Abstract
A 39-year-old male with decreased visual acuity and extensive macular hemorrhage and edema secondary to a hemiretinal vein occlusion was treated with multiple intravitreal injections of bevacizumab 1.25 mg every four to six weeks for over one year. Treatment outcomes were assessed by visual acuity and Cirrus spectral domain optical coherence tomography. Treatment resulted in ongoing visual and anatomic improvement, with resolution at the last visit.
Introduction
Retinal vein occlusions are a frequent cause of visual loss, and approximately 16 million adults worldwide are affected.Citation1 Macular edema and retinal ischemia are the primary sources of visual impairment in these settings. Retinal vein occlusions can be classified as branch retinal vein occlusion, hemiretinal vein occlusion, and central retinal vein occlusion depending on the occlusion site. Risk factors for the development of a retinal vein occlusion include diabetes mellitus, hypertension, hyperlipidemia, atherosclerosis, glaucoma, and smoking.Citation2
The clinical course and visual prognosis of retinal vein occlusions can be highly variable. Clinical trials have evaluated treatment modalities including observation, laser, intravitreal triamcinolone, and anti-vascular endothelial growth factor (VEGF) therapy. Intravitreal bevacizumab, an anti-VEGF drug, has been used to treat a variety of vitreoretinal diseases. Rosenfeld et al first injected intravitreal bevacizumab for macular edema from a central retinal vein occlusion and also reported long-term improvements in visual acuity and optical coherence tomography (OCT, Carl Zeiss Meditec, Jena, Germany) being sustained through one year with treatment.Citation3,Citation4 More recently, randomized, controlled clinical trials have evaluated the frequency of treatment with anti-VEGF therapy for macular edema secondary to retinal vein occlusions to help determine optimal long-term therapeutic strategies.Citation5,Citation6
We describe a case of an acute hemiretinal vein occlusion with confluent macular hemorrhage and persistent macular edema for which early and continued treatment with intravitreal bevacizumab facilitated functional and structural improvement and resolution.
Case report
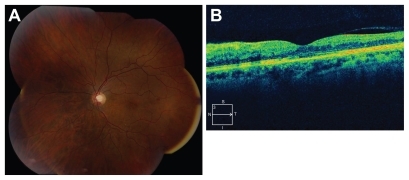
A 39-year-old male with no significant past medical history presented with decreased vision in the left eye for six weeks. The patient was initially evaluated at an outside facility and diagnosed with a hemiretinal vein occlusion in the left eye. Medical and hypercoaguable laboratory evaluation was unremarkable, and the patient was referred to the Bascom Palmer Eye Institute. Best corrected visual acuity was 20/20 in the right eye and 20/80 in the left eye. Intraocular pressures were 18 and 17 mmHg in the right and left eye, respectively. External and slit lamp examinations were unremarkable. Fundus evaluation of the right eye was within normal limits, and the left eye demonstrated extensive, confluent intraretinal hemorrhages extending inferiorly from the nerve and involving the macula (). OCT of the right eye was unremarkable, and the left eye demonstrated intraretinal and subretinal fluid with a central retinal thickness of 696 microns (). Fluorescein angiography of the left eye showed blockage from hemorrhage, with subsequent limited assessment of perfusion and late hyperfluorescence (). The patient was treated with 1.25 mg of intravitreal bevacizumab at this visit. At one month, visual acuity in the left eye improved to 20/60 and OCT demonstrated improved fluid with a central retinal thickness of 534 microns (). The patient was retreated with intravitreal bevacizumab. At the subsequent four-week visit, the patient was symptomatic with a decline in visual acuity to 20/70 and increased fluid was present on OCT (). The patient was treated with a third intravitreal bevacizumab injection. Six weeks later, visual acuity improved to 20/40, the confluent macular hemorrhage had improved, and OCT showed reduced fluid (). Treatment was continued at this visit, and at six-week intervals due to persistent visual symptoms and macular edema and hemorrhage. The patient received a total of nine intravitreal bevacizumab injections. At recent follow-up, six weeks after the last injection, visual acuity improved to 20/25 and fundus evaluation showed minimal intraretinal hemorrhages (). OCT demonstrated a preserved foveal contour with resolved fluid and subfoveal inner and outer segment (IS/OS) disruption (). The patient was observed.
Figure 1 Initial presentation. Best corrected visual acuity 20/80. (A) Color fundus photograph demonstrates extensive, confluent inferior retinal hemorrhages with macular involvement. (B) Optical coherence tomography demonstrates intraretinal cysts and subretinal fluid. Central foveal thickness 696 microns (central 1 mm subfield). (C–E) Fluorescein angiography. (C) Early: 28 seconds, (D) 2.37 minutes, and (E) Late: 9.42 minutes, extensive blockage from hemorrhage and late hyperfluorescence.
