Abstract
Purpose
To evaluate the success rate of a modified bleb needling technique in eyes with previous glaucoma surgery that had elevated intraocular pressure.
Methods
A retrospective study of 24 eyes of 24 patients that underwent repeated bleb needling performed for failing and failed blebs on slit lamp with 5-fluorouracil (5-FU) injections on demand. This was performed after gonioscopic examination to define levels of filtration block.
Results
There was significant reduction of mean IOP from 36.91 mmHg to 14.73 mmHg at the final follow-up (P < 0.001). The overall success rate was 92%.
Conclusion
Repeated needling with adjunctive 5-FU proved a highly effective, safe alternative to revive filtration surgery rather than another medication or surgery.
Keywords:
Introduction
Trabeculectomy is still the gold standard surgical procedure for treatment of glaucoma. It entails opening a fistula between the anterior chamber and the subconjunctival space, generating a reservoir for aqueous humor. It has a success rate of 67%–94%.Citation1 Early and late failure of filtering bleb due to fibrotic proliferation is especially reported in uveitis, aphakia, neovascular, and recurrent glaucomas.Citation2 A second trabeculectomy, especially in the aforementioned cases, may have a similar or lower success rate to the first procedure with the sacrifice of more virgin conjunctiva.Citation1 Drainage device implants including new generation ones, such as the Ex-PRESS Mini Glaucoma Shunt (Alcon, Houston, TX),Citation3 have a final (36-month) probability success rate of 50.9% and 60.6% in eyes with previous trabeculectomy and previous cataract surgery, respectively.Citation4 It is, furthermore, a more expensive alternative.Citation3,Citation4
Reinstitution of topical treatment may not be enough to control the intraocular pressure (IOP) or may be associated with poor compliance and more conjunctival damage.Citation5
Cyclodestructive procedures, including cyclophotocoagulation, have an inherent unpredictability and present a risk of hypotony and visual loss.Citation6 Needle revision with 5-fluorouracil (5-FU) was first reported by Ewing and Stamper.Citation7 Glaucoma surgery fails because of aqueous blocks at the levels of the internal ostium, intrascleral, or subconjunctival space.Citation1 Intrascleral and episcleral fibrosis are responsible for blockages in the last two levels.Citation1 Our study utilized a proper algorithm to exclude internal ostium blocks first by gonioscopy. We used gonioscopy to define the level of obstruction of aqueous outflow, then assessed needling as a way to eradicate all fibrous tissue present in the episcleral and intrascleral levels. Most studies in the literature have focused on needle revisions performed in the early postoperative periods.Citation8,Citation9
We are aiming to assess the efficacy of needling for both early and late bleb failure months and years after the original surgery.
Patients and methods
The study was retrospective and included 24 eyes of 24 patients operated upon by the same surgeon from December 2009 to December 2011.
Inclusion criteria
Impending failure due to flattening and increased vascularization.
Failed previous glaucoma surgery.
Patent internal ostium of filtration surgery site.
Failure to achieve target IOP despite surgery, and/or medical treatment.
In all cases, an informed consent form was provided prior to surgery that explained the use of needling to improve bleb function.
Exclusion criteria
Eyes with internal iris block.
Leaky bleb.
Corneal epithelial complications.
Fornix-based conjunctival flap in early postoperative period.
Eyes with more than one filtering surgery.
