkyo Medical University Koshigaya Hospital. All patients were followed for a minimum of 3 months (mean follow-up 13.1 ± 13.5 months). The mean age of the patients was 64.1 ± 9.5 years.
A standard 20-gauge three-port PPV was performed by removing enough vitreous and posterior hyaloid membrane to free the dislocated lens. After 0.1–0.3 cc of perfluorocarbon liquid was injected at the posterior pole, the lens was lifted and subsequently positioned in the vitreous cavity. Phacoemulsification was performed, with great care taken to ensure the ultrasound energy was in the middle of the vitreous cavity. Small lens flakes attached to the retina were removed using a silicone tip connected to the flute needle.
In cases where scleral fixation of the intraocular lens (IOL) was performed, a foldable acrylic IOL (VA-65BB or YA-65BB, Hoya Corporation, Tokyo, Japan) was used. The surgical method for scleral fixation of the IOL has been reported previously.Citation6 Briefly, after a 3.5 mm superior scleral tunnel incision was made, triangular scleral flaps were created opposite to each other at the 8 o’clock and 2 o’clock positions, with the IOL then sutured using an ab externo approach.Citation6
Decimal visual acuity data were converted into logarithm of the minimum angle of resolution (logMAR) values, and a change of 0.0.2 logMAR was judged as improvement or worsening of vision. Hand motion was converted into a decimal visual acuity of 0.002.
Intraoperative and postoperative complications were defined as complications that occurred during first-time PPV. Visual acuity and corneal endothelial cell density were measured for three months or longer postoperatively in cases that required second or third surgical interventions due to intraoperative or postoperative complications. Transient ocular hypertension was defined as a pressure over 25 mmHg, while transient ocular hypotension was defined as a pressure under 5 mmHg. “Transient” was used to mean a period of time that could range from a few days to 2 weeks at most.
Parameters examined in this study included the cause of dislocation, scleral fixation of the IOL, preoperative and postoperative visual acuity, preoperative and postoperative corneal endothelial cell density, and intraoperative and postoperative complications.
Statistical analysis
A paired t-test was used to compare preoperative and postoperative corneal endothelial cell densities. P values less than 0.05 were considered to be statistically significant.
Results
Causes of dislocation
Lens dislocation was caused by ocular trauma in four eyes, was idiopathic in four eyes, and was as a result of coloboma, laser iridotomy for acute primary angle closure, and Marfan syndrome in one eye each.
Scleral fixation of IOL
Of the eleven eyes studied, scleral fixation of the IOL was performed in seven eyes, and in four eyes was not performed during first-time PPV. Of the four eyes in which scleral fixation of the IOL was not performed during first-time PPV, it was performed as a secondary procedure in two eyes, despite being initially planned to have been performed during first-time PPV, but retinal detachment had occurred because of intraoperative complications during the first-time procedure. Scleral fixation of the IOL was therefore performed as a second procedure. In the remaining eye, a prior decision had been made to perform scleral fixation of the IOL as a second procedure. The other two eyes remained aphakic.
Preoperative and postoperative visual acuity
The initial decimal visual acuity ranged from hand motion to a visual acuity of 1.2, and logMAR values ranged from 3.699 to −0.079. Final decimal visual acuity ranged from 0.04 to 1.2, while the logMAR values ranged from 1.398 to −0.079. When both the initial and final visual acuities were compared as logMAR values, visual acuity improved in two eyes, was unchanged in eight eyes, and worsened in one eye. The reason for the worsening in the one eye was due to retinal detachment, with this postoperative complication requiring the patient to undergo a third procedure.
Preoperative and postoperative corneal endothelial cell density
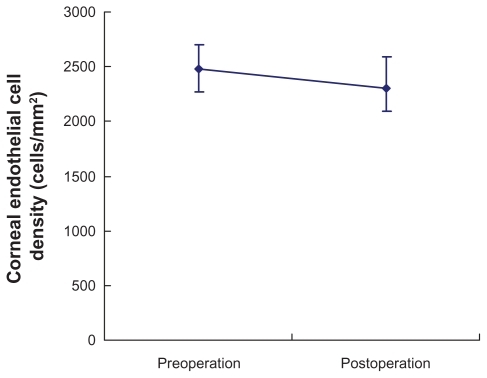
shows preoperative and postoperative corneal endothelial cell densities. The mean preoperative corneal endothelial cell density was 2485 ± 423 (range 1294–3012) cells/mm2 while the postoperative corneal endothelial cell density was 2301 ± 576 (range 1139–3194) cells/mm2. No significant differences were seen between the eyes before and after the surgeries (P = 0.15, paired t-test).
