Abstract
Purpose
To compare outcomes in visual acuity, refractive error, higher-order aberrations (HOAs), contrast sensitivity, and dry eye in patients undergoing laser in situ keratomileusis (LASIK) using wavefront (WF) guided VISX CustomVue and WF optimized WaveLight Allegretto platforms.
Methods
In this randomized, prospective, single-masked, fellow eye study, LASIK was performed on 44 eyes (22 patients), with one eye randomized to WaveLight Allegretto, and the fellow eye receiving VISX CustomVue. Postoperative outcome measures at 3 months included uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), refractive error, root-mean-square (RMS) value of total and grouped HOAs, contrast sensitivity, and Schirmers testing.
Results
Mean values for UDVA (logMAR) were −0.067 ± 0.087 and −0.073 ± 0.092 in the WF optimized and WF guided groups, respectively (P = 0.909). UDVA of 20/20 or better was achieved in 91% of eyes undergoing LASIK with both lasers while UDVA of 20/15 or better was achieved in 64% of eyes using the Allegretto platform, and 59% of eyes using VISX CustomVue (P = 1.000). In the WF optimized group, total HOA increased 4% (P = 0.012), coma increased 11% (P = 0.065), and spherical aberration increased 19% (P = 0.214), while trefoil decreased 5% (P = 0.490). In the WF guided group, total HOA RMS decreased 9% (P = 0.126), coma decreased 18% (P = 0.144), spherical aberration decreased 27% (P = 0.713) and trefoil decreased 19% (P = 0.660). One patient lost one line of CDVA secondary to residual irregular astigmatism.
Conclusion
Both the WaveLight Allegretto and the VISX CustomVue platforms had equal visual and safety outcomes. Most wavefront optimized HOA values trended upward, with a statistically significant increase in total HOA RMS. Eyes treated with the WF guided platform showed a decreasing trend in HOA values.
Introduction
Conventional laser refractive surgery platforms are capable of correcting lower-order aberrations, such as hyperopia, myopia, and astigmatism. Higher-order aberrations (HOAs), such as coma, spherical aberration, and trefoil, are induced by, and remain uncorrected in, traditional laser in situ keratomileusis (LASIK) surgery.Citation1,Citation2
Although conventional LASIK surgery is mostly accurate, abundant research has shown reoperation rates for primary myopic keratorefractive surgery are between 5.5% and 19.2%.Citation3–Citation9 When HOAs cannot be corrected, image quality may suffer.Citation1,Citation2,Citation10–Citation13 The HOAs call for more advanced optical measurements and more sophisticated laser algorithms. These laser algorithms are found in wavefront (WF) based treatments, which have been shown to diminish induced HOAs compared to traditional LASIK, and increase predictability of visual outcomes.Citation14–Citation18 As WF based methods have evolved rapidly over the years, an important question is whether there are significant differences in the induced HOAs and visual outcomes between specific WF guided and WF optimized platforms used in LASIK.
To date, multiple studies have compared WF guided and WF optimized platforms in LASIK surgery.Citation19–Citation24 The data shows varied results, with some studies suggesting an advantage to WF guided platforms,Citation19,Citation22–Citation24 and others showing no significant difference between the two platforms.Citation20,Citation21 In this prospective, randomized, fellow eye study, we compared WF guided VISX CustomVue platform (Abbott Medical Optics [AMO], Santa Ana, CA) with WF optimized WaveLight Allegretto platform (Alcon, Inc, Hüenberg, Switzerland) in the same patient undergoing LASIK, with respect to visual acuity, refractive error, HOAs, contrast sensitivity, and dry eyes.
Patients and methods
This prospective, single masked, randomized, fellow eye study evaluated and compared the outcomes of LASIK performed on 44 eyes (22 patients) using the VISX CustomVue laser system and the WaveLight Allegretto laser system. Patients were recruited and enrolled at the John A Moran Eye Center, Department of Ophthalmology and Visual Science, University of Utah, between December 2010 and July 2011. All patients were over the age of 21.