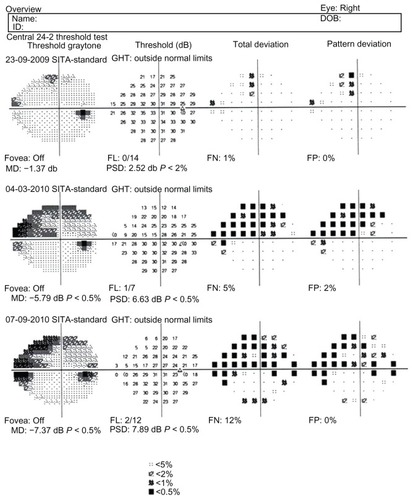
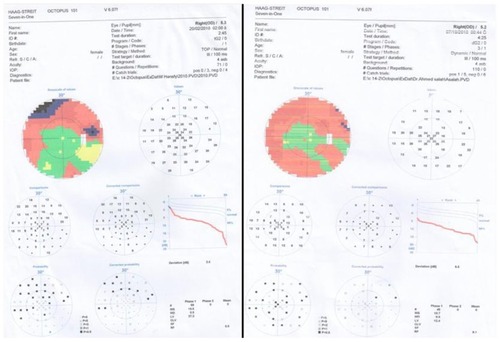
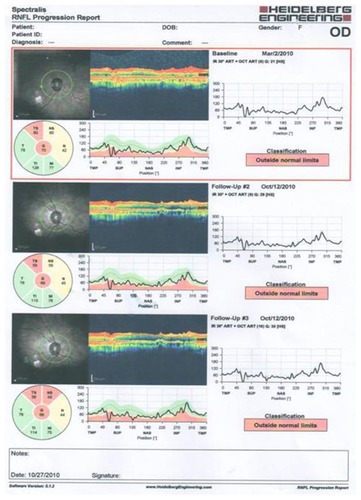
The descriptive parameters were age, sex, type of glaucoma, time elapsed since surgery, bleb morphology, IOP, and number of antiglaucoma medications used by the patient. Examination of cup-to-disc (CD) ratio was confirmed by an optical coherence tomography (OCT) assessment of the retinal nerve fiber layer (RNFL) thickness. Field examination with Humphrey field analyzer (Carl Zeiss) or Octopus field analyzer (Haag Streit International, Koeniz, Switzerland) and central corneal thickness (CCT) assessment were performed for all patients.
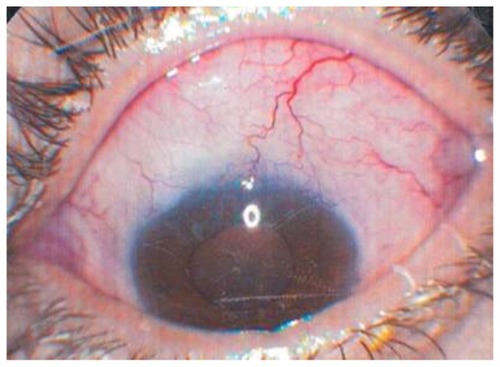
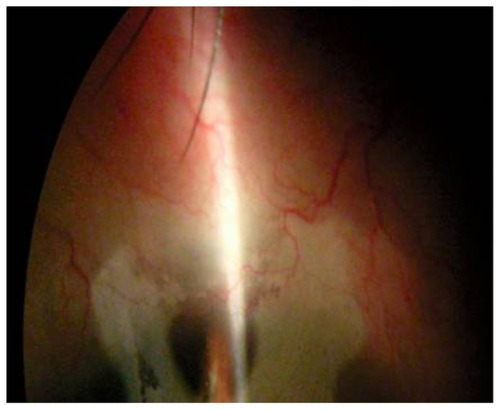
IOP was measured by Goldmann applanation tonometry on 2 different preoperative days, and the mean value was calculated as a baseline IOP. Gonioscopic examination was done by Goldmann three-mirror contact lens. The gonioscope lens was oriented for a view of ostium of the filtration surgery site. According to internal examination, eyes were classified to episcleral fibrosis (flap elevated from its bed) and intrascleral fibrosis (flap attached to its bed) after exclusion of the eyes with internal block. Bleb was considered failing if it was vascularized with gradually raising IOP (). Failed bleb was considered if it was completely flattened with elevated IOP. The needling procedure was performed in-office using a slit lamp for proper visualization of the layers. Topical anesthesia was 0.5% proparacaine drops and microsponge soaked in 2% lidocaine applied to the conjunctival surface. Eyelids and surrounding skin were prepared with a 10% povidone–iodine solution. Lidocaine 2% 0.1 mL was drawn into a 25-gauge needle insulin syringe. 5-FU (5 mg/0.1 mL) standard dose was drawn into another 25-gauge needle insulin syringe.
The needle of the lidocaine syringe was introduced about 10 mm away from the bleb and away from conjunctival blood vessels. The needle was inserted slowly and gently to reach the bleb. In case of episcleral fibrosis, the needle was moved in a side-to-side motion, breaking episcleral adhesions around the bleb and over the scleral flap. In cases of intrascleral fibrosis, the needle was introduced beneath the flap by moving the needle side-to-side, breaking adhesions and cutting suture, if present. If the patient had some pain, the plunger was pushed slowly to inject subconjunctival lidocaine. If IOP was still high, the procedure was repeated to break more adhesions. The needle of the syringe containing 5-FU was introduced subconjunctivally away from the needling site. Postneedling treatment consisted of a combination of tobramycin and dexamethasone 1% (TobraDex; Alcon) six times a day for 3 days and ciprofloxacin 0.3% every 2 hours on the first day and 6 times a day for 2 days thereafter. The patient was examined 2–3 days later.
