Abstract
Presbyopia, a loss of accommodative ability associated with aging, is a significant cause of vision impairment globally. At the clinical level, it is a frustrating and difficult issue that negatively impacts patients’ quality of life. Less appreciated is the fact that loss of accommodative ability and its current treatments methods may present safety concerns, for example, increasing the risk of falls. Therefore, a more complete understanding of treatment options with respect to how they relate to the natural ability of the eye is needed to improve decision making and to aid clinicians in individualizing treatment options. This article reviews the options for expanding functional through focus—a term coined to describe the ability of the eye to see at all distances with minimal latency—by how they vary the refractive power over time, across the visual field, between eyes, or across a range of distances.
Graphical abstract

Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
The loss of accommodation, a natural part of the lenticular aging process and the first stage of Dysfunctional Lens Syndrome,Citation1 is a significant cause of vision impairment suggested to affect about one-quarter of the world’s population.Citation2 Globally, there are an estimated 1.8 billion people with presbyopia, including 128 million people in the US alone.Citation2 The average age of onset is generally between 40 and 45 yearsCitation3 and varies depending on climate, heritage,Citation4 and other individual factors.Citation5–Citation7 The burden of uncorrected presbyopia is significant, accounting for near vision impairment in an estimated 826 million people globally,Citation2 resulting in an estimated $25 billion loss in productivity among individuals younger than 65 years.Citation8 With increasing longevity, most people in the western world will spend almost half of their lives as presbyopes.Citation9 It is a condition that results in loss of productivity and quality of life,Citation10,Citation11 and may create safety concerns,Citation12 suggesting it should be treated as an important medical need rather than as a lifestyle decision.
Accommodation describes the mechanism by which the eye varies refractive power to focus on objects at different distances to provide the retina a clear, sharp image.Citation13 Thomas Young is widely credited with confirming that the crystalline lens is the primary anatomical structure responsible for accommodationCitation14 (reviewed in 15)Citation15 and Helmholtz later described the role of ciliary muscle contraction and relaxation of the zonules in inducing lens thickening and curvature, which contribute to increased refractive power.Citation16 Glasser and Kaufman subsequently verified that the movement of the accommodative structures was most consistent with the Helmholtz theory.Citation17 More recently, the interrelationship of the zonular apparatus’ components has been visually described in a computer-animated model by Goldberg.Citation18 By extension, a loss of accommodative amplitude due to changes in these and other anatomic structures secondary to aging manifests as presbyopia.Citation19 Taken together, this evidence highlights that presbyopia is a phenomenon resulting from losing the ability to accommodate,Citation20 and, consequently, that the goal of treating presbyopia is to compensate for this inability. However, to our knowledge, there is no universally accepted word or term to describe the objective of accommodation: to see in clear focus at any distance with low or no latency. In this review, we will use the term “functional through focus with imperceptible latency” (or “functional through focus”) to describe this concept. According to the definition presented here, presbyopia can thus be thought of as a loss of functional through focus.
There are often tradeoffs associated with manipulating the optical system, particularly when dealing with the complexity and dynamic nature of accommodation. For example, increasing depth of field using multifocal intraocular lenses may result in loss of visual quality and contrast sensitivity.Citation21,Citation22 Other approaches can be associated with more severe unintended effects. For example, multifocal spectacles increase the risk of falls in elderly individuals.Citation23 A fuller understanding of the risks and benefits associated with various treatment approaches, beyond those that may be treatment related, requires a new way to think about them. As such, this article proposes a new system of classifying presbyopia interventions according to their mechanism of action.
Background and Rationale
Currently, presbyopia treatments are characterized according to the device used (ie, glasses and contact lenses) and/or the procedure performed (ie, corneal refractive surgery and lenticular refractive surgery). This method-based classification is logical for historical and clinical purposes, facilitating at least a basic understanding of efficacy and safety outcomes related to the method of treatment. However, it provides little insight into the optical effects experienced by a given patient and thus little utility for prospective clinical decision making based on a patient’s previous experience with presbyopia treatments. On the other hand, a more meaningful comparison would follow from classification by mechanism of action for achieving functional through focus. This would lend itself to a better understanding of the optical principles leveraged by a given intervention and the advantages and disadvantages associated with that mechanism.
Fundamentally, restoring functional through focus requires a varying of refractive power so that objects at different distances can be brought into focus with minimal latency. This can be achieved by leveraging at least one of four mechanisms that expand functional through focus by varying the refractive power (1) over time, (2) across the visual field, (3) between eyes, or (4) across a range of distances. These mechanisms can be used alone or in combination. The methods used to achieve the given mechanism of correction may be permanent or impermanent and can be applied at different extraocular or intraocular locations (eg, non-contact, on the surface, on the cornea, and intraocularly), which may or may not correspond to the location of the mechanistic effect ().
Table 1 Overview of Mechanisms for Correcting Presbyopia Subcategorized by Method, The Area of the Eye Where the Mechanism Has Effect (“M”), and Location of Application (“A”)
Considering the mechanism of action in the manner we propose provides a practical framework to understand the inherent advantages and disadvantages associated with treatment options, independent of the specific mode of intervention used to implement that mechanism (). For example, monovision leverages the mechanism of varying the refractive state between eyes. While there are subtle differences, the fundamental advantages and disadvantages of monovision are the same whether achieved via contact lenses, laser vision correction, or intraocular lenses (IOLs). As a result, a patient who is intolerant of monovision with contact lenses would likely not tolerate monovision with IOLs because both interventions share the same fundamental mechanism of action. Recognizing the underlying mechanism of action would allow a clinician to use a patient’s previous presbyopia treatment experience as a factor in clinical decision making.
