Abstract
Purpose
To assess attitudes of pre-clinical undergraduate medical students toward learning smartphone funduscopy (SF) and its appropriateness as a teaching tool.
Patients and Methods
Second year medical students received instruction on direct ophthalmoscopy (DO) and SF; they were then paired with a peer and randomly assigned to perform DO or SF first. The SF technique involved freehand alignment of the axes of the smartphone camera with a condenser lens. Both techniques were done through a maximally dilated pupil. A questionnaire was completed to acquire data on baseline experience, performance of both examination techniques, attitudes, and appropriateness. Statistical significance testing and Bland-Altman analysis were used to determine differences between DO and SF, and a multivariable mixed regression model was fitted to identify any predictors for positive attitudes toward DO or SF.
Results
One hundred thirty-seven (137) individuals completed the study. A similar proportion of students could identify the optic nerve, macula, and vessels using DO and SF. However, self-reported quality scores were higher for DO for the optic nerve (p = 0.006) and macula (p = 0.08). The mean (standard deviation) attempts to identify these major structures were 2.7 (SD 2.3) for DO and 4.5 (SD 2.9) for SF (p < 0.001). Attitudes of students were consistently more positive toward DO across the five questions assessed. A small subset of students had equally positive attitudes toward DO and SF. Improved quality scores were predictive of positive attitudes for both DO and SF. Ultimately, 24% of students preferred SF over DO.
Conclusion
Among inexperienced examiners of the fundus through a dilated pupil, SF is a non-inferior technique to DO in identifying structures. Despite overall favorable attitudes towards the more familiar DO, those students who quickly learned the SF technique had similar satisfaction scores. Teaching SF should be considered in undergraduate medical education.
Introduction
Since first reported in the literature in 2010, improvements in smartphone camera technology have been a boon for recording images and videos of the ocular fundus.Citation1 Bastawrous et al initially described a free-hand technique that simply requires aligning the smartphone camera axis with that of the condenser lens.Citation2 This is the most basic setup requiring no additional hardware, and newer smartphone models have faster image processors, higher resolution sensors, better optics, and constant powerful light sources. Since the mid-2010s, several commercially available apparatuses have entered mass production to reduce the challenges of the freehand technique. For example, two apparatuses, Peek RetinaCitation3 and D-EYE,Citation4 are based on principles of direct ophthalmoscopy whereas another apparatus, the Paxos scope,Citation5 is based on the indirect ophthalmoscope and fixes the condenser lens in place. In recent years, more options for the indirect ophthalmoscopy smartphone technique have been produced, such as an open-source 3D printable apparatus by Dr. Albert HuCitation6 or a smartphone head mount to simulate indirect ophthalmoscopy.Citation7 The design of these commercially available apparatuses is of critical importance, allowing for variable fields of view, working distance, dilation dependency, and smartphone compatibility.Citation8 Apparatuses like Peek Retina and the simple 20 D condenser lens are universally compatible with smartphones, however, the iExaminer (Welch Allyn), D-EYE, and iNview (Volk) have narrow compatibility with specific smartphone generations.Citation8
Variations of these apparatuses have been clinically validated in adult patients by comparing to a referenced gold standard, such as a conventional fundus camera, indirect ophthalmoscopic exam, or slit lamp biomicroscopy by a trained ophthalmologist.Citation3,Citation9 Agreement between smartphones fundus photos and dedicated retinal cameras is approximately 78%, despite heterogeneous classifications of criteria for detection. For example in diabetic retinopathy, a dichotomous refer or non-refer decision yielded as high as 91% agreement between smartphone and conventional imaging.Citation5 Even in neonates, whose examination cooperation is limited, smartphone-based imaging is becoming viable with deployments for imaging in retinopathy of prematurity.Citation10,Citation11 More recently, artificial intelligence (AI) software has been used to analyze images acquired by smartphone-based apparatuses.Citation12,Citation13 Early studies on deep-learning frameworks for detection of vision-threatening diabetic retinopathy has shown promising results.Citation14 This has furthered the potential for smartphone funduscopy (SF) in mass population screening programs.