Subconjunctival injection of 5 mg in 0.1 mL 5-FU near the bleb was repeated every visit for a minimum of five injections. Repetition of 5-FU injections was stopped when large blood vessels above and near the bleb disappeared (). It was also stopped if any epithelial defect or complication appeared. IOP was measured every visit. If IOP was elevated beyond the target IOP, needling was repeated. We performed needling when necessary, to a maximum of three times. Every needling procedure was associated with 5-FU injection. If IOP was still elevated after the third needling, medical treatment was reinstituted. Postneedling visits were scheduled every other day or twice a week, depending on IOP elevation. The minimum interval of 5-FU injections with or without needling repetition was 48 hours.
Target IOP was identified according to glaucoma severity. Based on the Early Manifest Glaucoma Trial (EMGT),Citation10,Citation11 glaucoma was considered moderate when eyes had a vertical CD ratio of 0.7 to 0.85, or when they had one hemifield defect with mean deviation (MD) from −6 to −12, not within 10° of fixation, or both. In these eyes, the target IOP was set at <17 mmHg with a reduction of at least 30% from the baseline IOP. Eyes were classified as having advanced disease, based on the Advanced Glaucoma Intervention Study (AGIS),Citation11,Citation12 when the vertical CD ratio was 0.9 or greater; the visual field had both hemifields affected; there was a defect encroaching on the central 10°; MD was worse than −12; or any of these features occurred together. In these eyes, the target IOP was set at <14 mmHg with a reduction of at least 30% from the baseline IOP. The target IOP was corrected accordingly for extreme CCT changes from the assumed 520 μm level.Citation13
A complete success was defined by achievement of the target IOP without medications. A qualified success was defined by achievement of the target IOP with the aid of hypotensive medication(s). Failure was defined by IOP greater than the target IOP, despite the maximum medications (topical medications three entititeis of antiglaucoma in two bottles) used and three needlings having been done.
Statistical methods
Data were presented as mean and standard deviation (SD) values. Paired sample t-test was used to compare two paired groups and independent sample t-test was used to compare two independent groups. Spearman’s correlation coefficient was used to determine the significant correlations between the studied parameters.
The significance level was set at P ≤ 0.05. Statistical analysis was performed with statistical package for social science (SPSS) version 16.0 for Windows (IBM Corporation, Armonk, NY).
Results
Our study included 24 eyes of 24 patients. Age of patients ranged from 29 to 75 years (mean 48.42 ± 14.36 years) and included 12 males and 12 females. All patients were from Egypt with the exception of dark race that has a high incidence of filtration surgery failure. Eyes with advanced disease number was 18/24 (66.7%) (–) and eyes with moderate disease number was 6/24 (33.3%). None of the eyes had early disease.
Figure 4 Preoperative serial optical coherence tomography examination of eye 1 with advanced disease.
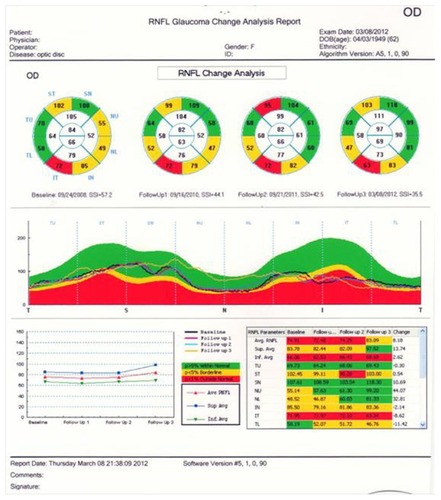
Figure 6 Two preoperative serial optical coherence tomography examinations for retinal nerve fiber layer progression of eye 4.
The preneedling IOP ranged from 26 to 60 mmHg (mean 36.91 ± 11.14 mmHg). Primary open-angle glaucoma was present in eight eyes (33.3%), pseudophakic glaucoma in eight eyes (33.3%), uveitic glaucoma in four eyes (16.7%), silicone-induced glaucoma in two eyes (8.3%), and chronic angle-closure glaucoma in two eyes (8.3%).