The University of Utah Hospital Institutional Review Board approved the research protocol in accordance with the tenets of the Declaration of Helsinki. All patients provided informed consent after they received an explanation of the procedure, including all risks and benefits. All patients had a preoperative discussion of relevant medical history, including history of herpetic eye disease and family history of keratoconus.
Patients were excluded if they had a history of clinically significant lens opacity, previous corneal or intraocular surgery, thin corneas, keratoconus, unstable refraction, amblyopia, or autoimmune disease; were pregnant or breastfeeding; or were on immunosuppressive therapy. Patients desiring monovision were not included in the study.
Eligible patients were scheduled for bilateral LASIK and correction for distance in both eyes. The patients were randomly assigned (Research Randomizer software – Urbaniak, www.randomizer.org) to treatment in one eye with the WaveLight Allegretto system (WF optimized group), which utilizes the WaveLight® Allegretto 400 Hz Wave® Eye-Q Laser. The fellow eye was assigned treatment with the VISX CustomVue™ STAR S4 IR™ Excimer Laser with Active-Track™ iris registration (WF guided group). The patients were blinded as to which laser was used for treatment in each eye. No patient had LASIK enhancement at any time during the study.
Soft contact lenses were discontinued 2 weeks before screening and rigid gas permeable contact lenses were discontinued 6 weeks before screening. All patients had a preoperative examination including manifest refraction (MRX) and cycloplegic refraction, uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), tonometry, slitlamp examination, and dilated fundus evaluation. Corneal topography and thickness were measured using the Pentacam (OCULUS Optikgeräte GmbH, Wetzlar, Germany) and Humphrey Atlas (Carl Zeiss Meditec, Inc, Jena, Germany) systems. Pupil size was measured in the dark using the Colvard pupillometer (Oasis Medical, Inc, Glendora, CA). Contrast sensitivity was performed using the VectorVision CSV-1000 (Dayton, OH) chart in controlled mesopic (70 lux) conditions at three, six, twelve, and 18 cycles per degree. Schirmers testing evaluation for dry eye was measured in millimeters with topical anesthetic after 5 minutes. MRX and WF measurements were repeated on two separate visits to ensure refractive stability.
All eyes received five preoperative wavefront analyses using the VISX CustomVue WaveScan aberrometer v 3.62 (Fourier) (AMO), without pharmacologic intervention, under mesopic conditions, with a minimum pupil diameter of 6.0 mm. The emmetropic correction target was based on MRX, topography, and wavefront analysis for the WF guided group. For the WF optimized group, emmetropic correction target was based on topography and MRX. Iris registration was obtained for eyes receiving WF guided treatment. Previously established Moran Laser Center WF guided LASIK nomograms were followed for both the Allegretto and the CustomVue treatments. The nomograms were generated with Datagraph-med refractive outcomes software (v 3.20a; Ingenieurbüro Pieger GmbH, Wendelstein, Germany) using a minimum of 50 eyes for each wavefront platform with a minimum follow-up of 3 months.
All LASIK flaps were created with an iFS™ Advanced Femtosecond Laser (AMO) at 150 kHz in a raster pattern with bed energy of 1.15 μJ, side cut energy of 2.00 μJ, and pocket enabled. Flaps were created with an intended thickness of 110 μm, diameter of 8.4 to 9.0 mm, superior hinge angle of 55°, and a side cut angle of 70°. If the 8.0 mm maximum intended ablation diameter exceeded the flap diameter, the hinge and flap were shielded during ablation. All surgeries were performed by Majid Moshirfar and Mark D Mifflin.
Postoperatively, each eye received one drop of gatifloxacin 0.3% (Allergan Inc, Irvine, CA) and prednisolone acetate 1% (Allergan, Inc). The prednisolone acetate was continued hourly on postoperative day 1, and then four times daily for 6 additional days. The gatifloxacin was continued four times daily for 1 week.
