Abstract
Electrophysiological and morphological findings were studied in a case of acute zonal occult outer retinopathy (AZOOR) showing abnormal pattern visual evoked potentials (VEPs) at the onset and significant functional recovery in the natural course. A 21-year-old woman presented with acute onset of photopsia and a large scotoma in the right eye of 2 weeks duration. Her visual acuity was 20/20 in both eyes with no ophthalmoscopic and fluorescein angiographic abnormalities. However, a relative afferent pupillary defect and an enlarged blind spot were found in the right eye. The pattern VEPs were severely reduced when the right eye was stimulated. The amplitudes of both rod and cone full-field electroretinographics (ERGs) were reduced in the right eye. The amplitudes of the multifocal ERGs were reduced in the area of the enlarged blind spot. Irregularities in the inner segment/outer segment (IS/OS) line of the photoreceptors were observed over the nasal fovea by optical coherence tomography (OCT). The patient was followed without treatment. The enlarged blind spot disappeared in 3 months after the onset. At 5 months, reappearance of the IS/OS line was detected by OCT. At 6 months, the P100 recovered to normal values. At 1 year, the reduced full-field ERGs were almost normal size and the multifocal ERGs in the area corresponding to the enlarged blind spot were also improved. ERG findings are crucial for differentiating AZOOR from retrobulbar neuritis, especially in patients with abnormal pattern VEPs. The pattern VEPs, full-field ERGs, multifocal ERGs, and OCT images can be abnormal in the early phase of AZOOR, but they can all improve during the natural course.
Introduction
Acute zonal occult outer retinopathy (AZOOR), first reported in 1993 by Gass,Citation1 is characterized by an acute onset of photopsia, scotoma, minimal funduscopic changes, and electroretinographic (ERG) abnormalities affecting one or both eyes. The presence of abnormal ERGs is important for the diagnosis of AZOOR, and the ERG findings suggest a dysfunction of the photoreceptors.Citation1–Citation5 Recent optical coherence tomographic (OCT) studies have shown morphological alterations of the photoreceptors.Citation6–Citation9
Although a viral or autoimmune etiology has been suspected, no cause is readily identifiable in this group of generally healthy patients. Some patients with AZOOR have been misdiagnosed with optic nerve disorders because they had an afferent pupillary defect, a scotoma, and no obvious fundus abnormalities.Citation1–Citation3
It has been reported that the natural course of AZOOR is varied,Citation1–Citation3 although there is still no known treatment. There are few detailed reports about AZOOR patients who showed subjective and objective improvements in their visual function. We report a case of AZOOR, showing abnormal pattern visual evoked potentials (VEPs) at the onset and significant functional recovery in the natural course.
Case report
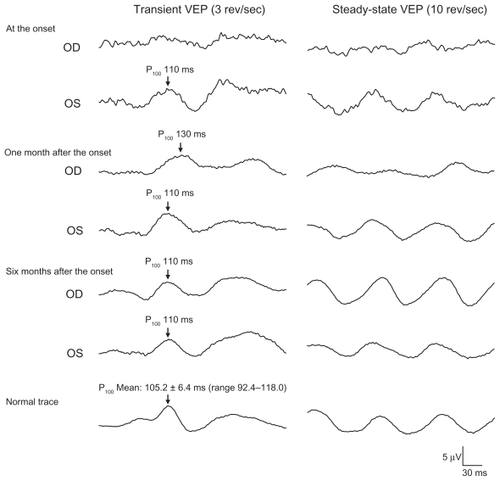
A healthy 21-year-old woman reported that she had a sudden onset of photopsia and a large scotoma in the right eye on August 14, 2008. She visited her ophthalmologist on August 15, and the initial examination showed no abnormalities of the fundus in both eyes but a large scotoma was detected by static perimetry in the right eye. She was referred to us for further examination on August 29. She reported that she had no systemic problems and was not taking any medications. Her best-corrected visual acuity was 20/20 bilaterally, and the refractive error was −9.5 diopters in the right eye and −8.5 diopters in the left eye. However, she had a relatively afferent pupillary defect in the right eye. The results of ophthalmoscopy (), fluorescein angiography (), blood screening, and brain magnetic resonance imaging (MRI) were within normal limits. Static perimetry with the Humphrey field analyzer showed an enlarged blind spot in the right eye (). The pattern VEPs elicited by transient and steady-state stimuli to the right eye were severely reduced (). She was suspected of having retrobulbar neuritis at this point of time. VEPs were recorded by Nihon Kohden MEB-2200 Neuropack (Tokyo, Japan) with the active electrode placed at Oz. The reference electrode was located at the right earlobe and the ground electrode at the left earlobe. The visual stimulus was a black and white check board pattern generated on a television monitor. The check size was 20 minutes of arc. The contrast was 80%, and the mean luminance was kept at 50 cd/m2. The stimulus field of the pattern was 7 × 11 degrees. The pattern was reversed at three reversals per second for transient VEP, and 10 reversals per second for steady-state VEP. The electrodes were connected to a preamplifier with a bandpass of 1 to 100 Hz, and for each measurement, 100 responses were averaged. The patient fixed on a point in the center of the pattern monocularly from an observing distance of 170 cm, with an undilated pupil under full refractive correction.