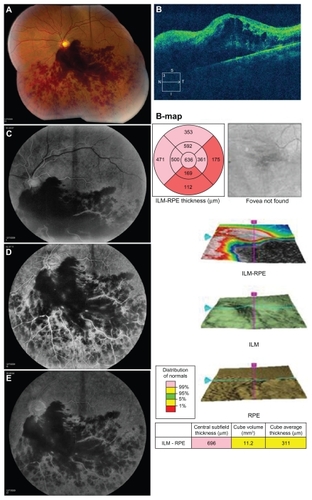
Figure 2 Cirrus spectral domain optical coherence tomography progression. (A) Best corrected visual acuity 20/60, improved intraretinal and subretinal fluid (central foveal thickness 534 microns) after initial intravitreal bevacizumab injection four weeks earlier. (B) Best corrected visual acuity 20/70, central foveal thickness 682 microns. (C) Color fundus photograph six weeks after third intravitreal bevacizumab injection. Improved confluent macular hemorrhage. (D) Best corrected visual acuity 20/40, central foveal thickness 473 microns, corresponding optical coherence tomography to (C) visit.
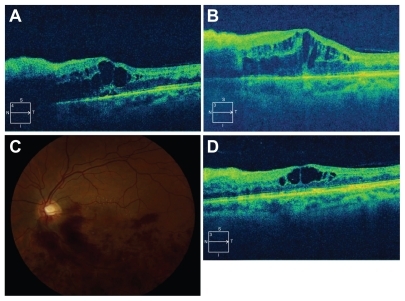
Figure 3 Recent follow-up. Best corrected visual acuity 20/25. (A) Color fundus photograph demonstrates resolution of majority of confluent hemorrhages. (B) Optical coherence tomography demonstrates resolved fluid (central foveal thickness 261 microns) and presence of subfoveal inner and outer segment disruption.
Discussion
Macular edema is often a frequent cause of vision loss in patients with retinal vein occlusions. Since hemiretinal vein occlusions share etiologic and clinical features of both branch and central retinal vein occlusions, treatment strategies are often extrapolated from studies pertaining to these conditions. The Branch Vein Occlusion Study (BVOS) reported that laser photocoagulation is beneficial for perfused macular edema with <20/40 vision for at least three months, but the visual recovery is both slow and limited.Citation7 After three years of follow- up, 63% of laser treated eyes improved ≥2 lines of vision compared with 36% of control eyes.Citation7 The average improvement of visual acuity was only 1.3 lines from the baseline in the laser-treated group, and 40% of eyes had a visual acuity of ≤20/40 and 12% had a visual acuity of <20/200.Citation7 Based on the Central Retinal Vein Occlusion Study (CVOS) results, grid laser photocoagulation is not a recommended therapy for improving visual acuity from macular edema secondary to central retinal vein occlusion.Citation8 The Standard Care versus Corticosteroid for Retinal Vein Occlusion (SCORE) study group concluded that 1 mg intravitreal triamcinolone, with retreatment criteria as utilized in the trial, was superior to observation and could be considered up to one year for central retinal vein occlusion-related macular edema, and was equivalent to macular grid laser treatment for macular edema from a branch retinal vein occlusion ( and ).Citation9,Citation10 This was the first trial to demonstrate efficacy of a treatment for macular edema secondary to a central retinal vein occlusion. Further, the Ozurdex Geneva Study Group investigated the efficacy of a dexamethasone intravitreal implant, Ozurdex®, for the treatment of macular edema due to retinal vein occlusions. The proportion of eyes achieving at least a 15-letter improvement from baseline was significantly greater in the 0.35 mg and 0.7 mg implant groups from day 30; but this effect was not maintained by day 180, when no statistically significant difference from the sham group was observed ( and ).Citation11 However, associated risks of intraocular pressure elevation and cataracts with steroid treatment were present in both studies.
Table 1 Branch retinal vein occlusion summary dataCitation5,Citation9,Citation10
Table 2 Central retinal vein occlusion summary dataCitation6,Citation9,Citation10
Additional therapeutic modalities have also been explored in the treatment of macular edema from retinal vein occlusions. VEGF-A has been implicated as a major factor for increased vascular permeability, and elevated intravitreal VEGF levels have been reported to be significantly increased after retinal vein occlusions and correlate with the degree of macular edema.Citation12 VEGF also stimulates endothelial cell hypertrophy, which reduces capillary lumen size and may lead to retinal ischemia.Citation13 Bevacizumab is a full length monoclonal humanized antibody to all active isoforms of vascular endothelial growth factor, and is frequently used in clinical practice to treat macular edema from retinal vein occlusions. Recently, clinical studies have demonstrated beneficial effects of monthly intravitreal treatment with an anti-VEGF agent, ranibizumab, on both macular edema and visual acuity in patients with retinal vein occlusions. Data from the Phase III Study of the Efficacy and Safety of Ranibizumab Injection in Patients with Macular Edema Secondary to Branch Retinal Vein Occlusion (BRAVO) and the Study of the Efficacy and Safety of Ranibizumab Injection in Patients with Macular Edema Secondary to Central Retinal Vein Occlusion (CRUISE) demonstrated that a higher proportion of patients treated with ranibizumab 0.3 mg and 0.5 mg experienced significant improvements in visual acuity and central foveal thickness at six months following monthly dosing compared with patients who received sham injections (, , and ).Citation5,Citation6 These improvements were sustained at 12 months in both trials in the ranibizumab groups, following six months of as-needed treatment ().Citation5,Citation6 Overall, results from these studies demonstrate that regular, monthly anti-VEGF treatment for retinal vein occlusions provided improvements superior to previous treatment modalities.