Eighteen eyes (75%) were described as having failing blebs and six eyes (25%) had failed blebs. All eyes had subscleral trabeculectomy. According to gonioscope examination, 18 eyes (75%) had episcleral fibrosis and six eyes (25%) had intrascleral fibrosis.
We performed needling procedures at a mean of 1.83 needlings per eye (SD 0.72). Eight eyes (33%) were needled once, 12 eyes (50%) twice, and four eyes (17%) three times.
describes statistical details of needling and 5-FU injections.
Table 1 Descriptive statistics of needling and 5-fluorouracil (5-FU) injection
The average follow-up after the first needling was 18.2 months (SD 6.0, range 2–50 months). The mean postneedling IOP was 14.73 ± 5.12 SD, which was significantly different from the preoperative IOP. describes preneedling and postneedling IOP and medications.
Table 2 Comparison between preneedling and postneedling intraocular pressure (IOP) and medications
No significant difference was found between postoperative IOP in both the failing and failed groups (). There was also no significant difference between postoperative IOP reduction and type of block in either the episcleral or intrascleral groups ().
Table 3 Comparison between postoperative IOP of failing versus failed groups, and episcleral fibrosis versus intrascleral fibrosis groups
There was no correlation between number of needling procedures performed and postoperative IOP reduction, and no correlation between the number of 5-FU injections and postoperative IOP reduction ().
Table 4 Correlation between postneedling IOP and number of needlings and injections
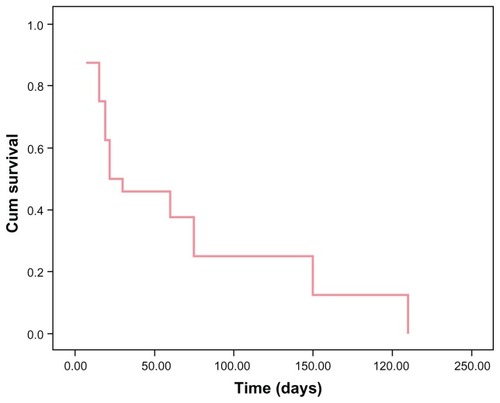
In this study, the overall success rate of needling procedures was 92%. The median survival time for patients was 22 days ().
Complete success was achieved in 16 eyes (66.7%); qualified success was achieved in six eyes (25%). Needling failure occurred in two eyes (8.3%). One eye (4.2%) developed corneal decompensation and two eyes (8.4%) had a conjunctival gaped wound that necessitated suturing of the conjunctiva by 7.0 Vicryl sutures (Alcon) for fear of infection. Two eyes (8.3%) developed punctuate epithelial erosion that necessitated discontinuation of 5-FU injections and prescription of preservative-free artificial tears (Refresh Plus® eye drops; Allergan Inc, Irvine, CA) every 2 hours until resolution within 1 week. None of the eyes had persistent epithelial defect.
Two eyes (8.4%) had IOP less than 10 mmHg. These eyes underwent a dilated fundus examination due to the possibility of choroidal detachment: only one eye (4.2%) had a small peripheral choroidal detachment that resolved spontaneously over 1 week. None of our eyes had postneedling shallow anterior chamber, even those with a gaped conjunctival wound.
Discussion
Failed filtration surgery is a common and challenging problem. Most failures are caused by fibrous tissue proliferation, which is a natural feature of wound healing.Citation1 Needling to break fibrous tissue without the use of antimetabolites has shown a success rate of 7% and a qualified success rate of 57%, which did not show significant difference from medical treatment alone.Citation14 Probability of success of filtering surgery with no intraoperative or postoperative antifibrotic agent was 56%.Citation15 Failing blebs with a fornix-based conjunctival flap in the early postoperative period were excluded from our study to avoid suture dehiscence.
We performed needling using a slit lamp for better visualization of the subconjunctival space, identification of scleral flap, and immediate measure of IOP after needling. This allows further introduction of the needle to subconjunctival space to break adhesions if IOP is still high. Martinez et al also used slit lamp for needling.Citation16 Gonioscopy allowed internal examination of the ostium for classification of outflow obstruction into episcleral (subconjunctival) fibrosis and intrascleral fibrosis, which allows for identification of the level to which the needle must be introduced.
We described a significant reduction of mean IOP from 36.91 mmHg to 14.73 mmHg in 18.2 months’ follow-up. Durak et alCitation17 described a reduction of mean IOP from 27.8 mmHg to 20.5 mmHg.
