Abstract
Purpose
Evaluation of improving near vision in presbyopic patients with low to moderate myopia with selective treatment of high-order aberrations (HOAs) using the ORK-CAM software aberrometer and a SCHWIND ESIRIS excimer laser. In this study, all HOAs except vertical coma were treated and the effect on near visual function was evaluated.
Setting
Horus Vision Correction Center, Alexandria, Egypt.
Methods
Twenty-six presbyopic patients (52 eyes) with low to moderate myopia were divided into two groups, A and B. The ORK-CAM software aberrometer was used in both groups to measure HOAs and design wavefront-guided treatment. All included eyes had total coma >0.2 μm. The Moria M2 mechanical microkeratome was used for flap making in both groups. Wavefront-guided laser-assisted in situ keratomileusis using ESIRIS laser was done for all eyes. In Group A (30 eyes) all HOAs were treated. In Group B (22 eyes) vertical coma was left untreated. Postoperative uncorrected distance visual acuity (UCVA), best corrected distance visual acuity (BCVA), uncorrected near acuity (UCNA), distance corrected near acuity (DCNA), best corrected near acuity with addition for near vision (BCNA), manifest refractive spherical equivalent (MRSE), HOAs, and contrast sensitivity for both groups were done preoperatively and at 3 months postoperatively.
Results
Mean age was 47.46 and 45.2 years for groups A and B, respectively. Mean preoperative MRSE was −2.37 and −2.87 D and mean preoperative total HOAs was 0.35 and 0.38 μm in groups A and B, respectively. There was no significant difference between groups regarding age, sex, preoperative MRSE, and preoperative total HOAs. After 3 months, there was no significant difference between groups in terms of UCVA, BCVA, MRSE, and contrast sensitivity. Analysis of postoperative HOAs showed significant difference in vertical coma between the two groups (P < 0.001). DCNA was significantly better in Group B (P < 0.01).
Conclusion
Treating low to moderate myopia with wavefront-guided ablation including selective treatment of HOAs might be very useful for improving visual functions. Treating all HOAs but the vertical coma improved uncorrected near acuity in presbyopic patients.
Keywords:
Introduction
Presbyopia is an age-related gradual, progressive loss of accommodation with recession of the near point of distinct vision over time. The eye is no longer able to either exert or maintain the accommodation required for clear near vision, necessitating the use of spectacles to enable the patient to see near distance. Intermediate vision, as well, might get affected with time.
Surgical techniques for presbyopia correction are diverse. However, they can be classified into two main approaches based on the mechanism of near vision restoration. The first approach aims at restoration of the eye’s true accommodative ability, such as anterior ciliary sclerotomy,Citation1 scleral expansion,Citation2 and accommodative intraocular lenses (IOLs).Citation3 The second approach includes restoration of helpful near vision without true gains in the eye’s accommodation by means of increasing the depth of focus, that is, pseudoaccommodation. Pseudoaccommodation can be achieved through either corneal techniques or intraocular surgery such as multifocal IOLs.Citation4,Citation5 MonovisionCitation6 is another option that can be achieved via conductive keratoplasty,Citation7 excimer laser, or monofocal IOLs.
In 2007, the authors performed an eventless wavefront-guided laser-assisted in situ keratomileusis on a 45-year-old male for moderate myopia. Postoperatively, he was able to see 20/15 unaided. Follow-up wavefront examinations revealed the accidental induction of a huge amount of vertical coma corresponding to an area of minimal ablation decentration on topography. Interestingly, this patient’s distance corrected near acuity (DCNA) improved from 20/70 preoperatively to 20/20 after the procedure.
Based on this observation and the fact that not all aberrations are harmful,Citation8 this prospective study evaluated the possibility of improving near vision in presbyopic patients with low to moderate myopia through selective treatment of high-order aberrations (HOAs).
Patients and methods
This prospective consecutive comparative randomized double-masked study was carried out at Horus Vision Correction Center in Alexandria, Egypt, from January to July 2009. Written informed consent was obtained from the patients before their participation in the study.
Patient selection
Fifty-two eyes of 26 patients, all aged >40 years, with symptoms of presbyopia were included in this study. Exclusion criteria were: <40 years old, any abnormal or suspicious patterns on corneal topography, central pachymetric measurements <500 μm, and history of chronic eye diseases. Patients with lens opacities were also excluded from the study.