Table 2 Relative Advantages and Disadvantage of Differing Approaches for Varying Refractive Power to Achieve Functional Through Focus
Varying Refractive Power Over Time
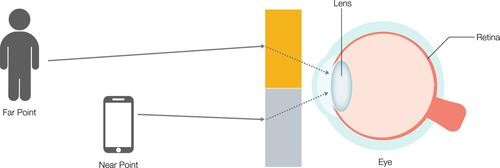
In the human visual system, focus is achieved when light from an object of regard is focused on the fovea (). As the eye regards objects at different distances, functional through focus describes the ability of the eye to adjust the refractive power to bring the object into focus at the given distance. This mechanism is the only one that can facilitate uncompromised vision at any given distance.
Figure 1 Varying the refractive power over time describes the eye’s natural ability to shift focus from far objects (person) at time 1 (t1) to near (smartphone) at time 2 (t2).

Accommodation is the natural mechanism to achieve functional through focus with imperceptible latency. Helmholtz proposed that circumferential ciliary muscle contraction releases zonular tension, allowing the lens capsule to contract, increasing lens surface curvature, thus providing the dioptric power necessary for near visual tasks.Citation16 This ability is reduced as the lens stiffens and becomes dysfunctional with age.
Interventions
Presbyopia is the loss of the eye’s ability to vary the refractive power.Citation19 Depending on the stage of presbyopia different approaches can be used to enhance or recreate this mechanism for creating functional through focus. Early in the progression of presbyopia, the residual accommodative amplitude can be enhanced; but in later stages, the only way to recreate the ability to vary refractive power over time is through artificial means.
Spectacles are the simplest method for changing the refractive state over time. While using different glasses for far and near visual tasks mechanistically varies the refractive power over time, it by necessity entails significant perceptible latency. Nonsurgical approaches include an eye drop that exerts ciliary muscle contraction as one of its mechanism for accentuating accommodation. Another pharmaceutical option dissolves disulfide bonds, returning the lens to a more flexible state, thereby allowing for natural accommodative ability.Citation24 Electrostimulation is a nonpharmaceutical approach for reviving ciliary muscle contraction.Citation25
Laser options include scleral laser micro-excision, in which an Er:YAG laser is applied to increase plasticity and compliance of the scleral tissue to facilitate contraction of the ciliary muscles, and femtosecond laser manipulation of the lens to increase its deformability, and thus accommodative ability.Citation26,Citation27 Other surgical options include implants which increase the area between the ciliary muscle and the sclera to restore accommodation.Citation28
Accommodating IOLs (AIOLs) are intended to create a progressive change in power in relation to the active contraction of the ciliary body.Citation29,Citation30 Various design approaches including hinged, dual optic, bioanalogic polyfocal, and fluid optic designs have been studied.Citation31–Citation33
Advantages and Disadvantages
By varying the refractive power over time, objects at any distance can be seen in full focus by the full visual field of both eyes. Visual distortions, breaks in the visual field, and monocular disparity are theoretically avoided. For these reasons, restoration of natural accommodation or creation of artificial accommodation would conceptually be the ideal approach to treating presbyopia. Although no drug or device demonstrating true power change over time has received approval from the US Food and Drug Administration (FDA), one candidate pharmaceutical is currently undergoing review.
The technical challenges of creating a device that achieves functional through focus through accommodation are many, specifically automatically sensing the amount of accommodation needed; optically or mechanically varying the refractive power accordingly; and stability over time. All of this would need to be combined in a device with biocompatible materials implantable through a microincision at the time of lens extraction.
With no current FDA-approved presbyopia treatment in this category, it is not possible to assess safety and efficacy. The sole IOL to receive approval from the FDA with an accommodating label is the Crystalens IOL (Bausch & Lomb, Bridgewater, NJ). However, this lens demonstrates limited objective accommodative response movement on aberrometry.Citation34 Given that a convenient solution that varies the refractive state over time does not yet exist, patients have sought a variety of options that are more convenient, but which are associated with inherent compromises.
Varying Refractive Power Across the Visual Field
Broadly speaking, near visual tasks such as reading are typically performed in the lower visual field, while far tasks, such as driving and watching television, are performed using the central and upper visual field. Optical devices have been designed to leverage this tendency by providing different refractive powers corresponding to the direction of gaze (). In order to be effective, the device must move independently with respect to the eye’s direction of gaze.
Figure 2 Varying the refractive power across the field requires optics that utilize two or more focusing zones. In this example, representing a bifocal correction, objects at far (person) are focused by an optic powered for far (orange rectangle), and objects at near (smartphone) are focused by an optic powered for near (grey rectangle). The viewer must either move the optic itself or physically adjust the eye gaze to utilize the appropriate viewing zone.
