Abstract
We report our findings for a patient with orbital apex syndrome associated with herpes zoster ophthalmicus. Our patient was initially admitted to a neighborhood hospital because of nausea and loss of appetite of 10 days’ duration. The day after hospitalization, she developed skin vesicles along the first division of the trigeminal nerve, with severe lid swelling and conjunctival injection. On suspicion of meningoencephalitis caused by varicella zoster virus, antiviral therapy with vidarabine and betamethasone was started. Seventeen days later, complete ptosis and ophthalmoplegia developed in the right eye. The light reflex in the right eye was absent and anisocoria was present, with the right pupil larger than the left. Fat-suppressed enhanced T1-weighted magnetic resonance images showed high intensity areas in the muscle cone, cavernous sinus, and orbital optic nerve sheath. Our patient was diagnosed with orbital apex syndrome, and because of skin vesicles in the first division of the trigeminal nerve, the orbital apex syndrome was considered to be caused by herpes zoster ophthalmicus. After the patient was transferred to our hospital, prednisolone 60 mg and vidarabine antiviral therapy was started, and fever and headaches disappeared five days later. The ophthalmoplegia and optic neuritis, but not the anisocoria, gradually resolved during tapering of oral therapy. From the clinical findings and course, the cause of the orbital apex syndrome was most likely invasion of the orbital apex and cavernous sinus by the herpes virus through the trigeminal nerve ganglia.
Introduction
Orbital apex syndrome is a condition in which the oculomotor nerve, trochlear nerve, abducens nerve, and ophthalmic branch of the trigeminal nerve are damaged. These alterations are generally associated with optic nerve dysfunction. Orbital apex syndrome can be caused by a variety of inflammatory, infectious, neoplastic, iatrogenic/ traumatic, and vascular conditions.Citation1 We present our findings in a patient with orbital apex syndrome associated with herpes zoster ophthalmicus. Magnetic resonance imaging (MRI) showed inflammatory changes that extended to the cavernous sinus and orbital apex. Treatment with intravenous prednisolone 60 mg followed by tapering and vidarabine antiviral therapy markedly improved the extraocular palsies and optic nerve dysfunction. These changes normalized after treatment, which indicated the pathogenesis of the case.
Case report
An 81-year-old woman attended a neighborhood hospital because of nausea and loss of appetite of 10 days’ duration. The internist found that the patient was severely dehydrated, and she was admitted to our hospital on the same day. On the following day, a rash developed along the first division of the trigeminal nerve, and she had a fever of about 38°C. No neck stiffness was reported.
Examination of the cerebrospinal fluid showed 90 cells/μL, with a predominance of lymphocytes and a protein level of 75 mg/dL. IgG for varicella zoster virus in the cerebrospinal fluid was positive on enzyme immunoassay and the unit value was 12.8, but IgM for varicella zoster virus was negative. MRI and computed tomographic images of the head showed no signs of meningitis or edematous changes in the cerebral parenchyma.
Herpetic encephalitis induced by varicella zoster virus was suspected from the clinical findings, so intravenous vidarabine 600 mg/day was initiated in combination with sulbactam + defoperazone sodium and betamethasone 4 mg. The patient still had severe dehydration due to insufficient fluid intake, and her serum creatinine was elevated to 0.96 mg/dL (normal range 0.47–0.79 mg/dL). Thus, we did not use acyclovir systemically because it could have worsened her renal dysfunction. However, the headache and orbital pain worsened. On day 7 of her hospital stay, there was a reduction of the corneal reflex, and herpes keratoconjunctivitis was diagnosed. Treatment with antiviral ointment, acyclovir, and betamethasone eye drops were started. On day 17 of the hospital day, she developed ptosis and total ophthalmoplegia in the right eye (). The pupillary diameters were 4.5 mm OD and 2.5 mm OS, and the light reflex in the right eye was absent (). The anisocoria was pronounced under ordinary room light. Best-corrected visual acuity was 0.5 OD and 1.0 OS. Central critical fusion frequency was 29 Hz OD and 31 Hz OS, and the intraocular pressures were 17 mmHg OD and 14 mmHg OS. Goldmann kinetic perimetry showed a slight constriction of the central visual field in the right eye (). Enhanced T1-weighted MRI showed enhancement of the optic nerve and orbital apex ().