In the current report, a young patient with decreased visual acuity and extensive macular hemorrhage with macular edema demonstrated an initial and ongoing functional and structural improvement with continued intravitreal bevacizumab treatment. Initial visual acuity, younger age, duration of retinal vein occlusion, baseline central retinal thickness, response to the first injection, and integrity of the photoreceptors have all been reported to be predictive factors for response to anti-VEGF therapy.Citation14,Citation15 Although this patient returned to his baseline vision, the presence of subfoveal IS/OS disruption likely secondary to chronic macular edema and/or initial hemorrhage may also indicate that ongoing treatment with intravitreal bevacizumab prevented further destructive changes and a subsequent decline in vision. The Patterns and Trends Survey by the American Society of Retina Specialists showed that approximately 50% of respondents use intravitreal bevacizumab as first-line therapy for retinal vein occlusions.Citation16 The favorable treatment outcome for this patient lends support to the clinical impression that regular injections of intravitreal bevacizumab are an effective primary treatment strategy for persistent macular edema and hemorrhage from a hemiretinal vein occlusion.
Acknowledgment
This research was supported by an unrestricted award from Research to Prevent Blindness (P30EY014801).
Disclosure
The authors report no conflicts of interest in this work.
References
- RogersSMcIntoshRLCheungNThe prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia and AustraliaOphthalmology201011731331920022117
- HayrehSSZimmermanBMcCarthyMJPodhajskyPSystemic diseases associated with various types of retinal vein occlusionAm J Ophthalmology20011316177
- RosenfeldPJFungAEPuliafitoCAOptical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for macular edema from central retinal vein occlusionOphthalmic Surg Lasers Imaging20053633633916156153
- GregoriNZGaitanJRosenfeldPJLong-term safety and efficacy of intravitreal bevacizumab (avastin) for the management of central retinal vein occlusionRetina2008281325133719430392
- CampochiaroPAHeierJSFeinerLRanibizumab for macular edema following branch retinal vein occlusion: six month primary end point results of a Phase III studyOphthalmology20101171102111220398941
- BrownDMCampochiaroPASinghRPRanibizumab for macular edema following central retinal vein occlusion: six-month primary end points results of a phase III studyOphthalmology20101171124113320381871
- The Branch Vein Occlusion Study GroupArgon laser photocoagulation for macular edema in the branch vein occlusionAm J Ophthalmology198498271282
- The Central Vein Occlusion Study GroupEvaluation of grid pattern photocoagulation for macular edema in central vein occlusion. The Central Vein Occlusion Study Group M reportOphthalmology1995102142514339097788
- The SCORE Study Research GroupSCORE study report 5: a randomized trial to compare the efficacy and safety of intravitreal injection(s) of triamcinolone acetonide with standard care to treat vision loss associated with macular edema secondary to central retinal vein occlusionArch Ophthalmol20091271101111419752419
- The SCORE Study Research GroupSCORE study report 6: a randomized trial to compare the efficacy and safety of intravitreal injection(s) of triamcinolone acetonide with standard care to treat vision loss associated with macular edema secondary to branch retinal vein occlusionArch Ophthalmol20091271115112819752420
- HallerJABandelloFBelfortRRandomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusionOphthalmology20101171134114620417567
- FunkMKriechbaumKPragerFIntraocular concentrations of growth factors and cytokines in retina vein occlusion and the effect of therapy with bevacizumabInvest Ophthalmol Vis Sci2009501025103219060280
- FigueroaMSContrerasINovalSResults of bevacizumab as the primary treatment for retinal vein occlusionBr J Ophthalmol2010941052105620679089
- HochAERuppensteinMAchTDithmarSOCT patterns of macular edema and response to bevacizumab therapy in retinal vein occlusionGraefes Arch Clin Exp Ophthalmol20102481567157220596719
- Wolf-SchnurrbuschUEGhanemRRothenbuehlerSPPredictors for short term visual outcome after anti-VEGF therapy of macular edema due to central retinal vein occlusionInvest Ophthalmol Vis Sci2011523334333721087958
- American Society of Retina Specialists Annual Preferences and Trends Survey2009 Available at: http://www.asrs.orgAccessed September 12, 2011