Interventions
Multifocal spectacles are the prototypical example of a presbyopia treatment that varies the refractive power over the visual field. The invention of bifocal glasses is widely credited to Benjamin Franklin.Citation35 Since that time, there have been various multifocal designs, including but not limited to flat top, round top, trifocal, and progressive add lenses. Certain multifocal contact lenses, specifically those with a segmented design, also leverage this mechanism. Although they may move with the eye, on down gaze, the lower lid prevents full downward movement of the lens, thus allowing the visual axis to pass through the higher-powered portion of the lens.
Notably, although multizone IOLs with nonrotationally symmetric power distribution may appear to vary refractive state across the visual field, they in fact leverage pseudoaccommodative principles due to the fact that they do not move independently from the eye gaze.Citation36
Advantages and Disadvantages
Although a popular option, varying the refractive state across the visual field is associated with several drawbacks. Multifocal spectacles may require head and body movements when trying to focus on objects at different distances, and bifocal and trifocal spectacles may contribute to image jumps and distortions. Progressive add lenses offer a smoother transition in power, but outside of a narrow corridor along the lens surface, there is additional distortion.Citation37 Multifocal spectacles of all types cause decreased edge-contrast sensitivity and depth perception in the inferior visual field, making it difficult to judge object position and movement. This has been shown to significantly increase risk of accidents and falls in the elderly.Citation38 Direct medical costs due to falls attributable to multifocal spectacles are estimated to be approximately $11 billion annually in the US.Citation23
Similarly, multifocal contact lenses may result in visually problematic superimposition of images in settings of low contrast.Citation39 Moreover, a number of factors may impact patients’ ability to successfully wear contact lenses of any modality,Citation40 which undermines their reliability as a suitable option for long-term management of presbyopia. As well, multiple viewing zones can reduce image quality and may result in halos, glares, or reduced nighttime vision.Citation41–Citation43
Varying the Refractive Power Between Eyes
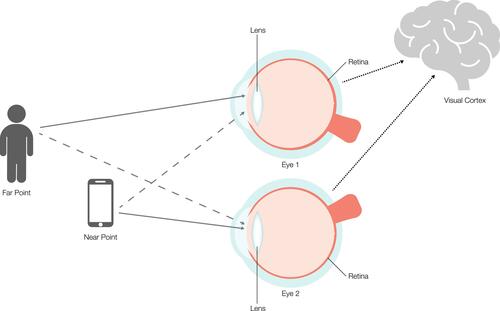
Natural binocularity provides redundancy in vision over all ranges with a slight parallax at near ranges, which the brain uses to facilitate depth perception.Citation44 Leveraging the redundancy and breaking binocularity via establishment of differing refractive powers between the two eyes thus provides a fuller range of vision.Citation45 Commonly referred to as monovision, varying the refractive state between eyes requires patients to employ binocular neural summation to add focused and defocused images in the visual cortex where non-linear summation or cross-eye neural inhibition is thought to reduce the visibility of the defocused image ().Citation46,Citation47
Figure 3 Varying the refractive power between eyes, or monovision, ultimately depends on binocular summation within the visual cortex of the brain. Objects at far (person) are focused by one eye (Eye 1) that is appropriately powered for viewing (indicated by a solid arrow) and a defocused image (indicated by a dashed arrow) is perceived by the fellow eye (Eye 2). The opposite is true for near objects (smartphone). The resulting image is reorganized via binocular neural summation to add focused and defocused images in the visual cortex.
Interventions
Monovision can be achieved using a variety of methods. In creating induced anisometropia, the refractive power of one eye (typically the dominant eye) is established for far vision while the contralateral eye is established for near. Contact lenses, while typically used to correct static refractive errors, naturally lend themselves to this mechanism. After determining the power required to establish emmetropia, a separate strategy is needed to determine the degree of controlled anisometropia required to treat the presbyopia. Of note, leveraging this mechanism is often coupled with some degree of varying the refractive power across a range of distances (ie, pseudoaccommodation) with concentric or aspheric multifocal contact lenses to achieve even greater through focus.
This mechanism can also be utilized through various surgical approaches. Functionally, corneal and lenticular refractive surgery have the same visual effect as contact lenses. In addition to correcting static refractive errors, LASIK, PRK, and IOLs can be used to vary the refractive power between eyes, thus improving through focus. As is the case with multifocal contact lenses, presby LASIK and certain IOLs leverage some degree of pseudoaccommodation to increase depth of focus.Citation28,Citation48
Advantages and Disadvantages
Monovision is relatively easy to implement and works for many individualsCitation49–Citation52 but may not be tolerated by some.Citation45 Success with monovision is dependent on suppression of interocular blur.Citation53 Incomplete suppression may be a safety concern, as monocular blur increases the risk of falls.Citation54,Citation55 Furthermore, for most patients, binocular summation is limited to a contralateral difference of 1.5 D.Citation56 Higher adds may result in binocular inhibition. Therefore, successful implementation of monovision appears to benefit from residual accommodation, and thus may be insufficient in advanced and pseudophakic presbyopia.