Intraoperative and postoperative complications
Intraoperative complications included retinal detachment and suprachoroidal hemorrhage in one eye each. Postoperative complications included transient ocular hypertension in three eyes, IOL dislocation in two eyes, and retinal detachment, transient ocular hypotension, vitreous hemorrhage, chronic ocular hypertension, iris capture, and vitreous incarceration of the anterior chamber in one eye each. Because there was some overlap between cases, we counted the total number of eyes.
Due to IOL dislocation and vitreous incarceration of the anterior chamber in one eye, a second operation was required. In one eye, retinal detachment required the patient to undergo a third procedure. Chronic ocular hypertension noted in one eye has required ongoing administration of a beta-blocker. The patient’s ocular hypertension is now under control and is maintained at 21 mmHg.
Discussion
Problems affecting postoperative visual acuity are considered to be serious complications. In our eleven cases, retinal detachment after surgery was the most serious complication noted. After such surgery, the wounds need to be carefully observed. Also, vitreous strand incarceration and iatrogenic retinal tears that occur during surgery need to be correctly treated in order to avoid retinal detachment. When the procedure is properly performed, intraoperative complications, such as retinal detachments and suprachoroidal hemorrhage, can be prevented from affecting postoperative visual acuity. Postoperative ocular hypertension was reported as a complication resulting from use of perfluorocarbon liquid.Citation7–Citation9 Transient ocular hypertension in three eyes and chronic ocular hypertension in one eye were observed in the current study. Therefore, care should be taken when using perfluorocarbon liquid to minimize the risk of loss of postoperative visual acuity.
The most common complications in our patients resulted from ocular trauma or were idiopathic. In similar studies performed by Seo et al,Citation3 Oh and Smiddy,Citation4 and Ogawa et al,Citation10 it was reported that ocular trauma was the most common complication. When coloboma is present, the patient must be carefully observed because lens subluxation may be seen.Citation11 With bullous keratopathy, although it is a known complication after laser iridotomy,Citation12 only a few cases with lens dislocation after laser iridotomy have been reported.Citation3,Citation13,Citation14 Laser iridotomy can be easily performed on an outpatient basis, provided the indication for the procedure is based on a careful and thorough examination of the patient. Recently, there have been some reports supporting phacoemulsification as the first choice for acute angle closureCitation15,Citation16 and for angle closure glaucoma.Citation16
The use of perfluorocarbon liquid has made it possible to remove a surgically dislocated hard lens safely.Citation5 Because perfluorocarbon liquid has a high density, it pools posteriorly at the optic nerve, and due to its low viscosity, a smallgauge extrusion needle can be used during the procedure. Furthermore, removal of the perfluorocarbon liquid can be easily accomplished. However, when only using perfluorocarbon liquid during the procedure, it is not uncommon for lens movement to occur. Thus, the phacoemulsification technique in the vitreous cavity can be prone to difficulties when this liquid is used.
One problem that can also be encountered during the phacoemulsification procedure is small lens fragments that normally occur becoming trapped between the retina and the perfluorocarbon liquid. Removal of these fragments can be both dangerous and time-consuming. When viscoelastic is used with the perfluorocarbon liquid, these problems decrease and it is easier and safer to perform the surgery.Citation1 Although this method was not employed in any of the eleven patients in the current study, it has now been adopted at our institution and will now be used to prevent these types of problems from occurring in the future.
Although our PPV with the phacoemulsification method in the vitreous cavityCitation17,Citation18 does not require any enlargement of the scleral limbal wound, it is possible that a retinal tear or vitreous hemorrhage could occur due to the ultrasound energy present.Citation19 Other reported methods that can be used in such cases involve lifting the lens into the anterior chamber, with removal then performed via a scleral limbal wound.Citation5,Citation10 Although this method is both rapid and safe, it requires the scleral limbal wound to be enlarged. Because of this, we decided not to use this method in the current study, because it could potentially cause corectopia or iris prolapse.