Included patients all had low to moderate myopia with best corrected distance visual acuity (BCVA) of 20/20 for distance. All patients had total coma aberration of >0.2 μm at 6.0 mm pupil diameter. They were randomly divided into two groups, A and B.
In Group A, all HOAs were treated along with the sphere and cylinder. This group included 30 eyes of 15 patients (9 females and 6 males), with a mean age of 47.46 years (range 43–51 years). Mean manifest refraction spherical equivalent (MRSE) was −2.37 D (range −1.75 to −4.0 D) and mean total root mean square (RMS) value was 0.35 μm (range 0.26–0.53 μm).
In Group B, vertical coma aberrations were selectively left untreated, while all other HOAs, along with the sphere and cylinder, were treated. This group included 22 eyes of 11 patients (8 females and 3 males) with a mean age of 45.2 years (range 42–50 years). Mean MRSE was −2.87 D (range −2.0 to −4.5 D) and mean total RMS value was 0.38 μm (range 0.28–0.56 μm). shows the preoperative data of the two groups in terms of age, sex, MRSE, and root mean square RMS.
Table 1 Preoperative data showing no significant difference between both groups in terms of age, sex, manifest refractive spherical equivalent (MRSE), and root mean square (RMS)
Preoperative evaluation
All patients were tested for uncorrected distance visual acuity (UCVA), manifest and cycloplejic refractions, and BCVA. Near vision capabilities were also determined at a distance of 40 cm by testing uncorrected near acuity (UCNA), best corrected near acuity with addition for near vision (BCNA), and DCNA.
All patients were subjected to corneal mapping using the Humphrey® Atlas™ 993 (Carl Zeiss Meditech, Inc, Dublin, CA) Placido-disk corneal topographer, corneal pachymetry, pupil diameter measurement, contrast sensitivity testing using the CSV-1000E (VectorVision, Inc, Greenville, OH) chart, and a detailed slit-lamp examination using the Haag-Streit BM 900 slit-lamp (Haag-Streit International, Bern, Switzerland). ORK-CAM (SCHWIND eye-tech-solutions, Kleinostheim, Germany) software was used for all patients to measure HOAs and design ocular wavefront-guided treatment.
All HOAs were treated in Group A along with the sphere and cylinder, while vertical coma aberrations were left untreated in Group B.
Surgical technique
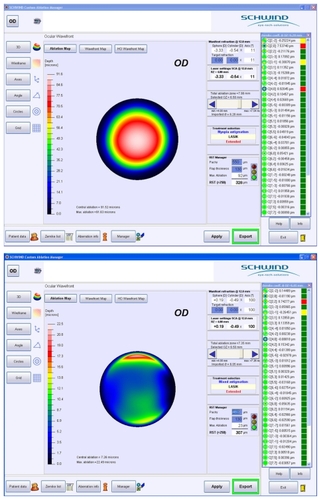
All patients had laser-assisted in situ keratomileusis done using the Moria M2 (Moria, Antony, France) mechanical microkeratome for flap creation. A flap diameter of 9.5 mm and thickness of 130 μm were intended. Wavefront-guided treatment was performed in both groups using the SCHWIND ESIRIS (SCHWIND eye-tech-solutions) excimer laser platform. shows a wavefront map in a patient pre-and postoperatively.
Follow-up and data analysis
Double-masked postoperative follow-up visits were scheduled at 1 day, 1 week, 1 month, and 3 months. The evaluation included measurement of distance UCVA and BCVA, manifest refraction, near UCVA, BCVA, and DCNA. Corneal topography, contrast sensitivity, and aberrometry were done at 1 and 3 months.
Statistical analysis was performed using the Microsoft Excel 2003 (Microsoft Corp, Redmond, WA) Data Analysis Tool Pak. Paired Student’s t-test was applied to compare data means.
Results
Safety
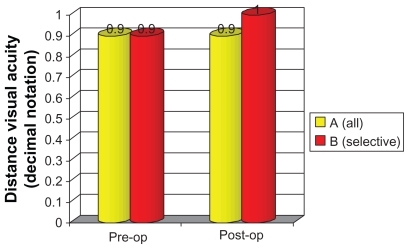
Safety index of the procedure (ratio of postoperative BCVA to preoperative BCVA) at 3 months was 1.0 and 1.1 for groups A and B, respectively, with no significant change in the postoperative BCVA compared with preoperative levels. Similarly, the difference in postoperative BCVA at 3 months between both groups was statistically insignificant ().