Low-resourced settings, which are not necessarily limited to low- and middle-income countries only, are prime applications for smartphone-based fundus imaging. Although low-cost direct ophthalmoscope options exist for low-resourced settings (ie, ArclightCitation15,Citation16), the advantage of magnification of images, storage of images, and data connectivity to allow sharing of images from a smartphone cannot be understated.Citation17 The coronavirus pandemic has placed a spotlight on new opportunities for telemedicine to improve access to health care while maintaining quarantine mandates and social distancing guidelines.Citation18 Smartphone-based fundus imaging can be used in conjunction with telemedicine as an avenue for screening examinations, including diabetic retinopathy, glaucoma, retinopathy of prematurity, or even in emergency setting.Citation17 To achieve optimal funduscopic screening examinations, multiple commercially available apparatuses may be required.Citation8 The Volk iNview has a large field of view with good image quality, which makes it an ideal choice for diabetic retinopathy screening, whereas the iExaminer has a small field of view but good magnification making it ideal for assessing glaucomatous changes to the optic nerve.Citation8 Moreover, applications in high-income countries can lower costs of large-scale screening programs targeting populations with historic disadvantages and relatively poorer health outcomes.Citation19 Training of healthcare professionals should continually be updated in order to align with new technological possibilities. In this case, the deployment of smartphones to image the fundus appears to be feasible and perhaps a newly indispensable aspect of the basic physical examination.
In undergraduate medical education in high-income countries, the vast majority of students are still taught direct ophthalmoscopy since these tools have been more historically available. However, Kelly et al demonstrated medical students’ preference of identifying posterior segment anatomy with fundus photography, especially among junior medical students.Citation20 Used by these trainees, SF produces images of comparable clinical utility to an average quality fundus camera.Citation21 Moreover, the landmark FOTO-ED study demonstrated that older model smartphones can capture images of useful quality on an objective scale.Citation22 The aforementioned D-EYE apparatus is preferred by 77–91% of medical students over direct ophthalmoscopy.Citation23,Citation24 For most individuals undergoing medical training, they will need to rely on equipment provided by their clinical environment. Ideally, the equipment replaces the conventional direct ophthalmoscope, commonly sold at an equivalent price of a D-EYE or Peek Retina. This price point is also similar to 20D or 28D condenser lenses, and these tend to be already available at major referral centers, such as eye hospitals and large quaternary facilities with teaching programs. Although smartphones add an additional cost, ownership among healthcare workers and medical students is rapidly growing which makes this less cost prohibitive.Citation25,Citation26 Therefore, we designed this study to assess the attitudes of pre-clinical medical students toward learning SF and its appropriateness as a clinical tool.
Methods
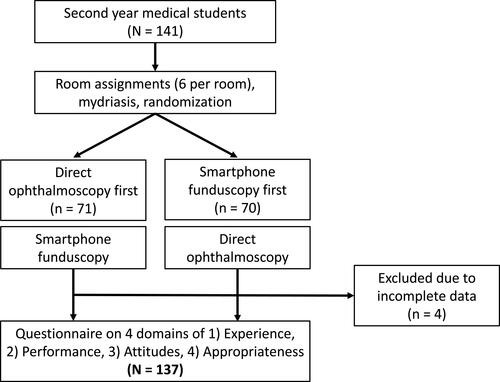
At University of Minnesota (UMN) Medical School in March 2018, pre-clinical medical students in their second of four years of the standard US Doctor of Medicine (MD) curriculum were recruited into this study. This occurred during the annual ophthalmology skills workshop designed to reinforce skills for basic eye examination. Students were organized into rooms of six individuals and worked in pairs. Each room had a lead instructor who was an ophthalmology post-graduate year 2–4 or an attending ophthalmologist. All lead instructors were already well-versed in acquiring fundus photos using the freehand condenser lens and smartphone technique after being trained by the most experienced users. Three rooms had five students, so that instructor became the examinee. The study flow diagram is depicted in . All medical students had similar exposure to direct ophthalmoscopy (DO) from our institution’s standard physical examination series in their first year. All students received the same SF exposure by watching an instructional video and reading an article on EyeWikiCitation27 one week prior to the workshop, although no formal assessment was made for assuring students reviewed this material.
In each room, the six students were divided into pairs and randomized to either perform DO first or SF first. Thus, there was a 50:50 distribution among those who started SF or DO first. Examination occurred after mydriasis of one pupil (laterality was based on individual student preference) with topical phenylephrine 2.5% and tropicamide 1% ophthalmic solutions. The room instructors then demonstrated DO and SF techniques, providing step-by-step guidance of funduscopic examination. The total combined instruction time for both techniques was 20–25 minutes. The direct ophthalmoscopes were all standard wall-mounted Welch Allyn, and 20 diopter Volk condenser lenses with minimal-to-no scratches were used for SF. The model of smartphone varied as they depended on each individual student examiner. This was deemed appropriate since it was imperative the student use a personal phone for general applicability beyond a controlled study setting. The model of phone was recorded. All phones had digital zooming and focusing capability as well as a light source. As for the freehand technique, the examiner used the phone’s native camera application in video mode, turned on the light source, and aligned the camera held in the dominant hand and the condenser lens held in the less dominant. The examinee was instructed to focus on an object straight ahead in the central visual axis. If the examinee could not tolerate the light intensity, a single piece of Scotch® semi-transparent tape was placed over the light source. An attempt was considered a continuous examination without a self-imposed halt. If the examinee requested a break to dim the light source with tape, this attempt by the examiner was not counted toward their total number of attempts to clearly identify landmarks. The examiner would make adjustments in working distance until the correct focal point was achieved to visualize a clear optic nerve head and main vessels. The examinee was then asked to look directly at the camera for visualization of the macula. This sequence was captured as a video.