Our greater reduction of IOP after needling may be related to a greater number of 5-FU injections (4.25/eye) than in Durak et al, who described a mean of 2.4 5-FU injections per eye.Citation17
Martinez et alCitation16 described a reduction of IOP from 26 mmHg to 16.3 mmHg (a 9.5 mmHg reduction). We described a greater reduction of 22 mmHg. Also, we described higher overall (complete and qualified) success (92%) than Martinez et al, who described an overall success rate of 70%.Citation16 The lower success rate of Martinez et alCitation16 may be because of a simpler technique that did not break all fibrous adhesions. Martinez et al described repeated subconjunctival punctures for the filtering bleb, whereas our study described side-to-side movement of the needle to remove fibrous adhesions, according to its level as identified by gonioscopy.Citation16
Our overall higher success rate can be explained by the breaking of the episcleral as well as intrascleral fibrosis. Furthermore, we used the needle to cut the scleral flap suture if the IOP was not lowered with needling. This explanation can be supported by the results of Mastropasqua et al’s postoperative 5-FU use after ocular massage during the first 3 months, in which a cumulative success rate of 100% was reported.Citation15 This may be because of the breaking of intrascleral, early-forming fibrinous proliferations by ocular massage and prevention of reformation by 5-FU injections.
Another studyCitation18 described a 65% overall needling success rate 1 year or more after failed trabeculectomy. This could be explained by the single needling procedure performed.
Our success rate also was higher than that of the needling of failed bleb by Maestrini et al,Citation19 who reported reestablished aqueous flow with raised bleb immediately in 92% of their eyes. However, they described only 76% of their eyes achieving overall IOP less than 16 mmHg, including 58% without medical treatment and 17% with medical treatment. This may be explained by the technique they used: “We never introduced the needle under the scleral flap or into the anterior chamber.”Citation18 This means an inability to break intrascleral adhesions.
Maestrini et al used mitomycin C (MMC) as antiproliferative, hence their caution regarding its toxic effect on corneal endothelium with anterior chamber entry.Citation19 we used 5-FU, even though MMC seems to be more effective for needle revisions in terms of the number of injections.Citation20 We described 5-FU injection away from the needling site and using a different needle from that used for needling. We also injected 5-FU slowly, monitoring both subconjunctival space and anterior chamber on the slit lamp. We found that 5-FU allows for more gradual modulation of the healing response by varying the number of postoperative injections.Citation15
In a study using needling with MMC,Citation16 eleven eyes (8%) developed hypotony and one of them needed surgical treatment with scleral patch graft. None of our eyes had hypotony less than 5 mmHg and none had significant choroidal detachment, indicating a gradual decrease of IOP with repeated 5-FU injections rather than sudden IOP reduction with MMC. The potency of MMC was indicated by Anand and Khan,Citation20 who reported single-needle revision in 47% of a 5-FU group compared to 80% of an MMC group (P = 0.009). Furthermore, our technique allowed us to break intrascleral fibrous adhesions without fear of endothelial toxicity from 5FU. We used a separate syringe for needling and another one to inject 5-FU away from the bleb site to avoid its leakage inside the eye.
Reviving success of 92% of the needling procedure represents retrieval of optic nerve in eyes with failed or failing filtering surgery. Another studyCitation21 reported 80% success of 5-FU injection in encapsulated bleb after drainage device surgery. This may be because they used needling together with 5-FU in only 50% of these eyes. It should be noted, however, that it is difficult to compare studies because of differences in inclusion criteria, success criteria, procedures, techniques, and periods of follow-up.
We have noticed that a needling technique with adjuvant 5-FU injection on demand was equally effective in IOP reduction in both failing bleb and failed bleb, regardless of the time elapsed after trabeculectomy. This is probably because we repeated needling to break already formed fibrous adhesions and repeated 5-FU injections to prevent new fibroblast activity.
Early successful needle revision has been described by other authors.Citation8,Citation9 Late needling with MMC was described by Masterini et al,Citation19 who described needle revision after 6 months to 30 years for failed trabeculectomy. We have described needling with 5-FU in 25% of our eyes from 1 to 10 years after filtering surgery. We also noticed similar IOP reduction in both episcleral and intrascleral levels of fibrous adhesions.
