Abstract
Purpose
To evaluate the rotational stability of the three monofocal toric intraocular lenses (IOLs) via data from an online toric IOL back-calculator.
Methods
A retrospective data review of an online toric IOL back-calculator, which allows users to input preoperative toric planning information, postoperative lens orientation, and subjective refraction. Inputted data were used to determine the optimal orientation of the toric IOL to minimize residual refractive astigmatism. Aggregate data from 3/11/2019 to 3/10/2020 were extracted and validated. Only data with ≥0.5D of residual refractive astigmatism were used in the study. Pre-operative intended IOL orientation and post-operative IOL orientation were used to calculate IOL rotation.
Results
After validation, 5397 entries were determined to represent patient eyes, of which 3238 represented the three monofocal IOLs evaluated. The rate of rotation for AcrySof, TECNIS, and enVista Toric IOLs was 72.7%, 83.4%, and 83.0%, respectively, and location only significantly impacted TECNIS IOLs. The magnitude of rotation for rotated IOLs was similar for all models and was significantly more for IOLs initially placed in the oblique axis. All IOL models tended to rotate in a counterclockwise direction (53.2%, 73.0%, 69.7%, respectively; p<0.05), and the tendency was greater for IOLs initially located horizontally.
Conclusion
The AcrySof IQ Toric IOL was more rotationally stable than both the TECNIS and enVista Toric IOLs; there was no significant difference in rotational stability of the latter two.
Keywords:
Introduction
The majority of patients undergoing cataract surgery have a visually significant amount of anterior corneal astigmatism. In 2010, Hoffman et al published biometry data from 23,239 eyes which showed 73.7% had ≥0.5D of anterior corneal astigmatism, and over a third (36.05%) had ≥1.0D of astigmatism.Citation1 Toric intraocular lenses (IOLs), first approved by the US Food and Drug Administration (FDA) in 1998, are an effective way of reducing corneal astigmatism for these patients at the time of cataract surgery.Citation2 A visually significant amount of residual astigmatism after placement of a toric IOL may leave patient and surgeon alike unsatisfied and frustrated.
Residual refractive astigmatism occurs when a toric IOL has the wrong amount of cylinder power or is misaligned. A major cause of toric misalignment is post-operative rotation, which typically occurs soon after surgery.Citation3,Citation4 While the earliest models of toric IOLs frequently had significant postoperative rotation,Citation5–Citation8 modern models are much more rotationally stable.Citation2,Citation4,Citation9–Citation14 However, significant postoperative rotation can still occur.
In 2018, the enVista® toric (MX60T; Bausch & Lomb, Rochester, NY) was FDA approved.Citation15 Initial rotational rates (>5°) for this IOL have ranged from 9.5% to 23%.Citation11,Citation16,Citation17 One study compared rotational rates of the enVista Toric (n=21) to the AcrySof® IQ Toric (n=28) (Alcon Vision LLC, Fort Worth, TX), and Lentis LT (n=14) (Oculentis, Berlin, Germany); rotation ≥5° occurred in 9.5%, 35.7%, and 35.4%, respectively. The enVista Toric IOL was found to be the most rotationally stable of the three; however, the study was small and statistical significance was not reported for these specific findings.Citation16
The purpose of the current study was to use a large database to further evaluate and compare rotational characteristics of three monofocal toric IOLs available in the US: enVista, AcrySof IQ, and TECNIS® Toric (Johnson & Johnson, New Brunswick, NJ).
Patients and Methods
This analysis was based on data input to an online toric back calculator (www.astigmatismfix.com; hereinafter “AstigmatismFix”) which was designed to assist surgeons in managing residual refractive astigmatism after surgical placement of a toric IOL. The University of North Carolina Office of Human Research Ethics was contacted regarding this study and determined that it did not constitute as human subjects research as defined under federal regulation and further Institutional Review Board approval was unnecessary. No patient identifying data is stored from the website, therefore all data accessed complied with relevant data protection and privacy regulations.
