Abstract
Purpose
The purpose of this retrospective study was to evaluate the characteristic features, including spectral-domain optical coherence tomography (SD-OCT), clinical course, and outcome of treatment if given for patients with optic disc pit maculopathy.
Methods
We investigated a consecutive series of patients with a diagnosis of optic pit maculopathy treated between 2001 and 2012 at the Bascom Palmer Eye Institute. Patients were divided into two main groups, ie, patients who were observed without surgery and patients who received surgical intervention. The main outcome measures were presenting and final visual acuity, and changes in SD-OCT imaging were recorded. Other data including age, gender, eye, age of onset, length of follow-up, location of optic pit, and location of fluid by OCT were also recorded.
Results
On OCT, 67% (12/18) of the eyes showed schisis-like cavities, 22% (4/18) had only subretinal fluid, and 17% (3/18) had only a schisis-like cavity without subretinal fluid. In the patients managed by observation, visual acuity was ≥20/200 in 6/8 eyes initially and 6/8 eyes at last follow-up. Ten of 18 patients received either focal laser, surgery or both. Six of 10 eyes undergoing surgery had initial visual acuity ≥ 20/200, and 8 of 10 eyes undergoing surgery had a visual acuity of ≥20/200 at last follow-up.
Conclusion
In this study, many eyes were observed and remained stable during follow-up. In eyes with reduced vision, surgical intervention produced variable outcomes, and persistent intraretinal/subretinal fluid was a common occurrence.
Introduction
First described by Wiethe in 1882, optic disc pits are small, gray-white, oval depressions found at the optic nerve head.Citation1 Optic pits are a relatively rare clinical entity, with an estimated incidence of one in 11,000 people. Men and women are affected equally, and optic pits usually appear sporadically.Citation2–Citation4 They are usually found on the inferotemporal border of the optic nerve head, and 25%–75% of patients have macular involvement.Citation4,Citation8 Visual loss in patients with optic pits may be associated with retinoschisis and/or serous retinal detachment involving the macula.
Unanswered questions surrounding this condition include the origin of the macular fluid and the variable clinical features seen in individual patients. Although many reports have been published on the subject, the majority of publications are limited to case series and brief reports because of the rarity of this entity.Citation5–Citation7 Lincoff et al proposed that fluid from optic pits forms a schisis-like cavity in the retina initially, then progresses to a retinal hole in the outer layer and allows fluid to track subretinally.Citation9 However, subsequent optical coherence tomography (OCT) studies have shown serous detachment associated with optic disc maculopathy without schisis-like cavities.Citation10–Citation12
The purpose of the current study is to report a consecutive series of patients at a university referral center over a 10-year period, including presenting features, clinical course, and spectral-domain OCT documenting the status of the macula.
Materials and methods
The University of Miami institutional review board approved this retrospective study, which was conducted in accordance with the principles of the Declaration of Helsinki. The inclusion criteria were a diagnosis of optic disc pit and presentation between the years 2001 and 2011. All data were obtained via a retrospective chart review and entered into a standard computerized database for subsequent analysis. Patients were divided into two main groups, ie, patients with optic pit maculopathy who were observed without surgery and patients with optic pit maculopathy who received surgical intervention. The data collected included demographics (age and gender), visual acuity, surgical information, OCT findings, clinical characteristics of the optic pit, and complications. Patients without maculopathy, those who did not undergo OCT imaging, and those who had only one visit and no follow-up were excluded.
Results
In the current series of 18 eyes, the mean age of patients at diagnosis was 27.9 years. There were nine male and nine female patients. Four of the patients presented with bilateral optic nerve pits. Nine of 18 pits were inferotemporal, seven were temporal, and two were inferior. Median length of follow-up was 19.5 months (). The visual acuity of the patients who had optic pit maculopathy and were observed without surgery is shown in . Six of a total of eight patients had ≥20/200 vision on presentation, which remained unchanged at the last follow-up. The average length of follow-up was 95.5 (range 3–310) months.