Skuta and ParrishCitation1 have described that bleb failure most often results from f ibroblast proliferation and subconjunctival fibrosis. To the contrary, Jinza et alCitation22 used ultrasound biomicroscopy to study filtering blebs and aqueous drainage routes beneath the scleral flap. They concluded that excessive healing of scleral wounds beneath the scleral flap may be involved in reduced aqueous filtration as well as subconjunctival fibrosis of the filtering bleb. This conclusion supports our modified needling technique to introduce the needle beneath the scleral flap based on gonioscopy result. Jinza et al also stated that an aqueous drainage route beneath the trabeculectomy scleral flap cannot be evaluated by conventional slit-lamp examination.Citation22 Another study, by Kaushik et al,Citation23 classified bleb failure after trabeculectomy into scleral route patent (SRP) and scleral route occluded (SRO), whereas we used gonioscopy for internal examination of the bleb bed to properly locate sites of fibrosis.
The abovementioned study,Citation23 although based on ultrasound biomicroscopy, used sub-Tenon needling in both SRP and SRO eyes. In our study, although based on simpler gonioscopy examination, we introduced the needle beneath the scleral flap in SRO eyes; this explains the failure of all SRO blebs reported by Kaushik et al and our equal outcome in eyes with intrascleral and episcleral fibrosis.
We also found that number of needlings and number of 5-FU injections did not correlate with IOP reduction. This is explained by the fact that we repeated needling as long as fibrous tissue was present and IOP was high. We also repeat 5-FU injections whenever vascularization was detected. These numbers were customized for each eye until target IOP was achieved.
The key study of postoperative use of 5-FU injectionCitation24 described a 21-injection protocol; however, this regimen is onerous for both patient and physician. We described fewer injections because of our modified needling technique and 5-FU injection beside the bleb. The Fluorouracil Filtering Surgery Study GroupCitation24 injected 5-FU 180° away from the bleb, usually in the inferior fornix.
In our study, conjunctival gaping that needed suturing was found in two eyes (8.4%). In a study using MMC with needling, accidental conjunctival perforation occurred in three eyes, but healed spontaneously within a few days,Citation16 and conjunctival hemorrhage was reported in 100% of needling procedures. We observed that subconjunctival blood was one of the features of successful needling. Other criteria of successful needling were sound or sensation of adhesion release and free movement of the needle in the subconjunctival space. These criteria were usually associated with bleb elevation and reduction of IOP after needling.
Punctate epithelial erosion (PEE) was described in two eyes (8.4%); Durak et alCitation17 described PEE in up to 44%. Another studyCitation25 reported 50% transient corneal epithelial defects. Our lower incidence may be related to meticulous injection only in the subconjunctival space.
One of our patient’s eyes (4%) had corneal endothelial decompensation, probably due to endothelial toxicity. Mazey et al described reversible corneal edema due to endothelial damage.Citation26 However, the potential for more serious complications, such as kissing choroidal detachment,Citation27 suprachoroidal hemorrhage,Citation8 malignant glaucoma,Citation19 and enodophthalmitis,Citation8 should not be overlooked.
The present study had some limitations, namely in being a retrospective study, having a relatively small sample, and inclusion of different glaucoma mechanisms and types.
Conclusion
Modified needling technique that addresses all fibrous adhesions and even sutures of the flap together with subconjuctival 5-FU injections near the bleb represent a relatively simple and successful technique. Needling is a safe technique that should be considered at any time after filtering surgery to regain bleb function prior to deciding another surgery and even prior to prescribing further medications. Simple gonioscopy helps establish the proper approach to use needling only in cases of open internal ostium. Gonioscoby also helps to define the level in which needling should be performed according to level of block.
Disclosure
The author reports no conflict of interest in this work.