Figure 1 Photographs of eye positions in all directions, and the pupils and face of our patient before treatment. (A) Photographs of eye positions in all directions. Complete ophthalmoplegia and ptosis can be seen on the right side. (B) Photographs of pupils under standard room lighting. Anisocoria can be seen and the right pupil is dilated. The light reflex is absent. (C) Photograph of the face. Mixed vesicular and crusted eruptions can be seen along the first division of the trigeminal nerve. Complete ptosis is present in the right eye. (D) Goldmann kinetic perimetry. Slight constriction of the visual field was detected in the right eye.
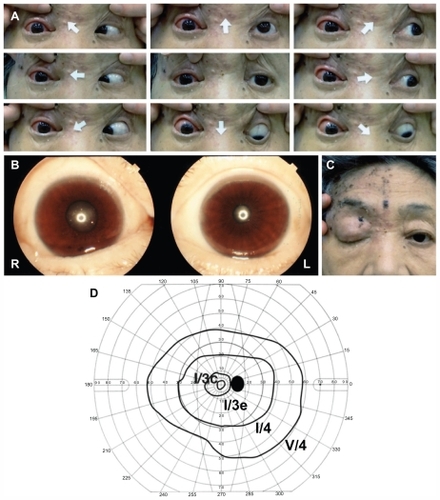
Figure 2 Enhanced fat-suppressed T1-weighted magnetic resonance images. (A and B) before steroid therapy. (C and D) after intravenous prednisolone. (A and C) are horizontal sections. (B and D) rare coronal sections. Enhancement of the optic nerve sheath and orbital apex can be seen before treatment (arrows).
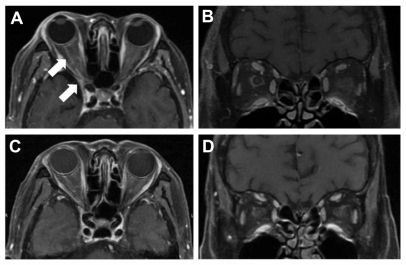
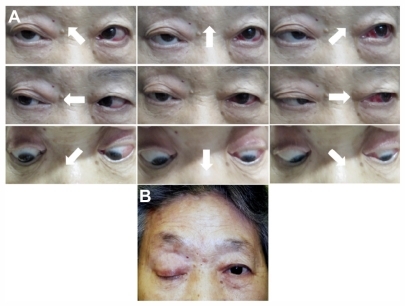
From these clinical findings, ie, orbital inflammation affecting the orbital apex and IgG for varicella zoster virus in the cerebrospinal fluid, the patient was diagnosed with orbital apex syndrome due to varicella zoster virus reactivation.Citation2 After the patient was transferred to our hospital for further treatment, intravenous prednisolone 60 mg/day was started in combination with vidarabine 600 mg/day. The ocular symptoms improved soon after initiation of steroid therapy. The limitation of adduction and supraduction improved from day 1 after initiation of therapy. Repeated MRI showed a decrease in enhancement of the right optic nerve and the tissues around the orbital apex (). Levels of cells and proteins in the cerebrospinal fluid were also decreased. The ptosis had recovered by about 11 weeks after the start of treatment. The right palpebral fissure was 9 mm and levator function was 10 mm. Twelve weeks after onset, diplopia at the primary position disappeared, and the best-corrected visual acuity in the right eye improved to 1.0 (). Twenty weeks after onset, eye movements were almost completely recovered, except for abduction (). However, the anisocoria still remained, despite the patient taking prednisolone 15 mg/day.