Raw data from AstigmatismFix were collected from 3/11/2019 through 3/10/2020. The start date was determined by the first enVista Toric IOL entry being made on 3/11/2019, and the study lasted 1 year. The data were then validated using data filters listed in . If a user with the same first and last name made multiple entries within a single calendar day, only the first of those entries was used in the final dataset to prevent over representation of a single case. A similar method of data validation was used with the AstigmatismFix data sets in previous studies.Citation18–Citation22
Box 1 Validation Criteria
The amount of rotation was calculated by taking the difference of the pre-operative intended IOL orientation and the post-operative IOL orientation. An IOL was said to have rotated if this difference was ≥5°. To determine rotation direction (clockwise vs counterclockwise), it was assumed the IOL rotated <90°. A subset analysis was performed by stratifying results based on the intended IOL location. IOLs were said to be with-the-rule (WTR) when located ≥60° to <120°, against-the-rule (ATR) when located ≥0° to <30° and ≥150° to <180°, and oblique when located ≥30° to <60° and ≥120° to <150°.
All data validation, calculations, and statistical analyses were performed via Microsoft® Excel for Mac (Version 16.35; Microsoft Corporation, Redmond, WA). For rotation frequency, odds ratios were calculated and chi-square tests were performed; for magnitude of rotation, analysis of variance (ANOVA) and equal variance two-tailed Student’s t-tests were conducted; for rotation direction, a one-proportion z-test with the probability of clockwise or counter-clockwise rotation set at 50%. Statistical significance was set at p < 0.05.
Results
There was a total of 26,949 AstigmatismFix entries between 3/11/2019 and 3/10/2020. After validation, 5397 entries were determined to represent actual cases. Three monofocal toric IOL models were identified and used in the final dataset: AcrySof IQ Toric, TECNIS Toric, and enVista Toric. Characteristics of this final dataset of 3238 toric IOLs can be seen in .
Table 1 Dataset Characteristics
Rotation Frequency
The rate of rotation ≥5° was 77.4% (4177/5397) for the entire validated dataset, and 77.7% (2517/3238) when only considering the three monofocal IOLs listed above. The rotation rate for the AcrySof, TECNIS, and enVista toric IOLs was 72.7% (1240/1706), 83.4% (1091/1308), and 83.0% (186/224) respectively. Comparison of rotation rates for the three IOLs can be seen in , where it is shown that the AcrySof toric IOL rotated significantly less frequently than both the TECNIS (p<0.001) and enVista (p=0.0011) toric IOLs. There was no statistical difference in rotation between the TECNIS and enVista toric models. Rotation rates for each IOL at multiple cutoff points can be seen in .
Table 2 Comparison of Toric IOL Rotation (≥5°)
Table 3 Rotation Rates for Three Toric IOLs at Multiple Cut-Points
Rotation Magnitude
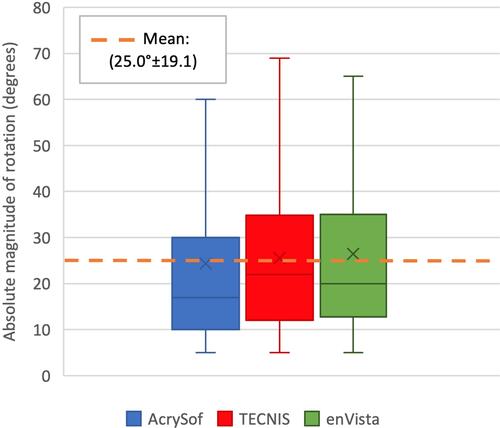
A subset analysis which included the 2517 IOLs that rotated was performed to determine the average magnitude of rotation. There was no statistical difference in magnitude of rotation for the three IOL models ().
Figure 1 Box and whisker plot of the magnitude of rotation for each IOL model. Only IOLs which rotated ≥5° were considered in this subset analysis. ANOVA showed no statistical difference between the three groups when considered as a whole (p=0.176). A two-tailed, equal variance Student’s t-test was performed and showed no difference when comparing the groups head-to-head. (AcrySof v. TECNIS p=0.126; AcrySof v. enVista p=0.191; TECNIS v. enVista p=0.513).
Rotation Direction
Another subset analysis which excluded IOLs that did not rotate in addition to 15 IOLs located orthogonal from their intended location was performed to determine any bias in rotation direction (n=2502). The AcrySof, TECNIS, and enVista Toric IOLs all had a bias toward counterclockwise (CCW) rotation (53.2%, 73.0%, and 69.7%, respectively) (p<0.05).