Monovision is frequently associated with a reduction of peak acuity, loss of contrast sensitivity, and compromise in stereo acuity.Citation45,Citation57 It also negatively affects quality of vision at all ranges and depth perception.Citation58 As a consequence, it may not be suitable for patients in whom binocular vision and depth perception are particularly critical to their career or lifestyle. There is evidence that monovision may affect the ability to properly perceive motion, especially at far distance.Citation59 Additionally, monovision has been found to impair the ability of elderly patients to effectively judge raised surfaces, thereby contributing to falls.Citation54 Indeed, epidemiological studies have shown an association between decreased monocular visual acuity and stereoacuity and an increased risk of falls and hip fractures in the elderly.Citation23,Citation60
Varying the Refractive Power Across a Range of Distance
Varying the refractive state across a range of distances refers to the creation of simultaneous focus through far, intermediate, and near (). With this mechanism, objects at all distances appear in simultaneous focus, and thus continuity across the field of view and between eyes is preserved.Citation61 This is commonly referred to as pseudoaccommodation. Pseudoaccommodation can have different patterns as characterized by its defocus curve, and it can be achieved by different techniques and at different locations.Citation61 Pseudoaccommodation is distinct from pseudophakic accommodation, with the latter referring to the dynamic change in refractive state due to movement of the IOL/bag complex.Citation62 As noted above, it can be combined with other mechanisms, such as monovision.
Figure 4 Varying the refractive power across a range of distances (pseudoaccomodation) achieves simultaneous focus from far (person) to near (smartphone). In this illustration, an iris pinhole optic provides pseudoaccomodative ability.
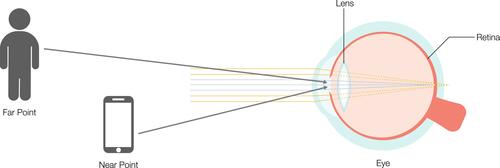
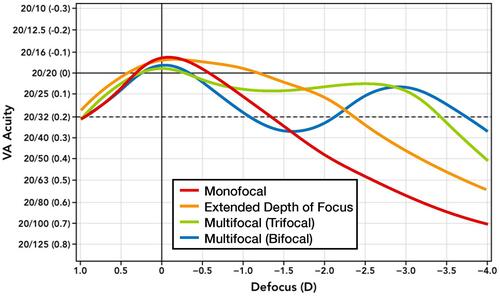
The defocus curve pattern of pseudoaccommodation can be broadly defined by the presence or absence of discrete ranges of sharper focus. Multifocal (bifocal and/or trifocal) technologies create two or more specific ranges of best focus while extended depth of focus technologies are characterized by a single broader range with no inflections in the defocus curve (). Clinically, multifocal defocus curves manifest as objects coming in, out, and back in focus when brought from far to near, while extended depth of focus curves manifests as objects remaining in focus when moving throughout the pseudoaccommodative range.
Figure 5 Representative defocus curves associated with various methods for varying the refractive power across a range of distances.
Interventions
Multiple methods can be used to achieve pseudoaccommodation. They can be categorized by the optical principle leveraged to increase the depth of field: small aperture, refractive, and diffractive optics ().
Figure 6 Varying refractive power across a range of distances may be accomplished by one of three mechanisms. Small Aperture/Pinhole Optics (A) function to block peripheral unfocused light rays, while focused light rays reach the retina. Refractive Optics (B) utilize multiple focusing zones. Diffractive Optics (C) leverage interference patterns to create zones/ranges of focus from far to near.
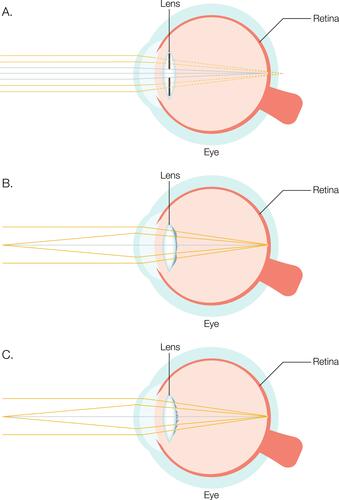
The small aperture, or pinhole effect, extends the depth of focus by blocking unfocused, peripheral light rays and permitting only central light rays to reach the retina.Citation48,Citation63 Various corneal inlaysCitation64 and IOLsCitation65 have been designed utilizing small aperture optics, and several studies are evaluating pharmaceutical eyedrops, such as pilocarpine HCL 1.25% (AGN-190584; Allergan, an AbbVie company; Chicago), that induce a similar effect.Citation66–Citation68 The latter uses the iris to create the pinhole effect, which has the advantage of modulating the existing aperture as opposed to adding a second aperture.
Refractive optics utilize various zones to focus incoming light rays from different distances to create a broader range of focus on the retina. Patterns of refractive contact lens optics include concentric and aspheric designs.Citation69 In presby LASIK, a customized ablation pattern creates a multifocal cornea,Citation70 whereas with refractive corneal inlays, the addition of the implant achieves a similar effect. With refractive multifocal IOLs, the zones of different power can be in concentric, aspheric, segmental, and combined patterns.Citation69
Diffractive optics create a phase shift of the incoming wavefront to create an expanded range of focus so that objects at different distances appear in focus. At current, available diffractive optics employ microscopic steps on the lens surface to create the phase shift necessary to achieve the desired diffractive pattern.Citation71 Varying the height, spacing, and profile of the steps, multifocal, trifocal, and extended depth of focus patterns of increasing through focus have been created.