Figure 3 Time course of ocular symptoms and signs after onset of orbital apex syndrome. After onset, the amount of steroid was increased from betamethasone 4 mg, and the converted amount of prednisolone was 26–60 mg. Ocular movement, visual acuity, and ptosis gradually improved thereafter. Vidarabine was also given for 12 days after the onset of orbital apex syndrome.
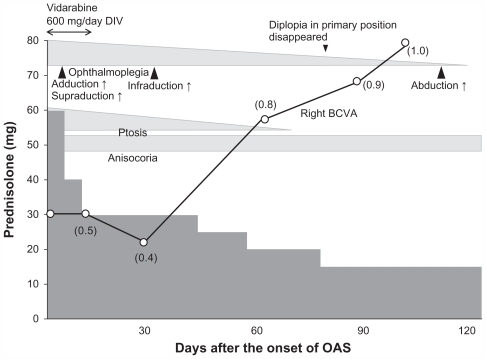
Figure 4 Photographs of eye positions in all directions five months after initiation of therapy. (A) Most ocular movements are markedly improved, except for abduction. Subconjunctival hemorrhage is present in the left eye. (B) Photograph of face one month after initiation of therapy. The skin lesions are almost resolved but ptosis remains.
Discussion
Herpes zoster ophthalmicus can be triggered by reactivation of varicella zoster virus that is dormant in the trigeminal nerve ganglia. Reactivation of varicella zoster virus can be triggered by aging, an immunocompromised host, trauma, surgery, iatrogenic immunosuppression, tuberculosis, syphilis, and radiation therapy. Half of herpes zoster ophthalmicus cases have ocular complications, including blepharitis, keratoconjunctivitis, iritis, scleritis, and acute retinal necrosis.Citation3 Neurological complications, such as ophthalmoplegia and optic neuritis, are rare, but are responsive to antiviral or steroid treatment. Ophthalmoplegia was found in 3.5%–10.1% of two large herpes zoster ophthalmicus series.Citation3,Citation4 Among the cases with extraocular nerve palsies, oculomotor nerve palsy is the most frequent and abducens nerve palsy the second most frequent.Citation5,Citation6
Several cases of orbital apex syndrome have been reported in association with more severe herpes zoster ophthalmicus.Citation7–Citation12 Shirato et al reported a 71-year-old man who developed orbital apex syndrome 12 days after onset of herpes zoster ophthalmicus.Citation7 T1-weighted, gadolinium-enhanced MRI showed diffuse enhancement of the orbital fat, ocular muscles, and optic nerve on the right side. They used systemic prednisolone 30 mg followed by tapering. Five months after the onset of herpes zoster ophthalmicus, the extraocular palsies and ptosis were slightly improved, but there was no improvement in visual acuity. Kattah and Kennerdell reported two cases of orbital apex syndrome associated with herpes zoster ophthalmicus.Citation8 Both cases developed extraocular palsies and optic nerve dysfunction one and five days after onset of rash. After oral prednisolone 80 mg, one of the patients recovered fully from the neurological complications, and the other patient had an improvement in ophthalmoplegia and optic neuritis, but the left eye progressed to endophthalmitis followed by corneal perforation.
Krasnianski et al reported a case of orbital apex syndrome with complete ophthalmoplegia due to orbital myositis and optic neuritis two days after the onset of herpes zoster ophthalmicus. Citation10 The case was a 67-year-old woman who was treated with acyclovir 750 mg for 10 days with prednisolone 100 mg intravenously for three days, and then the prednisolone was tapered. MRI with gadolinium enhancement showed marked thickening of all the external ocular muscles and optic nerve sheath on the right side. Four weeks later, the extraocular muscle palsies and optic neuritis recovered almost completely.