All students completed a post-workshop questionnaire consisting of 25 questions; the questionnaire was developed for the purposes of this study only and was not adapted from any previously validated survey (Supplemental Data). One of the study authors has extensive experience in large survey and semi-structured interview methodology (TT). The 4 major domains assessed were: 1) Experience, 2) Performance, 3) Attitudes, 4) Appropriateness. Significance testing was performed to compare DO and SF, using a combination of parametric (Х2 test, paired t-test) for continuous variables, Wilcoxon Rank-Sum to compare Likert scale scores, Bland-Altman analysis, and mixed effects linear regression modeling to identify variables associated with positive attitude toward SF. STATA 16 was used to perform these analyses (StataCorp, College Station, Texas, United States), and significance level was set at p < 0.05.
The study was exempted from institutional review board and approved as a quality improvement project not human subjects research (UMN IRB 00002974). All students were notified of the study one week in advance with information provided in standard informed consent processes, such as risks, benefits, voluntary nature, and right of refusal. All students were provided instructions on how to opt out. All data were kept de-identified, and written consents were not acquired to maintain anonymity.
Results
One hundred thirty-seven (137) individual records were available for analysis; 61.3% of students had hands-on examination experience with DO prior to this study versus 9.6% with hands-on SF experience (p < 0.001). Evaluating performance, there was no significant difference in proportion of students who could identify the optic nerve, macula, or vessel arcades (). For SF, the instructors could verify by viewing the live aerial image and recorded video file, while for DO, successful viewing was not verifiable and depended on self-reporting. For quality ratings, students provided their own self-assessment for both DO and SF. Instructor rating was not acquired. Students self-reported higher quality with DO for the optic nerve (p = 0.006) and macula (p = 0.08, ). Efficiency was based on number of attempts the students took to successfully identify all three structures. An attempt was considered a continuous examination without a self-imposed halt. Mean number of attempts with DO was 2.7 (SD 2.3) and 4.5 (SD 2.9) for SF (p < 0.001). The proportion of students who could not identify all three structures was 0.06 for DO versus 0.17 for SF (p < 0.001, ).
Figure 2 Performance evaluation of smartphone funduscopy (SF) and direct ophthalmoscopy (DO). (A) Proportion of medical students identifying optic nerve (SF 0.75, DO 0.77, p = 0.651); macula (SF 0.47, DO 0.54, p = 0.252), and vessels (SF 0.79, DO 0.84, p = 0.285). (B) Quality rating of structures (1 = worst, 5 = best). Median [interquartile range] for optic nerve: SF is 3[2–4] and DO is 4[3–4], p = 0.006. Values for macula: SF is 3[1–4] and DO is 3[2–4], p = 0.08. (C) Proportion of medical students by categories based on the number of attempts to successfully identify the optic nerve, macula, and vessels. The top block represents the proportion of students who did not identify all three structures: 0.17 for SF and 0.06 for DO (p = 0.001).