Finally, laser refractive indexing can theoretically modify the optics of the cornea or an existing implant both through refractive and diffractive means to create multifocality by selectively modifying the refractive index of a tissue or material.Citation72
Advantages and Disadvantages
The specific effects of pseudoaccommodation depend on the method used to expand the visual range. When appropriately applied, small aperture optics can improve visual acuity at near and intermediate distances without negatively impacting far vision, reducing binocular contrast sensitivity, or increasing dysphotopsias.Citation64 However, when the aperture is too small, or when a second aperture is introduced, and possibly misaligned, visual quality can be degraded and peripheral vision can be compromised.Citation63
Application of pseudoaccommodation via refractive and diffractive multifocal optics is successful in many patients, providing functional vision at far, intermediate, and near.Citation73 The two primary disadvantages of pseudoaccommodative optics are potential compromise in visual quality and incidence of bothersome low light dysphotopsias. These potential side effects are inherent to this method of expanding through focus. Therefore, attention to reduction of monochromatic and chromatic aberrations, as well as lens profile and chromophore considerations, is essential to have a successful product.
Conclusion
Understanding presbyopia treatments according to their mechanism of action confers several benefits. From a broad perspective, such a classification system permits a fuller understanding of how closely the given intervention or treatment replicates the physiologic processes that provide the human eye the ability to see in clear focus at any distance with low or no latency. For the clinician, an understanding of mechanisms facilitates clinical decision-making. When offering a treatment option to the patient, the clinician can use prior experiences as a guide. For example, patients who exhibit a suboptimal presbyopia correction with multifocal contact lenses may have difficulties with multifocal IOLs, as the latter utilizes the same mechanism. Instead, the clinician can consider an alternative option that leverages one or more of the other mechanisms noted above.
In some cases, functional through focus can be achieved with a combination of mechanisms. One example may be using an extended depth of focus lens in each eye set at different powers to achieve a mini-monovision arrangement. In this hypothetical example, the overall correction leverages two mechanisms: varying refractive power over a range of distances and between eyes. Similarly, corneal inlays and presby-LASIK can vary the refractive power across a range of distances, and when performed in only one eye, also vary the refractive power between eyes. Thus, the categories described herein can be used in combination in certain clinical settings as building blocks for achieving functional through focus in the correction of presbyopia.
Historically, the treatment of presbyopia has been combined with refractive correction. However, doing so requires greater precision than addressing either problem on its own. Decoupling presbyopia treatment from refractive correction can lower the barrier to restoring functional through focus. This consideration will become even more relevant as newer treatment options become available.
An important limitation to this classification system should be acknowledged. Specifically, at present, there are only limited ways to measure the specific pathologic features contributing to loss of accommodative ability in a given patient. Moreover, the understanding of the exact mechanisms of accommodation is unsettled. Although widely considered the most accurate description of the physiology associated with accommodation, the Helmholtz theoryCitation16 is disputed by other authors.Citation74 Taken together, these facts underscore that any classification system is inherently limited by the extent of the current knowledge base. However, they also suggest an opportunity: as eye models evolve, and as new means of measuring the various mechanisms associated with loss of accommodation become available, the existing framework presented in this article can be updated accordingly.
Fundamentally, we propose this new classification schema because presbyopia treatment should be thought of in terms of medical need rather than as a lifestyle decision. The increasing prevalence of presbyopiaCitation2 stands to account for significant financial burdenCitation8 while negatively impacting patients’ quality of life and daily living.Citation10,Citation11 As well, loss of functional through focus is a safety concern.Citation12 However, what may be under appreciated is that some treatments also introduce safety concerns,Citation38 with substantial implications for direct medical costs.Citation23 Thus, a more meaningful comparison of treatment options based on an understanding of the optical principles leveraged by a given intervention would bring the clinician closer to understanding the true goal of correcting presbyopia: restoring or mimicking the human eye’s natural ability to achieve functional through-focus with imperceptible latency.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Medical Writing, Editorial, and Other Assistance
Editorial assistance in the preparation of this article was provided by Bryan Bechtel of Bechtel Editorial Services, LLC. Support for this assistance was funded by Allergan, an AbbVie Company.
Consent for Publication
All tables and figures used in this publication are the work of the authors and are original.
Author Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Dr. Chang declares that he is a consultant to and has received research support from Allergan/Abbie and Johnson & Johnson Vision, and that he has received research support from AcuFocus, Inc, and personal fees from Carl Zeiss Meditec, outside the submitted work. Dr. Barnett declares that she is a consultant to Allergan/AbbVie and Visus Therapeutics. Dr. Hom declares that he has received research support from the following: AbbVie/Allergan, Novartis, Kala, Tarsus, Hovione Scientia, Silk-tech, Sydnexis, Eyenovia, Surface, Nevakar, AstaReal, and Vyluma; and that he is a consultant to AbbVie/Allergan, Bausch, Novartis, Sun, Kala, Tarsus, laboratoires Thea, Eyevance, Visus, Aperta, and Azura. Dr. Waring declares that he is a consultant to Johnson & Johnson Vision, Allergan/AbbVie, Perfect Lens, and ACE Vision Group. The authors report no other conflicts of interest in this work.