Bourke and Pyle reported a 63-year-old woman with herpes zoster ophthalmicus who developed complete ptosis, total ophthalmoplegia, and loss of visual acuity 10 days after the rash developed.Citation11 Treatment consisted of intravenous methylprednisolone 500 mg/day for three days, followed by a two-week course of oral prednisolone reducing by 80 mg/day. Oral acyclovir 800 mg every four hours was also used. The ocular movements slowly improved. The day following initiation of therapy, supraduction, infraduction, and incyclotorsion were slightly improved. Visual acuity also increased from finger counting to 6/24 on the next day, and further improved to 6/18 soon thereafter. At one year after onset, visual symptoms were completely resolved.
Dhingra et alCitation9 reported a case of orbital apex syndrome associated with herpes zoster ophthalmicus and multiple myeloma. The signs and symptoms of herpes zoster ophthalmicus developed after the patient had completed chemotherapy. Although systemic acyclovir and prednisolone 30 mg slightly improved the visual acuity and disturbances of eye movements, the ptosis, anisocoria, and partial ophthalmoplegia did not improve. Saxena et alCitation12 also reported a case of human immunodeficiency virus associated with herpes zoster ophthalmicus. A 29-year-old woman developed severe anterior uveitis, optic neuritis, complete ptosis, and ophthalmoplegia due to myositis 14 days after the onset of a facial rash. Serological testing was positive for human immunodeficiency virus. Highly active antiretroviral therapy and oral acyclovir 800 mg five times a day were started. Five days later, oral prednisolone 1 mg/kg/day was combined with highly active antiretroviral therapy and acyclovir therapy. By the end of four weeks, visual acuity and extraocular motility were markedly improved.
In most of the earlier reports, and in our patient, orbital apex syndrome developed within 14 days of onset of herpes zoster ophthalmicus and was relatively responsive to steroid therapy, but may need more than 60 mg of prednisolone. The outcomes of visual function were good, although the duration of treatment may need to be from four weeks to one year.
Sanjay et al summarized the clinical characteristics and course of 20 well documented cases of herpes zoster ophthalmicus presenting with complete ophthalmoplegia.Citation13 Herpes zoster ophthalmicus preceded the ophthalmoplegia as orbital apex syndrome by a mean interval of 9.5 days. Sixty-five percent of these cases recovered completely or partially after antiviral and steroid therapy, although anisocoria remained in most cases, as in our patient. In consideration of our case and the earlier reports, combined antiviral and steroid therapy should be effective in cases of orbital apex syndrome if the steroid therapy is used for at least four months.
The pathological mechanism for ophthalmoplegia in cases of herpes zoster ophthalmicus has not been determined. Histopathological studies have demonstrated significant perivascular and perineural inflammation of the ocular tissues, including the optic nerve, cavernous sinus, superior orbital fissure, and retina.Citation14 Earlier histological studies on autopsy specimens have suggested two possible pathological mechanisms, ie, reactivation of varicella zoster virus in the trigeminal ganglion, which then invades the cavernous sinus and superior orbital fissure,Citation5 and a second mechanism might be lymphocytic infiltration of the affected nerves by sensory offshoots of the trigeminal nerves to all the motor nerves of the eye.Citation15 Naumann et al showed that inflammatory cells infiltrated the orbital apex along the long posterior ciliary vessels and nerves in 21 enucleated eyes affected by herpes zoster ophthalmicus, indicating that the neuropathy arises from an occlusive vasculitis.Citation16 Thus, the ophthalmoplegia and optic neuritis are suggested to be due to direct invasion by varicella zoster virus or by an inflammatory reaction and occlusive vasculitis after virus invasion. Lexa et al reported a case of herpes zoster ophthalmicus with optic neuritis, total ophthalmoplegia, and cerebellar manifestations.Citation14 Enhanced MRI showed enhancement around the optic nerve sheath, which corresponded with the post mortem findings of invasion of inflammatory cells into the sheath of the optic nerve and ischemic changes in the optic nerve axons.