Table 1 Demographics and clinical characteristics
Table 2 Optic pit maculopathy observed without surgery
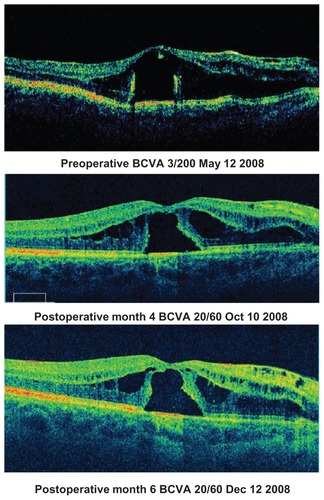
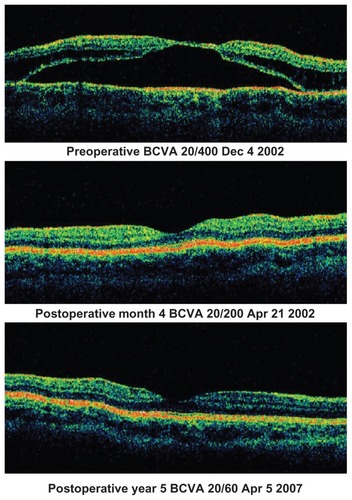
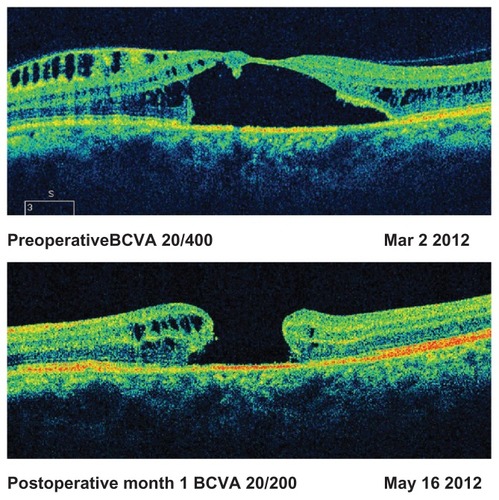
The visual acuity of 10 patients with optic pit maculopathy who had either surgery or laser is shown in . Of these 10 patients, two received only laser; six patients had ≥20/200 visual acuity on presentation and eight had ≥20/200 visual acuity at the last follow-up. The average length of follow-up was 71.6 (range 6–310) months. In the surgical group, persistent subretinal or intraretinal fluid occurred in four of seven patients. One patient had severe retinal pigment epithelium atrophy limiting postoperative visual acuity, and another patient developed a macular hole after surgery ().
Table 3 Optic pit maculopathy receiving intervention
OCT findings for all the patients with optic pit maculopathy are described in . The location of the fluid was most often in the outer nuclear layer or in the subretinal space, although a significant portion of patients also had fluid in the inner nuclear layer. Twelve of 18 patients had a schisis-like cavity in the macula on OCT. – shows the sequential OCT images of representative patients with varying clinical courses.
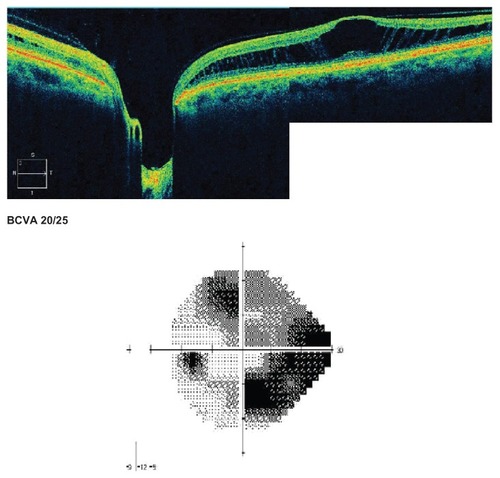
Figure 1 Observed patient with progression of schisis-like cavity over 6 year period.