Additional information
Funding
References
- Waring GO, Rocha KM. Characterization of the dysfunctional lens syndrome and a review of the literature. Curr Ophthalmol Rep. 2018;6(4):249–255. doi:10.1007/s40135-018-0190-3
- Fricke TR, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modelling. Ophthalmology. 2018;125(10):1492–1499. doi:10.1016/j.ophtha.2018.04.013
- Pointer JS. The presbyopic add. II. Age-related trend and a gender difference. Ophthalmic Physiol Opt. 1995;15(4):241–248. doi:10.1046/j.1475-1313.1995.9400022r.x
- Holden BA, Fricke TR, Ho SM, et al. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol. 2008;126(12):1731–1739. doi:10.1001/archopht.126.12.1731
- Burke AG, Patel I, Munoz B, et al. Population-based study of presbyopia in rural Tanzania. Ophthalmology. 2006;113(5):723–727. doi:10.1016/j.ophtha.2006.01.030
- Pointer JS. The presbyopic add. III. Influence of the distance refractive type. Ophthalmic Physiol Opt. 1995;15(4):249–253. doi:10.1046/j.1475-1313.1995.9400023s.x
- Pointer JS. Gender-related optical aspects of the onset of presbyopia. Ophthalmic Physiol Opt. 2002;22(2):126–129. doi:10.1046/j.1475-1313.2002.00012.x
- Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology. 2015;122(8):1706–1710. doi:10.1016/j.ophtha.2015.04.014
- Charman WN. Developments in the correction of presbyopia I: spectacle and contact lenses. Ophthalmic Physiol Opt. 2014;34(1):8–29. doi:10.1111/opo.12091
- Goertz AD, Stewart WC, Burns WR, Stewart JA, Nelson LA. Review of the impact of presbyopia on quality of life in the developing and developed world. Acta Ophthalmol. 2014;92(6):497–500. doi:10.1111/aos.12308
- Patel I, Munoz B, Burke AG, et al. Impact of presbyopia on quality of life in a rural African setting. Ophthalmology. 2006;113(5):728–734. doi:10.1016/j.ophtha.2006.01.028
- Wolffsohn JS, Leteneux-Pantais C, Chiva-Razavi S, et al. Social media listening to understand the lived experience of presbyopia: systematic search and content analysis study. J Med Internet Res. 2020;22(9):e18306. doi:10.2196/18306
- American Optometric Association. Care of the Patient with Presbyopia. St. Louis (MO): American Optometric Association; 2010.
- Atchison DA, Charman WN. Thomas Young’s contribution to visual optics: the Bakerian Lecture “on the mechanism of the eye. J Vis. 2010;10(12):16. doi:10.1167/10.12.16
- Ovenseri-Ogbomo GO, Oduntan OA. Mechanism of accommodation: a review of theoretical propositions. Afr Vision Eye Health. 2015;74(1):6. doi:10.4102/aveh.v74i1.28
- Southall JPC, ed. Helmholtz’s Treatise on Physiological Optics. Translated from the 3rd German Ed. New York: Dover Publications; 1962.
- Glasser A, Kaufman PL. The mechanism of accommodation in primates. Ophthalmology. 1999;106(5):863–872. doi:10.1016/s0161-6420(99)00502-3
- Goldberg DB. Computer-animated model of accommodation and presbyopia. J Cataract Refract Surg. 2015;41(2):437–445. doi:10.1016/j.jcrs.2014.07.028
- Harvard Health Publishing. Medical dictionary of health terms; 2021. Available from: https://www.health.harvard.edu/medical-dictionary-of-health-terms/j-through-p#P-terms. Accessed March 10, 2021.
- Croft MA, Glasser A, Kaufman PL. Accommodation and presbyopia. Int Ophthalmol Clin. 2001;41(2):33–46. doi:10.1097/00004397-200104000-00005
- Lichtinger A, Rootman DS. Intraocular lenses for presbyopia correction: past, present, and future. Curr Opin Ophthalmol. 2012;23(1):40–46. doi:10.1097/ICU.0b013e32834cd5be
- Torricelli AA, Junior JB, Santhiago MR, Bechara SJ. Surgical management of presbyopia. Clin Ophthalmol. 2012;6:1459–1466. doi:10.2147/opth.s35533
- Chang DH. Multifocal spectacle and monovision treatment of presbyopia and falls in the elderly. J Refract Surg. 2021;37(S1):S12–S16. doi:10.3928/1081597X-20210408-02
- Korenfeld MS, Robertson SM, Stein JM, et al. Topical lipoic acid choline ester eye drop for improvement of near visual acuity in subjects with presbyopia: a safety and preliminary efficacy trial. Eye (Lond). 2021. doi:10.1038/s41433-020-01391-z
- Gualdi L, Gualdi F, Rusciano D, et al. Ciliary muscle electrostimulation to restore accommodation in patients with early presbyopia: preliminary results. J Refract Surg. 2017;33(9):578–583. doi:10.3928/1081597x-20170621-05
- Lubatschowski H, Schumacher S, Fromm M, et al. Femtosecond lentotomy: generating gliding planes inside the crystalline lens to regain accommodation ability. J Biophoton. 2010;3(5–6):265–268. doi:10.1002/jbio.201000013
- Schumacher S, Oberheide U. Femtosecond lentotomy: a prospect for a treatment to regain the accommodation ability. In: Nolte S, Schrempel F, Dausinger F, editors. Ultrashort Pulse Laser Technology. Springer Series in Optical Sciences. Vol. 195. Cham: Springer; 2016: 285–309. doi:10.1007/978-3-319-17659-8_13
- Hipsley A, Hall B, Rocha KM. Scleral surgery for the treatment of presbyopia: where are we today? Eye Vis (Lond). 2018;5:4. doi:10.1186/s40662-018-0098-x
- Alió JL, Alió Del Barrio JL, Vega-Estrada A. Accommodative intraocular lenses: where are we and where we are going. Eye Vis (Lond). 2017;4:16. doi:10.1186/s40662-017-0077-7