![Figure 2 Performance evaluation of smartphone funduscopy (SF) and direct ophthalmoscopy (DO). (A) Proportion of medical students identifying optic nerve (SF 0.75, DO 0.77, p = 0.651); macula (SF 0.47, DO 0.54, p = 0.252), and vessels (SF 0.79, DO 0.84, p = 0.285). (B) Quality rating of structures (1 = worst, 5 = best). Median [interquartile range] for optic nerve: SF is 3[2–4] and DO is 4[3–4], p = 0.006. Values for macula: SF is 3[1–4] and DO is 3[2–4], p = 0.08. (C) Proportion of medical students by categories based on the number of attempts to successfully identify the optic nerve, macula, and vessels. The top block represents the proportion of students who did not identify all three structures: 0.17 for SF and 0.06 for DO (p = 0.001).](/cms/asset/b1033309-1a3a-424b-8cbc-a8ee2b9f919e/doph_a_12177087_f0002_b.jpg)
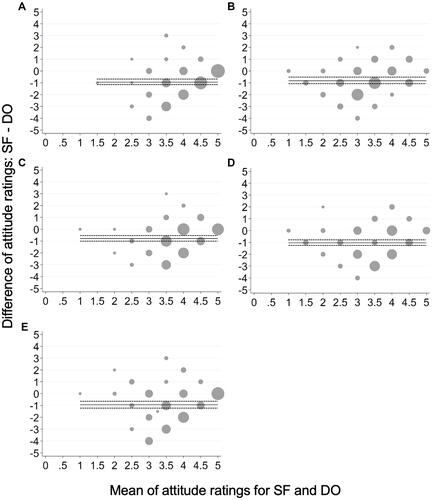
The attitudes of students were consistently more positive toward DO across all five questions (). Bland-Altman analysis was used to further explore each of the five questions assessed (). Students were generally scattered about their own confidence in using either technique after receiving instruction. As for whether each method should be integrated into the curriculum, the majority were slightly above ambivalent (rating of 3) with a slight majority favoring of DO over SF (more values in the negative in the Bland-Altman plots). When assessing their attitudes for usefulness in a clinical setting to examine patients for pathology, as a teaching tool for the fundus examination, and recommendation of each technique, there is a small subset of students who endorsed ratings of 5 for both techniques, thus minimizing disagreement between either method (SF – DO value nears 0). This was not the case with confidence in imaging or integration into the curriculum as there was more variation yet favoring DO (). To assess what was predictive of positive attitudes toward either imaging technique, a mixed effects linear regression model was fitted in which the dependent variable was the sum rating of the 5 previously mentioned attitudes-based questions, and the independent variables were experience, ophthalmology interest (if it was listed as one of 3 interested specialties), total number of structures identified, and total quality rating (sum of score for optic nerve and macula). Only the total quality score significantly predicted a higher total attitude rating (). This positive association was consistent for both DO and SF with a higher magnitude observed for SF.
Table 1 Attitudes of Students Toward Direct Ophthalmoscopy and Smartphone Funduscopy
Table 2 Mixed Effects Regression Model on Attitude of Students
Figure 3 Bland-Altman analysis adjusted for trend of attitudes of students toward direct ophthalmoscopy (DO) and smartphone funduscopy (SF). The X axis represents the mean of ratings of both techniques with scaling from 1 (most disagreement) to 5 (highest agreement), and the Y axis represents the difference in values between the rating for SF minus DO. The size of the grey circle represents the number of students at that specific point. The black solid line is the mean bias and the dotted black lines represent the confidence limits about the mean bias. (A) Usefulness in clinical setting. Mean bias: −0.95 (95% CI, −1.18 to −0.72). (B) Confidence in imaging method. Mean bias: −0.83 (95% CI, −1.05 to −0.61). (C) Teaching tool for fundus imaging. Mean bias: −0.78 (95% CI, −1.00 to −0.57). (D) Integration into curriculum. Mean bias: −1.04 (95% CI, −1.29 to −0.79). (E) Recommend imaging method. Mean bias: −0.94 (95% CI, −1.20 to −0.68).
In appropriateness, 69% of students preferred DO over SF with only 24% preferring SF over DO (). Students generally felt more physically comfortable when being examined by DO (p < 0.001, ). However, 46.9% of examinees felt more comfortable with tape placed over the LED light source from the smartphone. For all examinees, one layer of Scotch® semi-transparent tape was enough to reduce the intensity of light to a more tolerable level though there are smartphone applications that allow reduction digitally. The smartphone model used by each examiner was recorded: Apple iPhones (5, 6, 7, 8, X) accounted for 73.9% of smartphones used in the study, followed by unreported (12.3%), Samsung Galaxy (9.4%), and finally various others (Note 5, Moto G5, Google Pixel) accounting collectively for 5.1%. No statistically significant association was determined between model of smartphone and quality of optic nerve and macula; there was also no association with total attitude rating (). Therefore, whichever smartphone the student was most accustomed to using was appropriate for use in SF.