Patients were seen and data was collected at 1 day, 1 week, and 1 and 3 months after surgery. UDVA and CDVA were tested using a standard Snellen eye chart. Visual acuity was recorded in both Snellen notation and logarithm of the minimum angle of resolution (logMAR) format. Evaluation of contrast sensitivity, dry eye, and HOAs were performed. HOAs including total HOA root mean square (RMS), coma Z(3,1), trefoil Z(3,3), and spherical aberration Z(4,0), were measured using the WaveScan aberrometer. Undilated scans of both eyes were taken at 3 months postoperatively regardless of the wavefront platform used for treatment. Subjective outcomes were recorded using the Quality of Life Impact of Refractive Correction (QIRC) instrument. The ratings from the QIRC were interpreted using the guidelines set by Pesudovs et al.Citation25
Statistics
After the study was completed, the results were compiled and the data unmasked for statistical analysis. MRX, refractive error, visual acuity, contrast sensitivity, HOA values for coma, trefoil, and sphere, and HOA RMS wavefront aberration values were treated as continuous variables and analyzed for significance by using a paired Student’s t-test. A P value of 0.05 or less was considered statistically significant. Data analysis was performed using Microsoft Excel (Microsoft Corp, Redmond, WA).
Results
22 patients (44 eyes) with 3 months of postoperative care were evaluated in this study. The sample population consisted of 15 women and seven men with a mean age of 31.2 years ± 6.3 standard deviation (SD) (range 23 to 53 years). Baseline data showed no significant differences in preoperative CDVA or refractive error ().
Table 1 Preoperative group comparisons
Visual acuity
UDVA and CDVA were not statistically different between the groups at 1 or 3 months (). Postoperatively, 20/15 UDVA was achieved in 64% and 59% of the eyes in the WF optimized and WF guided groups, respectively. Three months after surgery, 91% of the eyes in both groups achieved 20/20 UDVA (). Postoperatively, spherical equivalent and sphere measurements decreased significantly in the WF optimized group compared to the WF guided group at 1 and 3 months (P = 0.020, P = 0.017). There was no significant difference in cylinder measurements in either group before or after surgery.
Table 2 One month and three month visual acuity comparisons
Table 3 Efficacy, predictability, and safety comparison of allegretto and VISX laser platforms
Safety, efficacy, and predictability
At 1 month, 21 eyes (95%) in the WF optimized group and 18 (81%) in the WF guided group were within ± 0.50 diopters (D) of emmetropia. In addition, ten eyes (45%) in the WF optimized group and six eyes (27%) in the WF guided group were within ±0.25 D of emmetropia (P = 0.035). Although there was a significant difference in emmetropia at 1 month, this did not remain significant at 3 months ().
At 3 months, one eye (5%) in the WF optimized group lost one line of CDVA. The vision loss was attributed to residual irregular astigmatism confirmed by topography. No other eyes in the study population lost any lines of CDVA. Nine eyes (41%) in the WF optimized group maintained equal CDVA compared to twelve eyes (55%) in the WF guided group. Eleven eyes (50%) in the WF optimized group and nine eyes (41%) in the WF guided group gained one line of CDVA. One eye in both groups gained two lines (P = 1.000).
Schirmers testing
The preoperative average Schirmers test value for the WF optimized group was 19.9 mm ± 9.95 and 22.1 mm ± 9.98 for the WF guided group. At 1 month the values were 20.3 mm ± 8.52 and 21.1 mm ± 10.2 for the WF optimized group and the WF guided group, respectively. The 3 months postoperative values were 21.1 mm ± 7.83 for the WF optimized group and 20 mm ± 8.12 for the WF guided group. There was no significant difference in Schirmers testing between both groups during the study period (P ≥ 0.081).