Figure 1 Fundus photograph, fluorescein angiographic image, Humphrey static perimetry, and Optical coherence tomography (OCT) of the right eye. (a) Fundus photograph at the onset showing that the retina was normal. (b) Fluorescein angiography at the onset showing normal vascular pattern and no leakage. (c) Humphrey static perimetry at the onset showing enlarged blind spot (30-2 strategy MD −21.97 dB). (d) Humphrey static perimetry 3 months after the onset showing marginally enlarged blind spot (30-2 strategy MD −1.90 dB). (e) OCT image at the onset showing irregular inner segment/outer segment (IS/OS) line over the nasal fovea. (f) OCT image 5 months after the onset showing reappearance of IS/OS line over the nasal fovea.
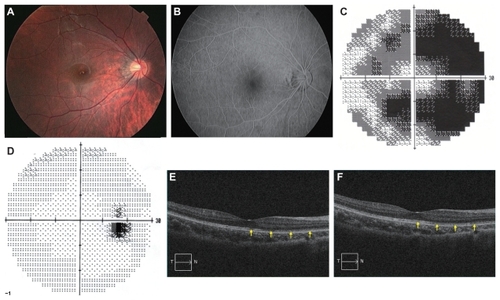
Figure 2 Pattern visual evoked potentials (VEPs). At the onset, pattern VEPs are severely reduced in the right eye. One month after the onset, the P100 component of the pattern VEPs has a prolonged latency of 130 milliseconds. Six months after the onset, the P100 recovers to 110 milliseconds.
To eliminate the possibility that the patient had AZOOR, full-field ERGs and multifocal ERGs were recorded. The amplitudes of the rod and cone responses in the right eye were reduced to about 50% of those in the left eye (). The multifocal ERGs recorded from the area of the enlarged blind spot were reduced (). Irregularities in the inner segment/outer segment (IS/OS) line of the photoreceptors over the nasal fovea were observed by Fourier-domain OCT (HD-OCT; Carl Zeiss Meditec, Oberkochen, Germany) (). Serum anti-recoverin was negative. She was diagnosed with AZOOR from these findings. Full-field ERGs were recorded by Nihon Kohden Neuropack 9400, following dilation of the pupils and 30 minutes of dark adaptation. A contact lens electrode was used. The reference electrode was placed at the forehead and the ground electrode at the earlobe. The flash strength was 0.01 cd s m−2 for rod response, 80.0 cd s m−2 for combined rod–cone response and oscillatory potentials, and 3.0 cd s m−2 for cone response and flicker. Light adaptation and background luminance was 25 cd/m2. Responses were amplified with a bandpass of 0.2 to 1000 Hz. First-order Kernel multifocal ERGs were recorded with the Visual Evoked Response Imaging System (VERIS science 4.1; EDI, San Mateo, CA). A Burian-Allen bipolar contact lens electrode was used. The visual stimuli consisted of 61 and 103 hexagonal elements with an overall subtense of approximately 60°. The luminance of each hexagon was independently modulated between black (3.5 cd/m2) and white (138.0 cd/m2) according to a binary M-sequence at 75 Hz. The surround luminance was 70.8 cd/m2.
Figure 3 Full-field electroretinographics (ERGs). At the onset, the amplitudes of the rod and cone responses in the right eye are reduced to about 50% of those in the left eye. At the 1 year follow-up examination, the reduced full-field ERGs are improved to be approximately the same amplitudes as those from the left eye.
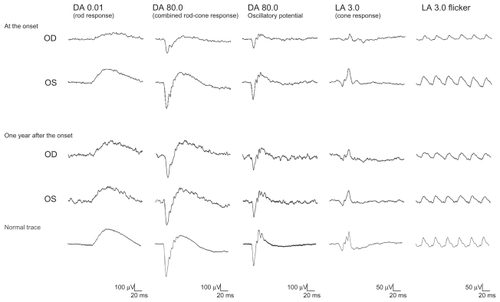
Figure 4 Multifocal electroretinographics (ERGs). At the onset, the multifocal ERGs are reduced in the right eye. At the 1 year follow-up examination, the multifocal ERGs have improved but are still reduced especially from the temporal retina. Shorter duration protocol with 61 hexagonal elements was used for the latest recording, because acceptable responses to 103 hexagonal elements could not be obtained due to fatigue of the patient during the recording.