Table 3 Univariate Association Between Total Quality Score, Total Attitude Rating, and Smartphone Models
Discussion
We performed a prospective randomized medical education study to assess preference of preclinical medical students regarding smartphone funduscopy (SF) to conventional direct ophthalmoscopy (DO). Though more medical students preferred DO over SF coupled with higher performance marks for DO and more favorable attitudes toward DO, the data show those students who had a better experience with SF viewed it just as positively as DO, if not even more positively. Our results contrast with other comparable studies in the literature;Citation23,Citation24,Citation28–Citation30 however, these other studies used commercially available smartphone imaging apparatuses, D-EYE and PEEK retina, which are also imaging techniques that are more directly comparable to conventional DO. We posit the stark differences in our study are due to imaging technique and difficulty of freehand positioning a condenser lens with a smartphone, such that the imaging axis is aligned well enough to produce a quality image. These skills require repeated practice, and a half-day workshop session may not be sufficient for beginning, preclinical medical students, among whom the vast majority do not have any ophthalmic examination experiences.Citation31–Citation34
Experience and Performance
There are inherent limitations of comparing DO and SF. The individuals who had a priori hands-on experience with DO far outnumbered those who endorsed experience with SF. Surprisingly, having hands-on SF experience was not predictive of a higher total quality score. Even though a majority of our students had exposure to DO, this does not necessarily translate to being fully adept at the examination as other studies have demonstrated in more advanced trainees.Citation35,Citation36 Therefore, despite a discrepancy between technique exposure among our students, it is reasonable to assume the skill levels were compatible enough to allow direct comparison. The performance metrics did not measure as we expected with similar proportions of students being able to identify the three structures and higher quality scores for DO. Quality scoring is an imperfect measurement even though we only compared self-reported scores. Perhaps those who did SF first and received feedback from their instructors were then able to more objectively rate structures in DO. The DO’s higher magnification may bias quality scoring as well. All of this confirms our hypothesis that the freehand SF technique requires skills that most medical students do not acquire in the usual course of medical education. Efficiency of performance, measured in number of attempts, is consistent with this assessment. This SF technique might be a useful bridge to teaching indirect ophthalmoscopy with a binocular indirect headset.
Attitudes and Appropriateness
The attitude ratings favored DO across all five questions, and only 12% rated total SF attitudes 20 and above (maximum of 25). The Bland-Altman analysis shows this 12% viewed both techniques positively. This contrasts with the use of D-EYE in other reports in preclinical medical students.Citation23,Citation24 It is likely more students will view SF more favorably if given more time to practice and produce clinically useful images, which is what the regression model suggests: higher quality scores were significantly predictive of more positive attitude. Appropriateness for clinical use by medical students and non-ophthalmology clinicians with this SF technique is questionable. Our students preferred DO by far and the light intensity required with SF is similar to the discomfort experienced with conventional indirect ophthalmoscopy. Perhaps the value added is (1) teaching the fundus examination and (2) enabling each trainee to see their own posterior pole anatomy. This SF technique can be used to reinforce DO skills where students are given a set period to match the DO exam findings with an image acquired by SF.Citation37,Citation38
Given the availability of condenser lenses, it is feasible for nearly all undergraduate medical education programs in high-resource settings to teach this technique. Commercially available apparatuses, such as Paxos Scope (indirect ophthalmoscope-based), D-EYE and Peek (direct ophthalmoscope-based), or simulatorsCitation3,Citation32,Citation39–Citation42 require added expenses to the teaching institution. As for DO, it is an essential skill that may be reinforced with new low-cost direct ophthalmoscopes, and the most promising at the current moment is the ArcLight.Citation43 There is a role for D-EYE or Peek to improve DO skills for institutions who can afford to make these devices accessible; for example, Mamtora et al combined D-EYE with a mannequin simulator displaying common ophthalmic pathologies.Citation44 Of course, the same can be done using the freehand condenser lens SF technique and as mentioned previously, this can help bridge the teaching of indirect ophthalmoscopy to relevant trainees.
The SF technique we introduced requires more investment by the trainee as the manual skills and visual reasoning required are different than DO. Used by experienced ophthalmologists, the freehand SF technique described in our study has a 93.6% sensitivity to detect moderate non-proliferative diabetic retinopathy or worse diabetic retinopathy compared to 100 Optos photos.Citation45 Taking these challenges into consideration, a non-inferior performance in identifying structures is promising. The advantages in education and clinical application are clear. Instructors and trainees can review images and video files to objectively critique technique for improvement, review of media is easier to teach trainees ophthalmic pathology,Citation46,Citation47 media can be uploaded securely using applications such as Haiku, and clinical decision support can be made more expeditiously if a specialist can review these images in a timely manner. Our data does not support replacement of DO with SF, but follow-on studies that enable more time and practice with granular and critical objective evaluation of performance outcomes may answer these questions.