Location
The above findings of frequency, magnitude, and direction of IOL rotation were stratified by the intended IOL location and can be seen in . The major findings were as follows: 1) TECNIS IOLs placed ATR appear to rotate less than those placed WTR or oblique; 2) when IOLs rotate, those placed obliquely rotate at higher magnitudes (); 3) when IOLs rotate, those placed ATR favor counterclockwise rotation more so than those placed WTR or obliquely.
Table 4 Effects of IOL Location
Discussion
When considering the results of this study, it is crucial to understand that its population consists solely of cases of residual astigmatism, and therefore the frequency of rotation is largely overestimated compared to the population of total implanted toric IOLs. However, this database and method were used previously to compare rotation rates of IOL models,Citation18 and those findings were later supported by additional publications.Citation4,Citation23 Only one known study previously compared the rotation rate of the enVista Toric IOL to others, and the results showed enVista was more rotationally stable than the AcrySof and Lentis LT IOLs. Although this study was small (n=63, for monofocal toric IOLs) and statistical significance was not reported for rotation frequency. This study found the opposite; both the enVista and TECNIS IOLs were 1.84x and 1.89x more likely to rotate than the AcrySof IOL (p<0.05). The rotational stability of AcrySof IOLs compared to TECNIS IOLs is similar to that found in previous studies,Citation4,Citation18,Citation23 and this is the first known comparison of the TECNIS and enVista IOLs, of which there was no statistical difference. Variability in rotational stability among different IOL models is thought to be due to either IOL design or material, although an exact mechanism has yet to be proven. Johnson & Johnson has addressed the rotational instability of the TECNIS IOL by launching the TECNIS Toric II in late 2019, which has squared and frosted edges at the end of the haptic.Citation24 Bausch & Lomb is also in the process of transitioning from the MX60T to the MX60ET. The rotational stability of these newer IOL versions has yet to be published.
The location in which IOLs are placed has also been shown to affect the frequency of rotation.Citation4,Citation25 In this study, location only significantly affected the rotation rate in the TECNIS group, which showed IOLs initially placed vertically (WTR) or obliquely rotated more than those placed horizontally (ATR). The anatomy of the capsular bag or gravity may play a role in this slight predisposition.
A tendency to rotate counterclockwise has been described for both TECNIS and enVista IOLs.Citation4,Citation16,Citation18,Citation23 This was also found to be true in this study (). Regarding AcrySof IOLs, there is no consensus, as clockwise (CW),Citation16,Citation25,Citation26 CCW,Citation23 and no directionCitation18,Citation27 tendencies have been described. In this study, there was a slight tendency for AcrySof IOLs to rotate CCW (53.2%). When considering the initial location of the IOL, there is a clear tendency for IOLs located horizontally (ATR) to rotate CCW for all IOLs (). While all locations still had a bias toward CCW rotation for TECNIS and enVista (note: WTR and oblique enVista categories failed to reach statistical significance), for AcrySof each category was different; horizontal (ATR) IOLs tended to rotate CCW, vertical (WTR) CW, and oblique did not have a bias. This may explain the conflicting literature regarding AcrySof IOLs as Miyake et al, who showed a CW tendency, had 100% of IOLs initially located vertically, and Oshika et al, who showed a CCW tendency, had 72% of IOLs initially located horizontally.Citation23,Citation25 The tendency for AcrySof IOLs located vertically (WTR) to rotate CW and horizontally (ATR) to rotate CCW seems to support the findings of Lee et al, although a specific statistical analysis regarding this was not performed in their study.Citation4
Figure 2 Stacked bar graph of the direction of rotation. A one-proportion z-test was performed with the expected amount of IOLs rotating counterclockwise set at 50%. * denotes groups which were statistically different (p<0.05).
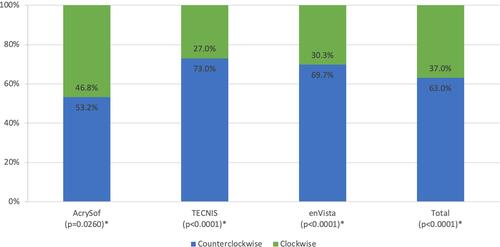
Figure 3 Box and whisker plot of the magnitude of rotation stratified by IOL model and intended IOL location. Via ANOVA, the intended IOL location effected magnitude significantly in the AcrySof (p=0.0415) and TECNIS (p<0.001) groups, but not the enVista group (p=0.382). This was largely due to the increased magnitude of rotation for IOLs located obliquely, and there were only 17 enVista entries in this subset.