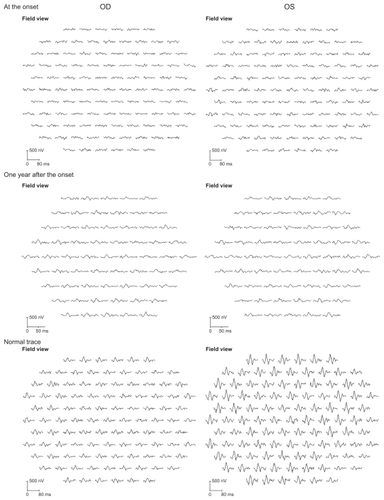
The patient was followed without any treatment, and more comprehensive examinations were made in her follow-up examinations. The enlarged blind spot in static perimetry disappeared 3 months after our initial examination (). The P100 component of the pattern VEPs had a prolonged latency of 130 milliseconds 1 month later. At 6 months, the P100 recovered to 110 milliseconds (mean: 105.2 ± 6.4 milliseconds; normal range: 92.4–118.0 milliseconds) (). At 5 months, reappearance of the IS/OS line was detected by OCT over the nasal fovea (). At the 1 year follow-up examination, her best-corrected visual acuity was 20/20 in both eyes. The reduced full-field ERGs were improved to be approximately the same amplitudes as those from the left eye (). A mild improvement of the reduced multifocal ERGs was also observed (). The other findings had not worsened.
Discussion
In 1993, Gass introduced AZOOR to describe a previously unrecognized syndrome occurring predominantly in young females. In his original series of 13 patients, affected individuals typically presented with acute onset of photopsia, scotoma, minimal funduscopic changes, and ERG abnormalities affecting one or both eyes.Citation1 The presence of abnormal ERGs is essential for the diagnosis of AZOOR. Gass et al reported that electroretinographic amplitudes were depressed in all 90 affected eyes.Citation2 Jacobson et al reported 24 patients with AZOOR showing abnormal ERGs. Interocular asymmetry was a prominent feature.Citation4 Francis et al reported that electrophysiology demonstrated a consistent pattern of dysfunction both at the photoreceptor/retinal pigment epithelial complex but also at inner retinal levels in 28 patients with AZOOR.Citation5
Our case presented with a sudden onset of photopsia and a large scotoma in the right eye at the onset. The normal fundus, large scotoma, and the afferent pupillary defect made us suspect retrobulbar neuritis at first. But the absence of retrobulbar pain at rest or on eye movement, which is a common symptom in retrobulbar neuritis,Citation10 and the presence of photopsia, which is a typical symptom of AZOOR,Citation1–Citation5 made us suspect AZOOR at the same time. Further examinations were taken to make a definite diagnosis.
Our patient had an extinguished P100 component of the pattern VEPs at the onset, although her visual acuity was 20/20. Fluorescein angiography showed normal vascular pattern and no leakage. MRI showed no changes in the optic nerve. Strikingly, in full-field ERGs, the amplitudes of both rod and cone responses were reduced in the right eye. The amplitudes of the multifocal ERGs were reduced in the area of the enlarged blind spot. She was diagnosed with AZOOR because of ERG abnormalities. Serum anti-recoverin was negative, which was helpful to reduce the possibility that she had cancer-associated retinopathy. Irregularities in the IS/OS line of the photoreceptors were observed by OCT. The findings of OCT helped make the diagnosis.
It is known that a delayed latency of the pattern VEPs is not a specific sign of optic neuropathy because it is also found in eyes with retinal diseases.Citation11–Citation15 However, there were few reports of AZOOR showing abnormal VEPs. Gass reported that 80% of AZOOR patients had normal VEPs, and only one patient with poor visual acuity of 20/70 in the right eye and 20/300 in the left eye had abnormal VEPs.Citation1 Takai et al reported five AZOOR patients who had no delay in the VEPs.Citation7 Patients of AZOOR who had normal pattern VEPs with normal visual acuity have been reported.Citation16,Citation17 Although significant abnormalities of the VEPs have rarely been reported in eyes with AZOOR, our case showed that AZOOR can be associated with significantly delayed VEPs. The mechanisms for the altered pattern VEPs without a decrease in the visual acuity was not determined in our case. The delayed VEP might be explained by reduced macular sensitivities. However, the possibility of inner retina or optic nerve involvement cannot be completely excluded.
Gass et al reported that in the presence of normal fundi, the most frequent misdiagnosis was retrobulbar neuritis, and there was a median of 17 months delay in the diagnosis of AZOOR.Citation2 In addition to the afferent pupillary defect, abnormal VEPs could mislead the ophthalmologist to a diagnosis of optic nerve disease. This case report serves to alert the ophthalmologist to consider the diagnosis of AZOOR and consider recording ERGs in individuals presenting with unexplained scotoma, particularly where photopsia are a prominent feature.