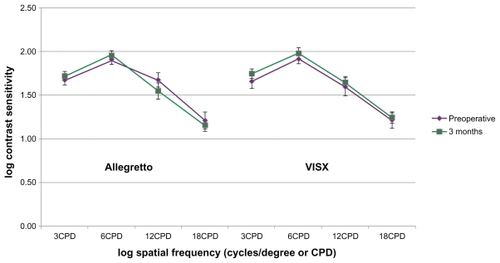
Contrast sensitivity
Contrast sensitivity did not change significantly in either group when preoperative measurements were compared to postoperative measurements (P ≥ 0.07) ().
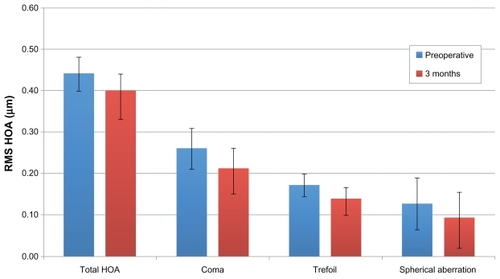
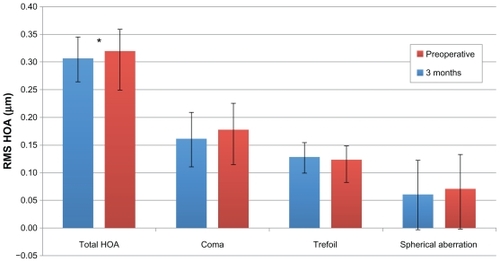
Higher-order aberrations
At 3 months postoperatively, 15 eyes (68%) in each group completed CustomVue WaveScan analysis. The only statistically significant change discovered was a 4% increase in total HOA RMS (P = 0.012) in the WF optimized group. In this group, other HOAs had nonsignificant changes, which showed the following: coma increased 11% (P = 0.065), trefoil decreased 5% (P = 0.239) and spherical aberration increased 19% (P = 0.214) (). The WF guided group showed a decreasing trend in HOA values, with total HOA RMS, coma, trefoil, and spherical aberration decreasing 9% (P = 0.126), 18% (P = 0.144), 19% (P = 0.660), and 28% (P = 0.713) respectively (). There were no significant differences in preoperative or postoperative HOA values between the WF guided or WF optimized groups.
Figure 2 Comparison of higher-order aberrations before surgery (n = 16) and 3 months postoperatively (n = 16) in the wavefront optimized platform. Total, coma, Z(3, 1), trefoil, Z(3, 3), and spherical aberration, Z(4, 0) were measured using the WaveScan at a mean diameter of 6 mm.
Abbreviation: RMS HOA, root-mean-square higher order aberration.
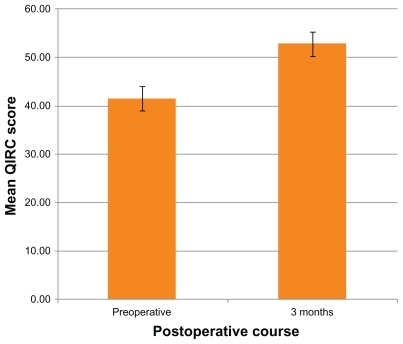
Quality of life
Mean QIRC values were obtained preoperatively and at 3 months postoperatively. Postoperative mean QIRC values at 3 months were 27% higher than preoperative values (P < 0.001) ().
Complications
No intraoperative complications occurred in the study population. One eye lost one line of CDVA in the WF optimized group. The patient had 4.00 D of astigmatism preoperatively, and the loss of vision was determined to be due to residual astigmatism with some irregularity confirmed by topography. No other eyes in the sample population lost any lines of CDVA. Complications included three eyes with nonvisually significant microstriae, one of which was slightly overcorrected. All patients with microstriae were in the −7.00 D range preoperatively. The overcorrected eye was in the WF guided group, and had a terminal spherical equivalent measuring +1.75 D. This patient remains at 20/20 UDVA. No other complications were observed.
Discussion
In a recent retrospective study comparing VISX Custom-Vue to WaveLight Allegretto platforms in LASIK surgery, Perez- Straziota et al found there were no significant differences in visual outcomes or induced HOAs.Citation20 To the best of our knowledge, we report the first prospective, randomized, single masked, fellow eye study between these lasers.