- Liang YL, Jia SB. Clinical application of accommodating intraocular lens. Int J Ophthalmol. 2018;11(6):1028–1037. doi:10.18240/ijo.2018.06.22
- Ossma IL, Galvis A, Vargas LG, Trager MJ, Vagefi MR, McLeod SD. Synchrony dual-optic accommodating intraocular lens. Part 2: pilot clinical evaluation. J Cataract Refract Surg. 2007;33(1):47–52. doi:10.1016/j.jcrs.2006.08.049
- Alió JL, Ben-nun J, Rodríguez-Prats JL, Plaza AB. Visual and accommodative outcomes 1 year after implantation of an accommodating intraocular lens based on a new concept. J Cataract Refract Surg. 2009;35(10):1671–1678. doi:10.1016/j.jcrs.2009.04.043
- Studeny P, Krizova D, Urminsky J. Clinical experience with the WIOL-CF accommodative bioanalogic intraocular lens: Czech National Observational Registry. Eur J Ophthalmol. 2016;26(3):230–235. doi:10.5301/ejo.5000653
- Pérez-Merino P, Birkenfeld J, Dorronsoro C, et al. Aberrometry in patients implanted with accommodative intraocular lenses. Am J Ophthalmol. 2014;157(5):1077–1089. doi:10.1016/j.ajo.2014.02.013
- Letocha CE. The invention and early manufacture of bifocals. Surv Ophthalmol. 1990;35(3):226–235. doi:10.1016/0039-6257(90)90092-a
- Alió JL, Piñero DP, Plaza-Puche AB, Chan MJ. Visual outcomes and optical performance of a monofocal intraocular lens and a new-generation multifocal intraocular lens. J Cataract Refract Surg. 2011;37(2):241–250. doi:10.1016/j.jcrs.2010.08.043
- Sheedy JE, Campbell C, King-Smith E, Hayes JR. Progressive powered lenses: the Minkwitz theorem. Optom Vis Sci. 2005;82(10):916–922. doi:10.1097/01.opx.0000181266.60785.c9
- Lord SR, Dayhew J, Howland A, Howland A. Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people. J Am Geriatr Soc. 2002;50(11):1760–1766. doi:10.1046/j.1532-5415.2002.50502.x
- Charman WN, Saunders B. Theoretical and practical factors influencing the optical performance of contact lenses for the presbyope. J Br Contact Lens Ass. 1990;13:67–75. doi:10.1016/0141-7037(90)80012-Q
- Woods RL. The aging eye and contact lenses – a review of ocular characteristics. J Br Contact Lens Ass. 1991;14:115–127. doi:10.1016/0141-7037(91)80004-6
- Chu BS, Wood JM, Collins MJ. The effect of presbyopic vision corrections on nighttime driving performance. Invest Ophthalmol Vis Sci. 2010;51(9):4861–4866. doi:10.1167/iovs.10-5154
- Cochener B, Lafuma A, Khoshnood B, Courouve L, Berdeaux G. Comparison of outcomes with multifocal intraocular lenses: a meta-analysis. Clin Ophthalmol. 2011;5:45–56. doi:10.2147/opth.s14325
- Maxwell WA, Lane SS, Zhou F. Performance of presbyopia-correcting intraocular lenses in distance optical bench tests. J Cataract Refract Surg. 2009;35(1):166–171. doi:10.1016/j.jcrs.2008.10.026
- Qian N. Binocular disparity and the perception of depth. Neuron. 1997;18(3):359–368. doi:10.1016/s0896-6273(00)81238-6
- Evans BJ. Monovision: a review. Ophthalmic Physiol Opt. 2007;27(5):417–439. doi:10.1111/j.1475-1313.2007.00488.x
- Blake R, Logothetis N. Visual competition. Nat Rev Neurosci. 2002;3(1):13–21. doi:10.1038/nrn701
- Polonsky A, Blake R, Braun J, Heeger DJ. Neuronal activity in human primary visual cortex correlates with perception during binocular rivalry. Nat Neurosci. 2000;3(11):1153–1159. doi:10.1038/80676
- Charman WN. Developments in the correction of presbyopia II: surgical approaches. Ophthalmic Physiol Opt. 2014;34(4):397–426. doi:10.1111/opo.12129
- Finkelman YM, Ng JQ, Barrett GD. Patient satisfaction and visual function after pseudophakic monovision. J Cataract Refract Surg. 2009;35(6):998–1002. doi:10.1016/j.jcrs.2009.01.035
- Greenbaum S. Monovision pseudophakia. J Cataract Refract Surg. 2002;28(8):1439–1443. doi:10.1016/s0886-3350(02)01218-x
- Ito M, Shimizu K. Reading ability with pseudophakic monovision and with refractive multifocal intraocular lenses: comparative study. J Cataract Refract Surg. 2009;35(9):1501–1504. doi:10.1016/j.jcrs.2009.03.051
- Marques FF, Sato RM, Chiacchio BB, Marques DM, Barreiro J, Caetano RL. Evaluation of visual performance and patient satisfaction with pseudophakic monovision technique. Arq Bras Oftalmol. 2009;72(2):164–168. doi:10.1590/s0004-27492009000200006
- Schor C, Landsman L, Erickson P. Ocular dominance and the interocular suppression of blur in monovision. Am J Optom Physiol Opt. 1987;64(10):723–730. doi:10.1097/00006324-198710000-00002
- Vale A, Buckley JG, Elliott DB. Gait alterations negotiating a raised surface induced by monocular blur. Optom Vis Sci. 2008;85(12):1128–1134. doi:10.1097/OPX.0b013e31818e8d2a
- Vale A, Scally A, Buckley JG, Elliott DB. The effects of monocular refractive blur on gait parameters when negotiating a raised surface. Ophthalmic Physiol Opt. 2008;28(2):135–142. doi:10.1111/j.1475-1313.2008.00543.x
- Hayashi K, Yoshida M, Manabe S, Hayashi H. Optimal amount of anisometropia for pseudophakic monovision. J Refract Surg. 2011;27(5):332–338. doi:10.3928/1081597x-20100817-01
- Durrie DS. The effect of different monovision contact lens powers on the visual function of emmetropic presbyopic patients (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2006;104:366–401.