Efficacy
UCVA significantly improved at 1 and 3 months postoperatively in both groups (). All cases in both groups achieved a UCVA of 20/30 or better.
Predictability
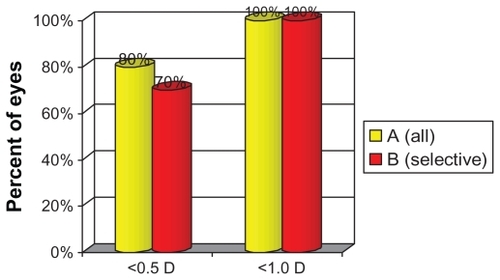
In Groups A and B, 80% and 70%, respectively, of cases were within ±0.5 D of emmetropia at 3 months. All cases in both groups were within 1.0 D of emmetropia. (.)
Near visual acuity
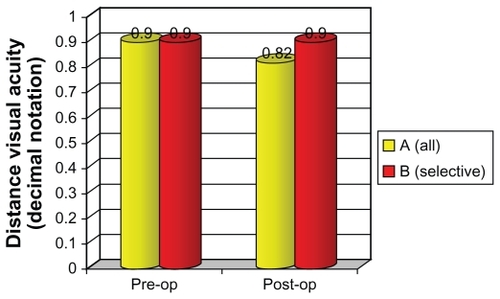
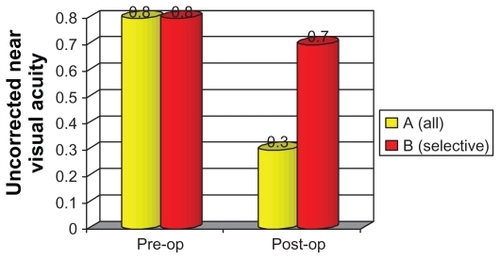
BCNA showed no statistically significant differences at 3 months after the procedure in both groups compared with preoperative levels. Similarly, the difference between both groups in postoperative BCNA at 3 months was statistically insignificant (). UCNA in Group B was significantly better than in Group A patients (P < 0.001) ().
Figure 5 Preoperative (pre-op) and postoperative (post-op) best corrected near acuity with addition for near vision of both groups with the suitable addition showing no significant difference between both groups either pre- or postoperatively.
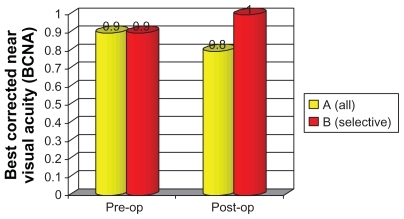
Figure 6 Preoperative (pre-op) and postoperative (post-op) uncorrected near acuity showing no preoperative significant difference between both groups and significant difference postoperatively.
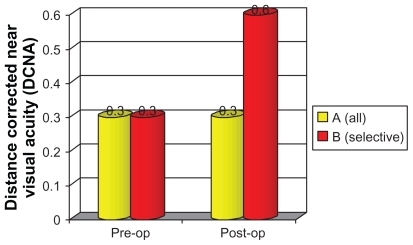
In Group B patients at 3 months after the procedure, DCNA was significantly improved compared with preoperative levels, while negligible difference was recorded in Group A. Postoperative DCNA was significantly better in Group B compared with Group A patients. (.)
HOAs and contrast sensitivity
Three months after the operations, vertical coma was significantly higher in Group B compared with Group A (P < 0.003). Other aberrations did not show statistically significant differences between the two groups in the postoperative period ().
Figure 8 Postoperative high-order aberrations (HOAs) showing no significant difference between both groups except in vertical coma, which was significantly higher in Group B than Group A.