Limitations
There are several limitations to our study not already mentioned previously. The questionnaire was developed for this study using general good practice principles to acquire objective data and focused, scale-based questions for subjective assessments, but the questionnaire itself has not been previously used. The quality scoring could have benefitted by showing the students a live image from a DO with different levels of quality rather than simply explaining it, as in our case. The laterality of the dilated pupil was not standardized, so most picked their non-dominant eye, and there was a variety of left and right eye combined with a supermajority right-hand dominant cohort of examiners. Imaging either eye should not require a high degree of ambidextrousness, but this may contribute to reducing quality that we could not account for in our analysis. Additionally, instructors were unable to verify student visualization of fundus anatomy, which is an inherent limitation of DO. It is conceivable that students may have overestimated their competency in DO in the absence of verification. This highlights a major benefit of smartphone funduscopy, capturing images, and being able to share them in real time. The inherent limitation of surveying students once is we do not know if the skills gained were durable. We attempted to address all of these anticipated limitations with the large sample size, the randomization, and ensuring completion of questionnaires by all willing participants. The limitations of the freehand condenser lens SF technique include necessity for mydriasis, delicate hand-eye coordinated movements while capturing an inverted aerial image, discomfort from the light source required for adequate illumination. The comfort issue was addressed using tape, and substantially more a priori exposure to DO. Finally, freehand SF requires coordinated movements in order to align the instruments correctly, whereas direct ophthalmoscopes are specifically designed and mass-produced to function as a well-aligned optic system without need for significant coordination among the users.
Conclusion
We have demonstrated that SF is non-inferior to DO, aided by mydriasis, in identifying three major normal anatomical structures (optic nerve, macula, vessels), and preclinical medical students who produced clinically useful images by the freehand condenser lens SF technique had positive attitudes toward learning and applying the technique. Smartphone imaging technology will only improve and permeate even resource-poor settings. We believe SF will become an indispensable skill in training and ophthalmic care delivery especially in coordination among clinical services and expediting urgent ophthalmic pathology. The resources of the healthcare organization will determine how SF is taught or deployed. We do not advocate one technique over the other but only to teach it as a component of the ophthalmic examination curriculum.
Disclosure
The authors have no financial or conflicts of interests to declare in relation to this study, the materials used, and this manuscript.
Additional information
Funding
References
- Lord RK, Shah VA, San Filippo AN, Krishna R. Novel uses of smartphones in ophthalmology. Ophthalmology. 2010;117(6):1274–1274 e3. doi:10.1016/j.ophtha.2010.01.001
- Bastawrous A. Smartphone fundoscopy. Ophthalmology. 2012;119(2):432–433e2; author reply 433. doi:10.1016/j.ophtha.2011.11.014
- Bastawrous A, Giardini ME, Bolster NM, et al. Clinical validation of a smartphone-based adapter for optic disc imaging in Kenya. JAMA Ophthalmol. 2016;134(2):151–158. doi:10.1001/jamaophthalmol.2015.4625
- Russo A, Morescalchi F, Costagliola C, Delcassi L, Semeraro F. Comparison of smartphone ophthalmoscopy with slit-lamp biomicroscopy for grading diabetic retinopathy. Am J Ophthalmol. 2015;159(2):360–4 e1. doi:10.1016/j.ajo.2014.11.008
- Toy BC, Myung DJ, He L, et al. Smartphone-based dilated fundus photography and near visual acuity testing as inexpensive screening tools to detect referral warranted diabetic eye disease. Retina. 2016;36(5):1000–1008. doi:10.1097/IAE.0000000000000955
- Hu A, Damji KF. New open source 3-dimensional printed smartphone fundus imaging adaptor. Can J Ophthalmol. 2019;54(3):399–400. doi:10.1016/j.jcjo.2018.10.017
- Wang A. Head mounted digital camera for indirect ophthalmoscopy. Invest Ophthalmol Vis Sci. 2014;55(13):1606.