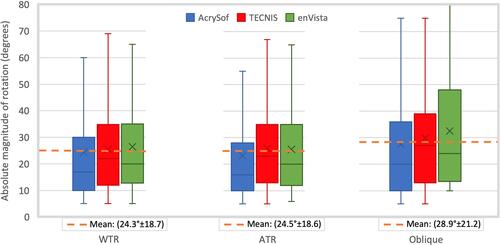
The magnitude of rotation was greater in IOLs initially placed obliquely, which to our knowledge has not been shown before, and was similar for all three IOL models.
Limitations of the study include that AstigmatismFix was not created for the purpose of conducting research, rather it is a freely available tool designed with the primary goal of helping surgeons manage post-operative residual astigmatism in patients who received a toric IOL. Prompts have been added to the website that allows users to label repeat and theoretical entries; however, even with these additions and the rigorous validation criteria described above, there is noise within the data. Regarding rotation calculations, the assumption was made that the surgeon accurately placed the IOL where they intended to, and therefore any postoperative misalignment was secondary to IOL rotation. It is also possible that postoperative misalignment was due to intraoperative misplacement. However, there is no reason to believe users of any particular toric IOL model would be more or less likely to misplace them, and therefore this unlikely skewed any results. It has also been shown that the majority of postoperative misalignment is in fact due to rotation.Citation3 The enVista group was much smaller than the AcrySof and TECNIS groups. Further controlled studies should be performed to confirm these findings.
Disclosure
All authors receive grant funding from Alcon Vision LLC. David R Hardten and John P Berdahl are owners of Ocular Surgical Data LLC. John P Berdahl receives personal fees from Alcon Vision LLC, Johnson & Johnson, and Bausch & Lomb. The authors report no other conflicts of interest in this work.
Additional information
Funding
References
- Hoffmann PC, Hutz WW. Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg. 2010;36(9):1479–1485. doi:10.1016/j.jcrs.2010.02.025
- Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016;123(2):275–286. doi:10.1016/j.ophtha.2015.10.002
- Inoue Y, Takehara H, Oshika T. Axis misalignment of toric intraocular lens: placement error and postoperative rotation. Ophthalmology. 2017;124(9):1424–1425. doi:10.1016/j.ophtha.2017.05.025
- Lee BS, Chang DF. Comparison of the rotational stability of two toric intraocular lenses in 1273 consecutive eyes. Ophthalmology. 2018;125(9):1325–1331. doi:10.1016/j.ophtha.2018.02.012
- Chang DF. Comparative rotational stability of single-piece open-loop acrylic and plate-haptic silicone toric intraocular lenses. J Cataract Refract Surg. 2008;34(11):1842–1847. doi:10.1016/j.jcrs.2008.07.012
- Maedel S, Hirnschall N, Chen YA, Findl O. Rotational performance and corneal astigmatism correction during cataract surgery: aspheric toric intraocular lens versus aspheric nontoric intraocular lens with opposite clear corneal incision. J Cataract Refract Surg. 2014;40(8):1355–1362. doi:10.1016/j.jcrs.2013.11.039
- Chang DF. Early rotational stability of the longer Staar toric intraocular lens: fifty consecutive cases. J Cataract Refract Surg. 2003;29(5):935–940. doi:10.1016/S0886-3350(02)01843-6
- Chua WH, Yuen LH, Chua J, Teh G, Hill WE. Matched comparison of rotational stability of 1-piece acrylic and plate-haptic silicone toric intraocular lenses in Asian eyes. J Cataract Refract Surg. 2012;38(4):620–624. doi:10.1016/j.jcrs.2011.10.037
- Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM. The AcrySof Toric intraocular lens in subjects with cataracts and corneal astigmatism: a randomized, subject-masked, parallel-group, 1-year study. Ophthalmology. 2010;117(11):2104–2111. doi:10.1016/j.ophtha.2010.07.033
- Waltz KL, Featherstone K, Tsai L, Trentacost D. Clinical outcomes of TECNIS toric intraocular lens implantation after cataract removal in patients with corneal astigmatism. Ophthalmology. 2015;122(1):39–47. doi:10.1016/j.ophtha.2014.06.027
- Packer M, Williams JI, Feinerman G, Hope RS. Prospective multicenter clinical trial to evaluate the safety and effectiveness of a new glistening-free one-piece acrylic toric intraocular lens. Clin Ophthalmol. 2018;12:1031–1039. doi:10.2147/OPTH.S167726
- Ahmed II, Rocha G, Slomovic AR, et al. Visual function and patient experience after bilateral implantation of toric intraocular lenses. J Cataract Refract Surg. 2010;36(4):609–616. doi:10.1016/j.jcrs.2009.10.044
- Visser N, Ruiz-Mesa R, Pastor F, Bauer NJ, Nuijts RM, Montes-Mico R. Cataract surgery with toric intraocular lens implantation in patients with high corneal astigmatism. J Cataract Refract Surg. 2011;37(8):1403–1410. doi:10.1016/j.jcrs.2011.03.034
- Visser N, Beckers HJ, Bauer NJ, et al. Toric vs aspherical control intraocular lenses in patients with cataract and corneal astigmatism: a randomized clinical trial. JAMA Ophthalmol. 2014;132(12):1462–1468. doi:10.1001/jamaophthalmol.2014.3602
- FDA US. enVista® one piece hydrophobic acrylic toric intraocular lens - P910056/S027. 2018 Accessed March 27, 2020.