- Kollbaum PS, Bradley A. Correction of presbyopia: old problems with old (and new) solutions. Clin Exp Optom. 2020;103(1):21–30. doi:10.1111/cxo.12987
- Burge J, Rodriguez-Lopez V, Dorronsoro C. Monovision and the misperception of motion. Curr Biol. 2019;29(15):2586–2592.e4. doi:10.1016/j.cub.2019.06.070
- Felson DT, Anderson JJ, Hannan MT, Milton RC, Wilson PW, Kiel DP. Impaired vision and hip fracture. The Framingham Study. J Am Geriatr Soc. 1989;37(6):495–500. doi:10.1111/j.1532-5415.1989.tb05678.x
- Nishi T, Taketani F, Ueda T, Ogata N. Comparisons of amplitude of pseudoaccommodation with aspheric yellow, spheric yellow, and spheric clear monofocal intraocular lenses. Clin Ophthalmol. 2013;7:2159–2164. doi:10.2147/opth.s52771
- Patel R, Wang L, Koch DD, Yeu E. Pseudoaccommodation. Int Ophthalmol Clin. 2011;51(2):109–118. doi:10.1097/IIO.0b013e31820f2748
- Charman WN. Pinholes and presbyopia: solution or sideshow? Ophthalmic Physiol Opt. 2019;39(1):1–10. doi:10.1111/opo.12594
- Seyeddain O, Hohensinn M, Riha W, et al. Small-aperture corneal inlay for the correction of presbyopia: 3-year follow-up. J Cataract Refract Surg. 2012;38(1):35–45. doi:10.1016/j.jcrs.2011.07.027
- Dick HB, Piovella M, Vukich J, Vilupuru S, Lin L. Prospective multicenter trial of a small-aperture intraocular lens in cataract surgery. J Cataract Refract Surg. 2017;43(7):956–968. doi:10.1016/j.jcrs.2017.04.038
- Vargas V, Vejarano F, Alió JL. Near vision improvement with the use of a new topical compound for presbyopia correction: a prospective, consecutive interventional non-comparative clinical study. Ophthalmol Ther. 2019;8(1):31–39. doi:10.1007/s40123-018-0154-6
- Benozzi J, Benozzi G, Orman B. Presbyopia: a new potential pharmacological treatment. Med Hypothesis Discov Innov Ophthalmol. 2012;1(1):3–5.
- Abdelkader A. Improved presbyopic vision with miotics. Eye Contact Lens. 2015;41(5):323–327. doi:10.1097/icl.0000000000000137
- Terwee T, Weeber H, van der Mooren M, Piers P. Visualization of the retinal image in an eye model with spherical and aspheric, diffractive, and refractive multifocal intraocular lenses. J Refract Surg. 2008;24(3):223–232. doi:10.3928/1081597x-20080301-03
- Vargas-Fragoso V, Alió JL. Corneal compensation of presbyopia: presbyLASIK: an updated review. Eye Vis (Lond). 2017;4:11. doi:10.1186/s40662-017-0075-9
- Davison JA, Simpson MJ. History and development of the apodized diffractive intraocular lens. J Cataract Refract Surg. 2006;32(5):849–858. doi:10.1016/j.jcrs.2006.02.006
- Ding L, Knox WH, Bühren J, Nagy LJ, Huxlin KR. Intratissue refractive index shaping (IRIS) of the cornea and lens using a low-pulse-energy femtosecond laser oscillator. Invest Ophthalmol Vis Sci. 2008;49(12):5332–5339. doi:10.1167/iovs.08-1921
- Xu X, Zhu MM, Zou HD. Refractive versus diffractive multifocal intraocular lenses in cataract surgery: a meta-analysis of randomized controlled trials. J Refract Surg. 2014;30(9):634–644. doi:10.3928/1081597x-20140814-04
- Charman WN. The eye in focus: accommodation and presbyopia. Clin Exp Optomet. 2008;91:207–225. doi:10.1111/j.1444-0938.2008.00256.x