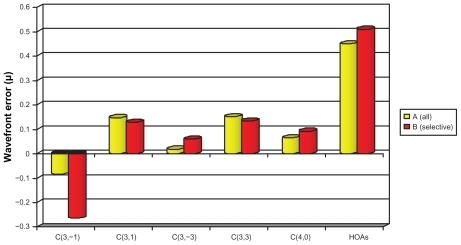
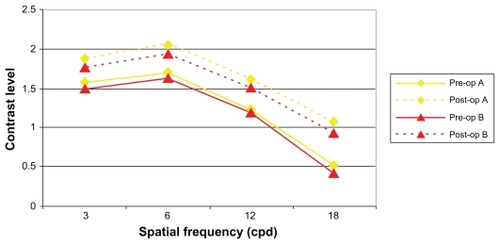
With regard to the comparison of different HOAs pre- and postoperatively, there was no significant difference, in each group, between pre- and postoperative values except in the vertical coma of Group B, which showed significant increase at 3 months postoperatively (P < 0.05). Contrast sensitivity significantly improved in both groups after the procedure (). No significant intergroup contrast sensitivity differences were detected in the postoperative period.
Discussion
Presbyopia correction is one of the most challenging situations in refractive surgery and ophthalmology. The challenges come from the fact that full understanding of accommodation and pathophysiology of presbyopia has not yet been reached. At the same time, presbyopia is the only refractive error that continues to progress with time.
The effect of wavefront aberrations on the quality of vision is quite obvious and several studies have attributed specific visual symptoms to specific types of HOAs. Chalita et alCitation8 showed positive correlation of double vision with total coma and with horizontal coma for the 5 mm and 7 mm pupil sizes, negative correlation between starburst and total coma for the 7 mm pupil size, positive correlation of double vision with horizontal coma, and glare and starburst with spherical aberration and with total aberrations. Melamud et alCitation9 showed that horizontal and vertical coma might be responsible for horizontal and vertical diplopia in symptomatic patients.
Just like all other aberrations, average normal values of coma aberrations vary depending on the pupil size but generally should be approximately 0.35 μm for a 7.0 mmCitation10 and 0.28 μm for 6.0 mm pupil diameter.Citation11
The authors are unaware of any studies that have correlated vertical coma with near vision abilities. It is assumed that vertical coma at certain magnitudes could improve near vision potentials of the eye through increasing the depth of focus. However, to be established, this assumption needs a larger number of cases with longer follow-up periods.
Disclosure
The authors have no conflicts of interest to declare in relation to this paper.
References
- HamiltonDRDavidorfJMMaloneyRKAnterior ciliary sclerotomy for treatment of presbyopia: a prospective controlled studyOphthalmology200210919761977
- MalecazeFJGazagneCSTarrouxMCGorrandJMScleral expansion bands for presbyopiaOphthalmology20011082165217111733253
- MacsaiMSPadnick-SilverLFontesBMVisual outcomes after accommodating intraocular lens implantationJ Cataract Refract Surg20063262863316698485
- Montés-MicóREspañaEBuenoICharmanWNMenezoJLVisual performance with multifocal intraocular lenses: mesopic contrast sensitivity under distance and near conditionsOphthalmology2004111859614711718
- AlióJLTavolatoMDe la HozFClaramontePRodríguez-PratsJLGalalANear vision restoration with refractive lens exchange and pseudoaccommodating and multifocal refractive and diffractive intraocular lenses: comparative clinical studyJ Cataract Refract Surg2004302494250315617915
- JainSAroraIAzarDTSuccess of monovision in presbyopes: review of the literature and potential applications to refractive surgerySurv Ophthalmol1996404914998724641
- McDonaldMBHershPSMancheEEMaloneyRKDavidorfJSabryMConductive Keratoplasty United States Investigators Group. Conductive keratoplasty for the correction of low to moderate hyperopia: US clinical trial 1-year results on 355 eyesOphthalmology200210919781989 discussion; 1989–199012414402
- ChalitaMRXuMKruegerRRCorrelation of aberrations with visual symptoms using wavefront analysis in eyes after laser in situ keratomileusisJ Refract Surg200319S682S68614640435
- MelamudAChalitaMRKruegerRRLeeMSComatic aberration as a cause of monocular diplopiaJ Cataract Refract Surg20063252953216631071
- ChalitaMRFinkenthalJXuMKruegerRRLADARWave wavefront measurement in normal eyesJ Refract Surg20042013213815072312
- SchwiegerlingJScaling Zernike expansion coefficients to different pupil sizesJ Opt Soc A Opt Image Sci Vis20021919371945