- Garzon N, Poyales F, de Zarate BO, Ruiz-Garcia JL, Quiroga JA. Evaluation of rotation and visual outcomes after implantation of monofocal and multifocal toric intraocular lenses. J Refract Surg. 2015;31(2):90–97. doi:10.3928/1081597X-20150122-03
- Vokrojova M, Havlickova L, Brozkova M, Hlinomazova Z. Effect of capsular tension ring implantation on postoperative rotational stability of a toric intraocular lens. J Refract Surg. 2020;36(3):186–192. doi:10.3928/1081597X-20200120-01
- Potvin R, Kramer BA, Hardten DR, Berdahl JP. Toric intraocular lens orientation and residual refractive astigmatism: an analysis. Clin Ophthalmol. 2016;10:1829–1836. doi:10.2147/OPTH.S114118
- Potvin R, Kramer BA, Hardten DR, Berdahl JP. Factors associated with residual astigmatism after toric intraocular lens implantation reported in an online toric intraocular lens back-calculator. J Refract Surg. 2018;34(6):366–371. doi:10.3928/1081597X-20180327-01
- Kramer BA, Berdahl JP, Hardten DR, Potvin R. Residual astigmatism after toric intraocular lens implantation: analysis of data from an online toric intraocular lens back-calculator. J Cataract Refract Surg. 2016;42(11):1595–1601. doi:10.1016/j.jcrs.2016.09.017
- Berdahl JP, Hardten DR, Kramer BA, Potvin R. The effect of lens sphere and cylinder power on residual astigmatism and its resolution after toric intraocular lens implantation. J Refract Surg. 2017;33(3):157–162. doi:10.3928/1081597X-20170105-01
- Berdahl JP, Hardten DR, Kramer BA, Potvin R. Effect of astigmatism on visual acuity after multifocal versus monofocal intraocular lens implantation. J Cataract Refract Surg. 2018;44(10):1192–1197. doi:10.1016/j.jcrs.2018.06.048
- Oshika T, Fujita Y, Hirota A, et al. Comparison of incidence of repositioning surgery to correct misalignment with three toric intraocular lenses. Eur J Ophthalmol. 2020;30:680–684.
- J&JVision. TECNIS® Toric II IOL. 2020. Available from: https://www.jnjvisionpro.com/products/tecnis%C2%AE-toric-ii-iol. Accessed March 31, 2020.
- Miyake T, Kamiya K, Amano R, Iida Y, Tsunehiro S, Shimizu K. Long-term clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatism. J Cataract Refract Surg. 2014;40(10):1654–1660. doi:10.1016/j.jcrs.2014.01.044
- Shah GD, Praveen MR, Vasavada AR, Vasavada VA, Rampal G, Shastry LR. Rotational stability of a toric intraocular lens: influence of axial length and alignment in the capsular bag. J Cataract Refract Surg. 2012;38(1):54–59. doi:10.1016/j.jcrs.2011.08.028
- Zuberbuhler B, Signer T, Gale R, Haefliger E. Rotational stability of the AcrySof SA60TT toric intraocular lenses: a cohort study. BMC Ophthalmol. 2008;8:8. doi:10.1186/1471-2415-8-8