We were unable to determine whether scleral fixation of an IOL during first-time PPV should be recommended in all cases. In our study, two aphakic patients elected not to undergo further surgery, so their aphakia is still present. In both cases, the patients now wear soft contact lenses for their hypermetropia. If these patients do change their minds, we will perform scleral fixation of the IOL procedure in the future.
To the best of our knowledge, there have been no previously reported studies measuring preoperative and postoperative corneal endothelial cell density. Thus, the current data will help to refine and improve the success of this technique in the future. Our results indicate that preoperative and postoperative corneal endothelial cell densities were not affected by our surgical technique. Therefore, when an experienced surgeon performs this type of surgery, the technique can be considered to be safe and one that does not cause any harm to the corneal endothelium.
To prevent inflammation or secondary glaucoma,Citation2 it is necessary to remove a lens that has undergone complete posterior dislocation. However, in some cases, retinal detachment can occur after surgery, which could affect the visual prognosis. These complications can occur due to insufficient cutting of the vitreous body or insufficient repair of the iatrogenic retinal tear during the surgical procedure. Further studies in larger numbers of patients will need to be undertaken in the future in order to clarify the nature of these complications.
Disclosure
The authors report no conflicts of interest in this work.
References
- Dalma-WeiszhauszJFranco-CardenasVDalmaAA modified technique for extracting a dislocated lens with perfluorocarbon liquids and viscoelasticsOphthalmic Surg Lasers Imaging20104157257420795578
- HuangHMKaoMLKuoHKVisual results and complications after trans pars plana vitrectomy and lensectomy for lens dislocationChang Gung Med J20042742943515455543
- SeoMSYoonKCLeeCHPhacofragmentation for the treatment of a completely posterior dislocation of the total crystalline lensKorean J Ophthalmol200216323612162515
- OhJSmiddyWEPars plana lensectomy combined with pars plana vitrectomy for dislocated cataractJ Cataract Refract Surg2010361189119420610099
- ShapiroMJResnickKIKimSHManagement of the dislocated crystalline lens with a perfluorocarbon liquidAm J Ophthalmol19911124014051928242
- MutohTMatsumotoYChikudaMScleral fixation of foldable acrylic intraocular lenses in aphakic post-vitrectomy eyesClin Ophthalmol20105172121311652
- YoshidaKKiryuJKitaMPhacoemulsification of dislocated lens and suture fixation of intraocular lens using a perfluorocarbon liquidJpn J Ophthalmol1998424714759886738
- SirimaharajMBalachandranCChanWCVitrectomy with short term postoperative tamponade using perfluorocarbon liquid for giant retinal tearsBr J Ophthalmol2005891176117916113376
- StolbaUBinderSVelikayMUse of perfluorocarbon liquids in proliferative vitreoretinopathy: results and complicationsBr J Ophthalmol199579110611108562545
- OgawaRYoshizawaTBabaESurgical management and visual outcome for dislocated lensesJapanese Review of Clinical Ophthalmology200599551553
- JardónJIzquierdoNJColoboma and CHARGE association in Puerto RicoBol Asoc Med P R20091013941 Spanish19954100
- AngLPHigashiharaHSotozonoCArgon laser iridotomy-induced bullous keratopathy a growing problem in JapanBr J Ophthalmol2007911613161517567658
- MelamedSBarraquerEEpsteinDLNeodymium: YAG laser iridotomy as a possible contribution to lens dislocationAnn Ophthalmol1986182812823490815
- SeongMKimMJTchahHArgon laser iridotomy as a possible cause of anterior dislocation of a crystalline lensJ Cataract Refract Surg20093519019219101444
- MineMOkamotoMYukawaEThe criteria of surgery for acute primary angle closure in Nara Medical UniversityFolia Japonica de Ophthalmologica Clinica2010311631166
- LachkarYAcute angle closure and angle closure glaucoma: phacoemulsification as first-line treatmentJ Fr Ophtalmol201033273278 French20347182
- Ruiz-MorenoJMBarileSMonteroJAPhacoemulsification in the vitreous cavity for retained nuclear lens fragmentsEur J Ophthalmol200616404516496244
- Soliman MahdyMEidMZShalabyKAIntravitreal phacoemulsification with pars plana vitrectomy for management of posteriorly dislocated nucleus or lens fragmentsEur J Ophthalmol20102011511919882507
- BoppSel-HifnawiESBornfeldNRetinal lesions after transvitreal use of ultrasoundFortschr Ophthalmol199188442445 [German.]1757028