Our study supports previous comparative research that the VISX CustomVue WF guided platform and the WaveLight Allegretto WF optimized platform are effective and predictable in LASIK surgery.Citation19–Citation23,Citation26 We found a statistically significant difference in postoperative sphere and spherical equivalent in the WF optimized group. Additionally, a greater percentage of the WF optimized eyes fell within ±0.50 D of emmetropia at 1 month, but at 3 months both groups were equal. Cylinder values did not differ significantly between the wavefront platforms. There were no statistically significant differences in outcomes of UDVA, CDVA, contrast sensitivity, or Schirmers testing at 3 months postoperatively.
Comparisons of various WF guided and WF optimized platforms in LASIK have not shown a consistent advantage in reduction of HOAs in either platform.Citation19,Citation21–Citation24 In comparing two WF guided platforms, Alcon CustomCornea and VISX CustomVue, Moshirfar et al observed that both platforms led to a small increase in total HOAs.Citation26 Several authors have compared similar Allegretto WF guided and Allegretto WF optimized lasers prospectively.Citation19,Citation21,Citation23 Padmanabhan et al concluded there was no significant difference between the two modalities in terms of visual acuity or refractive outcomes, although WF guided technology induced significantly fewer HOAs.Citation19 Miraftab et al saw no significant difference of induced HOAs between either group.Citation21 Lastly, Stonecipher and Kezirian observed that WF guided treatment was more beneficial for patients with a high degree of preoperative HOA RMS.Citation23 Brint,Citation22 followed by Tran and Shah,Citation24 compared Alcon CustomCornea WF guided treatment to Allegretto WF optimized treatment. Both found a statistically significant increase in HOAs using the Allegretto platform in comparison to WF guided platform.Citation22,Citation24
We observed a similar pattern of results for HOAs after LASIK. We found a significant increase in mean total HOA RMS in the WF optimized group, along with a nonsignificant trend of decrease in trefoil, and increase in coma and spherical aberration. Conversely, the WF guided group showed a nonsignificant decreasing trend in HOA values postoperatively. Similarly, Miraftab et al found postoperative nonstatistically significant increasing trends in total HOA, C7 vertical coma, and spherical aberration, with a decreasing trend in trefoil for their WF optimized platform.Citation21 Also, Randleman et al showed a nonsignificant trend of increases in total HOA, coma, trefoil, and spherical aberration in their WF optimized LASIK study.Citation18
In regards to patient satisfaction with WF guided vs WF optimized LASIK, Yu et al showed no significant difference in objective measurements on the QIRC questionnaire.Citation27 We observed significant increases postoperatively in quality of life measures in our study population. We were unable to compare VISX CustomVue to WaveLight Allegretto using the QIRC because this survey instrument does not separate subjective results based on each eye. We administered an additional subjective survey, but the data received was limited and no conclusions could be drawn. While short subjective surveys after LASIK have allowed for conclusions in previous literature,Citation28 we believe our ten item survey instrument would benefit from a larger sample size.