Cases of herpes zoster ophthalmicus with optic neuritis have been reported, and MRI and computed tomography show direct spread of granulomatous inflammation into the orbital apex.Citation8,Citation11 Immunohistological examination of an autopsy specimen in a case of human immunodeficiency virus infection showed direct invasion of varicella zoster virus into the retina and optic nerve.Citation17
Our patient responded well to steroids and antiviral therapy, although the time needed to achieve significant resolution was more than five months. However, treatment for herpetic encephalopathy, with which our patient was initially diagnosed, might not have been long enough to improve symptoms. MRI findings showing enhancement of the optic nerve might reflect a direct inflammatory reaction rather than occlusive vasculitis.
In conclusion, herpes zoster ophthalmicus is a relatively common disease in clinical ophthalmological practice, but is rarely accompanied by neurological complications. Orbital apex syndrome should be considered among the more severe ocular complications of herpes zoster ophthalmicus. If combined antiviral and steroid therapy is initiated early, it can be expected that visual dysfunction will recover. Therefore, ophthalmologists should be careful not to miss the neurological complications, and be especially vigilant during the 14 days after onset of herpes zoster ophthalmicus.
Acknowledgment
We thank Professor Duco Hamasaki, Bascom Palmer Eye Institute, University of Miami School of Medicine, for editing this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- YehSForoozanROrbital apex syndromeCurr Opin Ophthalmol200415649049815523194
- GildenDCohrsRJMahalingamRNeurological disease produced by varicella zoster virus reactivation without rashCurr Top Microbiol Immunol201034224325320186614
- WomackLWLiesegangTJComplications of herpes zoster ophthalmicusArch Ophthalmol1983101142456600391
- MarshRJCooperMOphthalmic herpes zosterEye (Lond)19937 Pt 33503708224290
- EdgertonAEHerpes zoster ophthalmicus: report of cases and a review of the literatureTrans Am Ophthalmol Soc19424039043916693295
- MarshRJDulleyBKellyVExternal ocular motor palsies in ophthalmic zoster: a reviewBr J Ophthalmol19776111677682338027
- ShiratoSOshitariTHanawaKMagnetic resonance imaging in case of cortical apex syndrome caused by varicella zoster virusOpen Ophthalmol J2008210911119517035
- KattahJCKennerdellJSOrbital apex syndrome secondary to herpes zoster ophthalmicusAm J Ophthalmol1978853378382306754
- DhingraSWilliamsGPearsonASevere permanent orbital disease in herpes zoster ophthalmicusOrbit200827432532718716975
- KrasnianskiMSievertMBauVExternal ophthalmoplegia due to ocular myositis in a patient with ophthalmic herpes zosterNeuromuscul Disord200414743844115210167
- BourkeRDPyleJHerpes zoster ophthalmicus and the orbital apex syndromeAust N Z J Ophthalmol199422177808037920
- SaxenaRPhuljheleSAalokLA rare case of orbital apex syndrome with herpes zoster ophthalmicus in a human immunodeficiency virus-positive patientIndian J Ophthalmol201058652753020952840
- SanjaySChanEWGopalLComplete unilateral ophthalmoplegia in herpes zoster ophthalmicusJ Neuroophthalmol200929432533719952908
- LexaFJGalettaSLYousemDMHerpes zoster ophthalmicus with orbital pseudotumor syndrome complicated by optic nerve infarction and cerebral granulomatous angiitis: MR-pathologic correlationAJNR Am J Neuroradiol19931411851908427086
- ArchambaultPWiseJSRosenJHerpes zoster ophthalmoplegia. Report of six casesJ Clin Neuroophthalmol1988831851932971683
- NaumannGGassJDFontRLHistopathology of herpes zoster ophthalmicusAm J Ophthalmol19686545335415300433
- GrevenCMFordJStantonCProgressive outer retinal necrosis secondary to varicella zoster virus in acquired immune deficiency syndromeRetina199515114207754241