- Karakaya M, Hacisoftaoglu RE. Comparison of smartphone-based retinal imaging systems for diabetic retinopathy detection using deep learning. BMC Bioinform. 2020;21(Suppl 4):259. doi:10.1186/s12859-020-03587-2
- Vilela MA, Valenca FM, Barreto PK, Amaral CE, Pellanda LC. Agreement between retinal images obtained via smartphones and images obtained with retinal cameras or fundoscopic exams - systematic review and meta-analysis. Clin Ophthalmol. 2018;12:2581–2589. doi:10.2147/OPTH.S182022
- Goyal A, Gopalakrishnan M, Anantharaman G, Chandrashekharan DP, Thachil T, Sharma A. Smartphone guided wide-field imaging for retinopathy of prematurity in neonatal intensive care unit - a Smart ROP (SROP) initiative. Indian J Ophthalmol. 2019;67(6):840–845. doi:10.4103/ijo.IJO_1177_18
- Lekha T, Ramesh S, Sharma A, Abinaya G. MII RetCam assisted smartphone based fundus imaging for retinopathy of prematurity. Indian J Ophthalmol. 2019;67(6):834–839. doi:10.4103/ijo.IJO_268_19
- Rajalakshmi R, Subashini R, Anjana RM, Mohan V. Automated diabetic retinopathy detection in smartphone-based fundus photography using artificial intelligence. Eye (Lond). 2018;32(6):1138–1144. doi:10.1038/s41433-018-0064-9
- Natarajan S, Jain A, Krishnan R, Rogye A, Sivaprasad S. Diagnostic accuracy of community-based diabetic retinopathy screening with an offline artificial intelligence system on a smartphone. JAMA Ophthalmol. 2019;137(10):1182. doi:10.1001/jamaophthalmol.2019.2923
- Hacisoftaoglu RE, Karakaya M, Sallam AB. Deep learning frameworks for diabetic retinopathy detection with smartphone-based retinal imaging systems. Pattern Recognit Lett. 2020;135:409–417. doi:10.1016/j.patrec.2020.04.009
- Lowe J, Cleland CR, Mgaya E, et al. The arclight ophthalmoscope: a reliable low-cost alternative to the standard direct ophthalmoscope. J Ophthalmol. 2015;2015:1–6. doi:10.1155/2015/743263
- Hytiris ML, Fioratou E, Gillan SN. The arclight vs. traditional ophthalmoscope: a cross-over trial. Eye. 2021;35(3):831–837. doi:10.1038/s41433-020-0972-3
- Wintergerst MWM, Jansen LG, Holz FG, Finger RP. Smartphone-based fundus imaging-where are we now? Asia Pac J Ophthalmol (Phila). 2020;9(4):308–314. doi:10.1097/APO.0000000000000303
- Saleem SM, Pasquale LR, Sidoti PA, Tsai JC. Virtual ophthalmology: telemedicine in a COVID-19 era. Am J Ophthalmol. 2020;216:237–242. doi:10.1016/j.ajo.2020.04.029
- Bifolck E, Fink A, Pedersen D, Gregory T. Smartphone imaging for the ophthalmic examination in primary care. JAAPA. 2018;31(8):34–38. doi:10.1097/01.JAA.0000541482.54611.7c
- Kelly LP, Garza PS, Bruce BB, Graubart EB, Newman NJ, Biousse V. Teaching ophthalmoscopy to medical students (the TOTeMS Study). Am J Ophthalmol. 2013;156(5):1056–1061 e10. doi:10.1016/j.ajo.2013.06.022
- Adam MK, Brady CJ, Flowers AM, et al. Quality and diagnostic utility of mydriatic smartphone photography: the smartphone ophthalmoscopy reliability trial. Ophthalmic Surg Lasers Imaging Retina. 2015;46(6):631–637. doi:10.3928/23258160-20150610-06
- Lamirel C, Bruce BB, Wright DW, Delaney KP, Newman NJ, Biousse V. Quality of nonmydriatic digital fundus photography obtained by nurse practitioners in the emergency department: the FOTO-ED Study. Ophthalmology. 2012;119(3):617–624. doi:10.1016/j.ophtha.2011.09.013
- Wu AR, Fouzdar-Jain S, Suh DW. Comparison study of funduscopic examination using a smartphone-based digital ophthalmoscope and the direct ophthalmoscope. J Pediatr Ophthalmol Strabismus. 2018;55(3):201–206. doi:10.3928/01913913-20180220-01
- Kim Y, Chao DL. Comparison of smartphone ophthalmoscopy vs conventional direct ophthalmoscopy as a teaching tool for medical students: the COSMOS Study. Clin Ophthalmol. 2019;13:391–401. doi:10.2147/OPTH.S190922
- Batista MA, Gaglani SM. The future of smartphones in health care. Virtual Mentor. 2013;15(11):947–950. doi:10.1001/virtualmentor.2013.15.11.stas1-1311
- Sharma N, Advani U, Sharma L, Jain M, Sharma K, Dixit A. Pattern of mobile phone usage among medical students. Int J Acad Med. 2019;5(2):118. doi:10.4103/IJAM.IJAM_61_18
- Tran TM, Huang NT, Montezuma SR. Smartphone funduscopy - how to use smartphone to take fundus photographs. Available from: https://eyewiki.aao.org/Smartphone_Funduscopy-How_to_use_smartphone_to_take_fundus_photographs. Accessed March 27, 2021.
- Ho DK-H, Morgan JE. Fundoscopy among novice users: comparing between direct ophthalmoscope and PEEK retina. Available from: https://www.oxfordeyesurgery.com/wp-content/uploads/2019/06/PEEK-study-OMG-meeting- poster.pdf. Accessed March 28, 2021
- Nagra M, Huntjens B. Smartphone ophthalmoscopy: patient and student practitioner perceptions. J Med Syst. 2019;44(1):10. doi:10.1007/s10916-019-1477-0
- Parthasarathy MK, Faruq I, Arthurs E, Lakshminarayanan V. Comparison of the efficacy of three direct ophthalmoscopes: a clinical study. Int Soc Opt Eng Photonics. 2019;111040T.
