Abstract
Some patients with acute zonal occult outer retinopathy (AZOOR) show symptomatic acute visual impairment in one eye only, but electrophysiological abnormalities in both eyes. A 46-year-old female who had noticed paracentral scotoma of her right eye six months previously was referred to our hospital. At initial examination, her best-corrected visual acuity was 0.7 in the right eye and 1.2 in the left. Whereas the full-field rod electroretinogram (ERG) was normal in both eyes, the cone response was nonrecordable in the right eye and showed a significant decrease in amplitude in the left eye. The 30 Hz flicker ERG showed similar results. Multifocal ERG was nonrecordable in the right eye and showed a residual response in only the central part of the left. Fourteen months after the first visit, the patient presented complaining of acute visual acuity loss in the left eye. Visual acuity in her left eye had decreased to 0.01. The multifocal ERG was nonrecordable. Although the patient chose oral prednisolone therapy, only limited recovery was observed in the patient. Even if only the ERG shows changes and there are no other symptoms, ophthalmologists should continue observation in view of the possibility of an acute exacerbation.
Introduction
Acute zonal occult outer retinopathy (AZOOR) is a syndrome characterized by rapid loss of one or more zones of outer retinal function.Citation1 Patients are predominantly young women and frequently present with photopsia and visual field defects. Electrophysiological testing is useful for diagnosis. Some patients with AZOOR show symptomatic acute visual impairment in one eye, but electrophysiological abnormalities in both eyes.Citation2,Citation3 However, to the best of the authors’ knowledge, there have been no follow-up reports of the electrophysiologically affected asymptomatic eye, and it is not well established whether the functionally affected eye will progress and the patient will develop clinical symptoms.
Case report
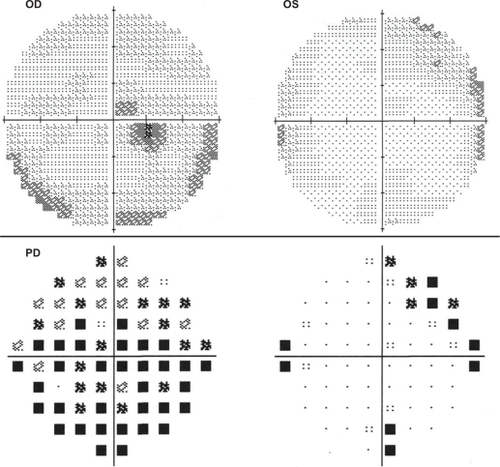
A 46-year-old female who had noticed paracentral scotoma of her right eye six months previously was referred to our hospital. At initial examination, her best-corrected visual acuity was 0.7 in the right eye and 1.2 in the left. Intraocular pressure, anterior segment, ocular media and fundus, including fluorescein angiographic examination showed no abnormalities (). The cone response was nonrecordable in the right eye and showed a significant decrease in amplitude in the left eye. The 30 Hz flicker ERG showed similar results, and the maximal response was abnormal, with reduced a-wave and b-wave amplitudes as well as oscillatory potentials (). Multifocal ERG was nonrecordable in the right eye and showed a residual response only in the central part of the left. Static perimetry (full threshold 10-2 Humphrey visual field examination) showed relative central scotoma of the right eye (). The clinical findings were compatible with a diagnosis of AZOOR,Citation1 and careful observation was recommended.
Figure 1 Fundus photograph and fluorescein angiography appears normal (left panels). Electroretinogram shows marked loss of cone function in both eyes (right panels).
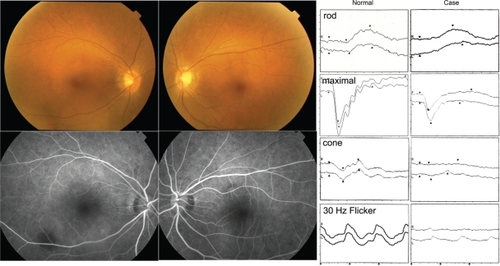
Figure 2 Static perimetry (full threshold 10-2 Humphrey visual field examination) shows central scotoma of right eye.
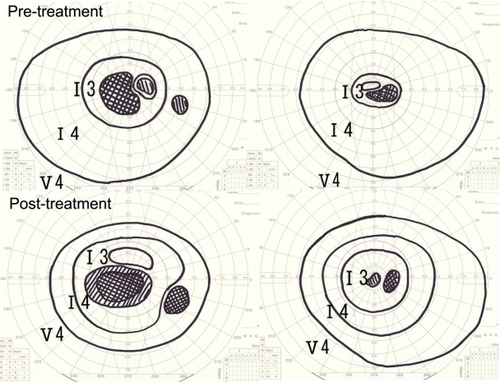
Fourteen months after the first visit, the patient presented complaining of acute visual acuity loss in the left eye. Visual acuity in her left eye had decreased to 0.01, while the right eye was 0.7. A full-field ERG showed cone function impairment. The residual response in the multifocal ERG in the central part was nonrecordable. The patient was informed that there is no established treatment for AZOOR and that oral prednisolone has been tested with moderate efficacy according to case reports.Citation2 The patient opted for oral prednisolone therapy 30 mg daily. One month thereafter, limited recovery was observed in the patient as revealed by Goldmann perimetry ().
Discussion
Gass et alCitation2 and Francis et alCitation3 reported that AZOOR was present in one eye in 61% and 46% cases, respectively, at the first visit, 61% and 14% of patients with unilateral AZOOR subsequently developed symptoms suggestive of AZOOR in the fellow eye, and electrophysiological abnormalities were observed in both eyes in 25% and 18% of patients at their first visit, respectively. However, there was no mention of whether such patients subsequently developed clinical symptoms. In the current case, there was a discrepancy in the results between the ERG and static visual field testing in the left eye at initial presentation. It is possible that kinetic visual field testing could have revealed a visual field abnormality at the initial visit. As this case report shows, when a patient is diagnosed with AZOOR, it should be determined whether AZOOR is unilateral or bilateral in consideration of ERG results. Even if only the ERG shows changes and there are no other symptoms, ophthalmologists should continue observation in view of the possibility of an acute exacerbation.
Disclosure
The authors report no conflicts of interest in this work.
References
- GassJDStereoscopic Atlas of Macular Diseases: Diagnosis and Treatment4th edSt. Louis, MOMosby1996
- GassJDAgarwalAScottIUAcute zonal occult outer retinopathy: a long-term follow-up studyAm J Ophthalmol200213432933912208243
- FrancisPJMarinescuAFitzkeFWBirdACHolderGEAcute zonal occult outer retinopathy: towards a set of diagnostic criteriaBr J Ophthalmol200589707315615750