References
- SkutaGLParrishRK2ndWound healing in glaucoma filtering surgerySurv Opthalmol198732149170
- RudermanJMRevising the failing filtration blebTechniques in Ophthalmology20053133137
- SarkisianSRUse of injector for Ex-PRESS mini glaucoma shuntOphthalmic Surg Lasers Imaging20073843443617955854
- LankaranianDRazeghinejadMRPrasadAIntermediate term results of Ex-Press miniature glaucoma implant under a scleral flap in previously operated eyesClin Experiment Ophthalmol2011395838138221749592
- KassMAGordonMMeltzerDWCompliance with topical timolol treatmentAm J Opthalmol1987103188193
- KosokoOGaasterlandDEPollackIPEngerCLLong-term outcome of initial ciliary ablation with contact diode laser transscleral cyclophotocoagulation for severe glaucoma. The Diode Laser Ciliary Ablation Study GroupOphthalmology19961038129413028764801
- EwingRHStamperRLNeedle revision with and without 5-fluorouracil for the treatment of failed filtering blebsAm J Opthalmol1990110254259
- GreenfieldDSMillerMPSunerIJPalmbergPFNeedle elevation of the scleral flap for failing filtration blebs after trabeculectomy with mitomycin CAm J Opthalmol1996122195204
- RotchfordAPKingJANeedling revision of trabeculectomies bleb morphology and long-term survivalOphthalmology20081151148115318082890
- HeijLALeskeMCBengtssonBHusseinMEarly Manifest Glaucoma Trial GroupReproduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma TrialArch Ophthalmol2002120101286127912365906
- Canadian Ophthalmological Society Glaucoma Clinical Practice Guideline Expert Committee, Canadian Ophthalmological SocietyCanadian Ophthalmological Society evidence-based clinical practice guidelines for the management of glaucoma in the adult eyeCan J Opthalmol200944Suppl 1S793 English and French
- [No authors listed]The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS InvestigatorsAm J Ophthalmol2000130442944011024415
- EhlersNBramsenTSperlingSApplanation tonometry and central corneal thicknessActa Ophthalmol (Copenh)197553134431172910
- CostaVPCorreaMMKara-JoseNNeedling versus medical treatment in encapsulated blebs. A randomized, prospective studyOpthalmology1997104812151220
- MastropasquaLCarpinetoPCiancagliniMZuppardiELobefaloLGallengaPEDelayed post-operative use of 5-fluorouracil as an adjunct in medically uncontrolled open angle glaucomaEye (Lond)19981247017069850268
- Perucho-MartínezSGutiérrez-DíazEMontero-RodríguezMMencía-GutiérrezELago-LlinásMDNeedle revision of late failing filtering blebs after glaucoma surgeryArch Soc Esp Oftalmol200681517522 Spanish17016783
- DurakIOzbekZYamanASoylevMCingilGThe role of needle revision and 5-fluorouracil application over the filtration site in the management of bleb failure after trabeculectomy: a prospective studyDoc Opthalmol20031062189193
- KapasiMSBirtCMThe efficacy of 5-fluorouracil bleb needling performed 1 year or more posttrabeculectomy: a retrospective studyJ Glaucoma200918214414819225352
- MaestriniHACronembergerSMatosoHDLate needling of flat filtering blebs with adjunctive mitomycin C: Efficacy and safety for the corneal endotheliumOpthalmology2011118755762
- AnandNKhanALong-term outcomes of needle revision of trabeculectomy blebs with mitomycin C and 5-fluorouracil: a comparative safety and efficacy reportJ Glaucoma200918751352019223788
- Gracía García-MiguelTGutiérrez-DíazEMontero RodríguezMSarmiento TorresBManagement of encapsulated blebs after glaucoma drainage device surgeryArch Soc Esp Oftalmol2002778429433 Spanish12185618
- JinzaKSaikaSKinKOhnishiYRelationship between formation of a filtering bleb and an intrascleral aqueous drainage route after trabeculectomy; evaluation using ultrasound biomicroscopyOphthalmic Res20003224024310971187
- KaushikSTiwariAPandavSSIchhpujaniPGuptaAUse of ultrasound biomicroscopy to predict long-term outcome of sub-Tenon needle revision of failed trabeculectomy blebs: a pilot studyEur J Opthalmol2011216700707
- [No authors listed]The fluorouracil filtering surgery study group. Five-year follow-up of the Fluorouracil Filtering Surgery Study. Fluorouracil Filtering Surgery Study GroupAm J Ophthalmol19961213493668604728
- ChangSHHouCHNeedling revision with subconjunctival 5-fluourouracil in failing filtering blebsChang Gung Med J20022529710311952278
- MazeyBJSiegelMJSiegelLIDunnSPCorneal endothelial toxic effect secondary to fluorouracil needle bleb revisionArch Opthalmol19941121411
- PasternackJJWandMShieldsMBAbrahamDNeedle revision of failed filtering blebs using 5-Fluorouracil and a combined ab-externo and ab-interno approachJ Glaucoma200514475115650604