(Patient one, )
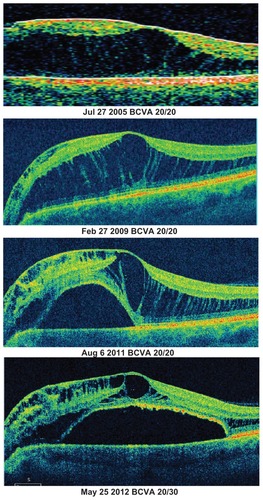
Table 4 Location of fluid for all optic pits with maculopathy on optical coherence tomography
Discussion
Observational studies have shown that long-standing macular retinal detachment from optic pits is generally associated with poor visual acuity.Citation13 Poor visual acuity (<20/200) on presentation is another predictor of poor visual outcome in these patients. In the observed patients, all with ≥20/200 vision on presentation maintained that degree of vision over a reasonable follow-up duration. The patients who presented with poor vision (<20/200) and were observed did not have visual improvement during follow-up. This is likely because of loss of photoreceptors which, in many cases, can be seen on SD-OCT. and both show significant macular schisis cavities which were able to maintain 20/25 vision for greater than 10 years. This is likely because the schisis-like cavity had not affected the foveal center, and although they maintained excellent Snellen acuity, a visual deficit is seen in the visual field in . However, in both of these cases, the schisis-like cavity remained stable over a long period with no significant changes.
SD-OCT findings in the observed group revealed many cases with schisis-like cavities, and also a number of cases with only subretinal fluid. SD-OCT studies of optic pits have shown that most cases of optic pit maculopathy have schisis-like cavities on SD-OCT.Citation14 The fluid is most often observed in the outer nuclear layer, as described in prior OCT studies of optic pit maculopathy. However, macular fluid can be found in any of a number of layers. It is unclear if location of the fluid plays a role in how stable the vision will be if observed. The most common postoperative finding on OCT is persistent intraretinal or subretinal fluid, which may have limited the final visual acuity.
In the current series, many of the patients with optic pit maculopathy were observed. Surgical intervention had mixed benefit in the treatment of this rare condition. Variability in type of intervention may have contributed to the different visual and anatomical outcomes, and is certainly a limitation of this study. SD-OCT enables improved understanding of the anatomical changes and visual impact of optic pit maculopathy.
Acknowledgments
This work was supported in part by Research to Prevent Blindness, New York, NY, and a core grant from the National Eye Institute (P30-EY14801).
Disclosure
The authors report no conflicts of interest in this work.
References
- WietheTA case of optic nerve deformityArch Augenheilkd1882111419
- ReisWA little known deformity of the optic nerve: circumscribed pit formation of the optic discArch Augenheilk190819505528 German
- HalbertsmaKCrater-like hole and coloboma of the disc associated with changes at the maculaBr J Ophthalmol192711111718168589
- KranenburgECrater-like holes in the optic disc and central serous retinopathyArch Ophthalmol19606491292413753957
- SugarHSCongenital pits of the optic disc and their equivalents (congenital colobomas and colobomalike excavations) associated with submacular fluidAm J Ophthalmol1967632983074959901
- GassJDMSerous detachments of the macula secondary to congenital pit of the optic nerve headAm J Ophthalmol1969678218415795739
- MustonenEVaronenTCongenital pit of the optic nerve head associated with serous detachment of the maculaActa Ophthalmol1972506896984678544
- BrownGCShieldsJAPattyBEGoldbergRECongenital pits of the optic nerve head. I. Experimental studies in collie dogsArch Ophthalmol19799713411344454276
- LincoffHLopezRKreissigIYannuzziLCoxMBurtonTRetinoschisis associated with optic nerve pitsArch Ophthalmol198810661673337708
- RutledgeBKPuliafitoCADukerJSHeeMRCoxMSOptical coherence tomography of macular lesions associated with optic nerve head pitsOphthalmology1996103104710538684793
- KrivoyDGentileRLiebmannJMImaging congenital optic disc pits and associated maculopathy using optical coherence tomographyArch Ophthalmol19961141651708573019
- LalwaniGAPunjabiOSFlynnHWJrKnightonRWPuliafitoCADocumentation optic nerve pit with macular schisis-like cavity by spectral domain OCTOphthalmic Surg Lasers Imaging20073826226417552399
- BrownGCShieldsJAGoldbergRECongenital pits of the optic nerve head. II. Clinical studies in humansOphthalmology19808751657375086
- ImamuraYZweifelSAFujiwaraTFreundKBSpaideRFHigh-resolution optical coherence tomography findings in optic pit maculopathyRetina2010301104111220523264