Our study showed one eye that lost one line of CDVA in the WF optimized group, which was caused by a persistent irregular astigmatism, in absence of a flap complication. This postoperative outcome has been observed by Levinson et al in their study on complications leading to cornea specialist referral after LASIK.Citation29 One patient in our study experienced overcorrection in the WF guided group. Efforts to prevent overcorrection were attempted by comparing preoperative WaveScan refractions to manifest and cycloplegic refractions. The overcorrection did not impact this patient’s postoperative UDVA, which was 20/20 with no subjective complaints. We attribute this UDVA in the setting of overcorrection to the patient’s accommodation. This patient had a high degree of preoperative myopia with a high spherical equivalent, which has been correlated with LASIK overcorrection.Citation30
Limitations of the study include small sample size and short-term follow-up. We hope to continue to follow our study patients to better assess long-term outcomes. A possible limitation in comparing the VISX WF guided platform to the Allegretto WF optimized platform is that the VISX CustomVue WaveScan aberrometer is specifically designed for the VISX STAR S4 platform. One may argue that the aberrometer (WaveLight® Analyzer, Alcon, Inc, Hüenberg, Switzerland) made for use with Allegretto may have shown different results. However, authors have used a single aberrometer platform to compare various wavefront lasers with consistent results.Citation20,Citation22
Because the statistically significant differences between the platforms were small, we feel both WF optimized and WF guided platforms can provide safe and effective outcomes in LASIK. In our experience, the challenges associated with WF guided techniques included pupil size requirements, mismatch to MRX which was mostly due to over accommodation, and the timely process of uploading wavefront data. The Allegretto WaveLight Eye-Q laser functions at a higher frequency, therefore allowing faster operating times. Additionally, the Allegretto platform does not require iris registration, which can sometimes be difficult to obtain intraoperatively, and there is no issue with mismatch to MRX.
In conclusion, no significant differences were observed in regards to UDVA, CDVA, dry eye, or contrast sensitivity when comparing the WaveLight Allegretto Wave Eye-Q laser to the VISX CustomVue STAR S4 IR Excimer Laser with ActiveTrack iris registration. While the WF optimized platform showed superior outcomes for refractive measures of sphere and spherical equivalent, postoperative visual acuity was not statistically different between the study groups. Most WF optimized HOA values tended to increase, with a statistically significant increase in total HOA RMS. In contrast, there was a trend for WF guided HOA values to decrease, although not with statistical significance.
Acknowledgements
This investigation was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the Public Health Services research grant numbers UL1-RR025764 and C06-RR11234 from the National Center for Research Resources.
Disclosure
Funding was provided from the Research to Prevent Blindness Foundation (New York, NY). The authors have no financial interests in any materials or products discussed in this paper or any other disclosures.
References
- Moreno-BarriusoELlovesJMMarcosSNavarroRLlorenteLBarberoSOcular aberrations before and after myopic corneal refractive surgery: LASIK-induced changes measured with laser ray tracingInvest Ophthalmol Vis Sci2001421396140311328757
- OshikaTKlyceSDApplegateRAHowlandHCEl DanasouryMAComparison of corneal wavefront aberrations after photorefractive keratectomy and laser in situ keratomileusisAm J Ophthalmol1999127179932992
- ZadokDMaskalerisGGarciaVShahSMontesMChayetAOutcomes of retreatment after laser in situ keratomileusisOphthalmology19991062391239410599677
- GimbelHVvan WestenbruggeJAPennoEEFerensowiczMFeinermanGAChenRSimultaneous bilateral laser in situ keratomileusis: safety and efficacyOphthalmology19991061461146810442889
- FarahSGAzarDTGurdalCWongJLaser in situ keratomileusis: literature review of a developing techniqueJ Cataract Refract Surg19982498910069682123
- CondonPIMulhernMFulcherTFoley-NolanAO’KeefeMLaser intrastromal keratomileusis for high myopia and myopic astigmatismBr J Ophthalmol1997811992069135383