- Rai AS, Mavrikakis E, Lam WC, Lam WC. Teaching binocular indirect ophthalmoscopy to novice residents using an augmented reality simulator. Can J Ophthalmol. 2017;52(5):430–434. doi:10.1016/j.jcjo.2017.02.015
- Lippa LM, Boker J, Duke A, Amin A. A novel 3-year longitudinal pilot study of medical students’ acquisition and retention of screening eye examination skills. Ophthalmology. 2006;113(1):133–139. doi:10.1016/j.ophtha.2005.09.003
- Cordeiro MF, Jolly BC, Dacre JE. The effect of formal instruction in ophthalmoscopy on medical student performance. Med Teach. 1993;15(4):321–325. doi:10.3109/01421599309006654
- Gupta RR, Lam WC. Medical students’ self-confidence in performing direct ophthalmoscopy in clinical training. Can J Ophthalmol. 2006;41(2):169–174. doi:10.1139/I06-004
- Schulz C, Hodgkins P. Factors associated with confidence in fundoscopy. Clin Teach. 2014;11(6):431–435. doi:10.1111/tct.12171
- Schulz C, Moore J, Hassan D, Tamsett E, Smith CF. Addressing the ‘forgotten art of fundoscopy’: evaluation of a novel teaching ophthalmoscope. Eye (Lond). 2016;30(3):375–384. doi:10.1038/eye.2015.238
- Milani BY, Majdi M, Green W, et al. The use of peer optic nerve photographs for teaching direct ophthalmoscopy. Ophthalmology. 2013;120(4):761–765. doi:10.1016/j.ophtha.2012.09.020
- Gilmour G, McKivigan J. Evaluating medical students’ proficiency with a handheld ophthalmoscope: a pilot study. Adv Med Educ Pract. 2017;8:33–36. doi:10.2147/AMEP.S119440
- Larsen P, Stoddart H, Griess M. Ophthalmoscopy using an eye simulator model. Clin Teach. 2014;11(2):99–103. doi:10.1111/tct.12064
- Hoeg TB, Sheth BP, Bragg DS, Kivlin JD. Evaluation of a tool to teach medical students direct ophthalmoscopy. WMJ. 2009;108(1):24–26.
- Ricci LH, Ferraz CA. Ophthalmoscopy simulation: advances in training and practice for medical students and young ophthalmologists. Adv Med Educ Pract. 2017;8:435–439. doi:10.2147/AMEP.S108041
- Myung D, Jais A, He L, Chang RT. Simple, low-cost smartphone adapter for rapid, high quality ocular anterior segment imaging: a photo diary. J Mob Technol Med. 2014;3:2–8. doi:10.7309/jmtm.3.1.2
- Blaikie A, Sandford-Smith J, Tuteja SY, Williams CD, O’Callaghan C. Arclight: a pocket ophthalmoscope for the 21st century. BMJ. 2016;355:i6637. doi:10.1136/bmj.i6637
- Mamtora S, Sandinha MT, Ajith A, Song A, Steel DHW. Smart phone ophthalmoscopy: a potential replacement for the direct ophthalmoscope. Eye (Lond). 2018;32(11):1766–1771. doi:10.1038/s41433-018-0177-1
- Duyongco KL, Arroyo MH, Caparas VL, Silva PS. Dilated smartphone imaging for the detection and grading of diabetic retinopathy. Med City J. 2018;1(1).
- Mackay DD, Garza PS, Bruce BB, et al. Teaching ophthalmoscopy to medical students (TOTeMS) II: a one-year retention study. Am J Ophthalmol. 2014;157(3):747–748. doi:10.1016/j.ajo.2013.12.013
- Bruce BB, Bidot S, Hage R, et al. Fundus photography vs. ophthalmoscopy outcomes in the emergency department (FOTO-ED) phase III: web-based, in-service training of emergency providers. Neuroophthalmology. 2018;42(5):269–274. doi:10.1080/01658107.2017.1419368

![Figure 4 Appropriateness of smartphone funduscopy (SF) and direct ophthalmoscopy (DO). (A) Proportion of medical students preferring SF (0.24), DO (0.69) or indifferent (0.07). (B) Comfort level of student being examined. Median [interquartile range] for SF is 4[3–5] and DO is 4[4–5], p < 0.001.](/cms/asset/c64c4795-8c16-4183-9ffe-baafcd1b7a39/doph_a_12177087_f0004_b.jpg)