It has been reported that the natural course of AZOOR is varied.Citation2,Citation3 Gass et al reported that visual field loss stabilized within 6 months in 37 patients (72%), progressed stepwise in two patients (4%), and partly improved in 12 patients (24%).Citation2 Degenerations of the photoreceptor outer segment have been detected by OCT at the convalescent stage.Citation6–Citation9 There are few detailed reports about the clinical course of AZOOR patients who show some recovery. Yasuda et al reported a case with mild improvement of the multifocal ERGs, but morphological changes were not demonstrated in the report.Citation18 Spaide et al reported restoration of the IS/OS line in the areas of improved visual field, but electrophysiological alterations of these patients were not demonstrated in the report.Citation9
Our case had a recovery of retinal function as assessed by not only visual field tests, but also full-field ERGs and multifocal ERGs. Morphological improvements were confirmed by OCT in parallel. Although it is difficult to compare the order or degree of improvement of each parameter, our case demonstrated that subjective and objective functional recovery could occur in the eyes with AZOOR. The irregular IS/OS line at the onset might have reflected incomplete loss of photoreceptor. In this case, the incomplete impairment of photoreceptor might have been associated with the visual function recovery. Further studies are needed.
Conclusion
We reported a case of AZOOR showing profoundly abnormal pattern VEPs at the onset, and significant functional recovery in the natural course. ERG findings are crucial for differentiating AZOOR from retrobulbar neuritis, especially in patients with abnormal pattern VEPs. The pattern VEPs, full-field ERGs, multifocal ERGs, and OCT images can be abnormal in the early phase of AZOOR, but they can all improve during the natural course. Further studies and long-term follow-up are needed to better understand this disorder, and these findings will hopefully reduce the number of misdiagnoses and unnecessary treatments.
Disclosure
The authors report no conflicts of interest in this work.
References
- GassJDMAcute zonal occult outer retinopathyJ Clin Neuroophthalmol199313279978340485
- GassJDAgarwalAScottIUAcute zonal occult outer retinopathy: a long-term follow-up studyAm J Ophthalmol2002134332933912208243
- MonsonDMSmithJRAcute zonal occult outer retinopathySurv ophthalmol2011561233521056448
- JacobsonSGMoralesDSSunXKPattern of retinal dysfunction in acute zonal occult outer retinopathyOphthalmology19951028118711989097746
- FrancisPJMarinescuAFitzkeFWBirdACHolderGEAcute zonal occult outer retinopathy: towards a set of diagnostic criteriaBr J Ophthalmol2005891707315615750
- FujiwaraTImamuraYGiovinazzoVJSpaideRFFundus autofluorescence and optical coherence tomographic findings in acute zonal occult outer retinopathyRetina20103081206121620661173
- TakaiYIshikoSKagokawaHFukuiKTakahashiAYoshidaAMorphological study of acute zonal occult outer retinopathy by multiplanar optical coherence tomographyActa Ophthalmol200987440841818778338
- LiDKishiSLoss of photoreceptor outer segment in acute zonal occult outer retinopathyArch Ophthalmol200712591194120017846358
- SpaideRFKoizumiHFreundKBPhotoreceptor outer segment abnormalities as a cause of blind spot enlargement in acute zonal occult outer retinopathy-complex diseasesAm J Ophthalmol2008146111112018439564
- Optic Neuritis Study GroupThe clinical profile of acute optic neuritis. Experience of the Optic Neuritis Treatment TrialArch Ophthalmol199110912167316781841573
- LennerstrandGDelayed visual evoked cortical potentials in retinal diseaseActa Ophthalmol19826044975047158314
- BassSJShermanJBodis-WollnerINathSVisual evoked potentials in macular diseaseInvest Ophthalmol Vis Sci1985268107110744019098
- NegishiCTakasohMFujimotoNTsuyamaYAdachi-UsamiEVisual evoked potentials in relation to visual acuity in macular diseaseActa
- ShimadaYAdachi-UsamiEMurayamaKHow are macular changes reflected in pattern visually evoked cortical potentials?Acta Ophthalmol Scand19977532772809253974
- HolderGEElectrophysiological assessment of optic nerve diseaseEye (Lond)200418111133114315534599
- LeeAGPragerTCAcute zonal occult outer retinopathyActa Ophthalmol Scand199674193958689493
- AraiMNao-iNSawadaAHayashidaTMultifocal electroretinogram indicates visual field loss in acute zonal occult outer retinopathyAm J Ophthalmol199812634664699744389
- YasudaKShimuraMNoroMNakazawaMTamaiMClinical course of acute retinal zonal occult outer retinopathy in visual field and multifocal electroretinogramBr J Ophthalmol19998391089109010636684