- KnorzMCLiermannASeiberthVSteinerHWiesingerBLaser in situ keratomileusis to correct myopia of −6.00 to −29.00 dioptersJ Refract Surg1996125755848871858
- GimbelHVBastiSKayeGBFerensowiczMExperience during the learning curve of laser in situ keratomileusisJ Cataract Refract Surg1996225425508784623
- GuellJLMullerALaser in situ keratomileusis (LASIK) for myopia from −7 to −18 dioptersJ Refract Surg1996122222288653524
- KulkamthornTSilaoJNTorresLFWavefront guided laser in situ keratomileusis in the treatment of high myopia by using the CustomVue wavefront platformCornea20082778779018650664
- ChalitaMRChavalaSXuMKruegerRRWavefront analysis in post-LASIK eyes and its correlation with visual symptoms, refraction, and topographyOphthalmology200411144745315019317
- BuhrenJMartinTKuhneAKohnenTCorrelation of aberrometry, contrast sensitivity, and subjective symptoms with quality of vision after LASIKJ Refract Surg20092555956819662912
- YamaneNMiyataKSamejimaTOcular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusisInvest Ophthalmol Vis Sci2004453986399015505046
- LiangJWilliamsDRMillerDTSupernormal vision and high-resolution retinal imaging through adaptive opticsJ Opt Soc Am A Opt Image Sci Vis199714288428929379246
- MrochenMKaemmererMSeilerTWavefront guided laser in situ keratomileusis: early results in three eyesJ Refract Surg20001611612110766379
- KohnenTBuhrenJKuhneCMirshahiAWavefront guided LASIK with the Zyoptix 3.1 system for the correction of myopia and compound myopic astigmatism with 1-year follow-up: clinical outcome and change in higher order aberrationsOphthalmology20041112175218515582071
- ZhouCChaiXYuanLHeYJinMRenQCorneal higher-order aberrations after customized aspheric ablation and conventional ablation for myopic correctionCurr Eye Res20073243143817514528
- RandlemanJBPerez-StraziotaCEHuMHWhiteAJLoftESStultingRDHigher-order aberrations after wavefront optimized photorefractive keratectomy and laser in situ keratomileusisJ Cataract Refract Surg20093526026419185240
- PadmanabhanPMrochenMBasuthkarSViswanathanDJosephRWavefront guided versus wavefront optimized laser in situ keratomileusis: contralateral comparative studyJ Cataract Refract Surg20083438939718299062
- Perez-StraziotaCERandlemanJBStultingRDVisual acuity and higher-order aberrations with wavefront guided and wavefront optimized laser in situ keratomileusisJ Cataract Refract Surg20103643744120202542
- MiraftabMSeyedianMAHashemiHWavefront guided vs wavefront optimized LASIK: a randomized clinical trial comparing contralateral eyesJ Refract Surg20102724525020839665
- BrintSFHigher order aberrations after LASIK for myopia with alcon and wavelight lasers: a prospective randomized trialJ Refract Surg200521S799S80316329383
- StonecipherKGKezirianGMWavefront optimized versus wavefront guided LASIK for myopic astigmatism with the ALLEGRETTO WAVE: three-month results of a prospective FDA trialJ Refract Surg200824S424S43018500097
- TranDBShahVHigher order aberrations comparison in fellow eyes following IntraLase LASIK with WaveLight Allegretto and CustomCornea LADARVision4000 systemsJ Refract Surg200622S961S96417124897
- PesudovsKGaramendiEElliottDBThe Quality of Life Impact of Refractive Correction (QIRC) Questionnaire: development and validationOptom Vis Sci20048176977715557851
- MoshirfarMEspandarLMeyerJJTannerJRHolzHAProspective randomized trial of wavefront guided laser in situ keratomileusis with the CustomCornea and CustomVue laser systemsJ Cataract Refract Surg2007331727173317889767
- YuJChenHWangFPatient satisfaction and visual symptoms after wavefront guided and wavefront optimized LASIK with the WaveLight platformJ Refract Surg20082447748618494340
- MoshirfarMHatchBBChangJCKurzCJEugarriosMFMifflinMDProspective, contralateral comparison of 120-mum and 90-mum LASIK flaps using the IntraLase FS60 femtosecond laserJ Refract Surg20102725125920672771
- LevinsonBARapuanoCJCohenEJHammersmithKMAyresBDLaibsonPRReferrals to the Wills Eye Institute Cornea Service after laser in situ keratomileusis: reasons for patient dissatisfactionJ Cataract Refract Surg200834323918165078
- BiebesheimerJBKangTSHuangCYYuFHamiltonDRDevelopment of an advanced nomogram for myopic astigmatic wavefront guided laser in situ keratomileusis (LASIK)Ophthalmic Surg Lasers Imaging20114224124721410091