Abstract
Background
The frontalis suspension technique is the surgical method of choice in patients with ptosis and a levator function of 4 mm or less. Several types of materials have been used, including Gore-Tex®, which has been used successfully as a frontalis sling material since 1986. Recently, a Gore-Tex sheet (wider than a sling or strip) suspension was reported. This paper reports the results of 27 eyes from 20 patients with congenital ptosis treated using the frontalis suspension technique with the newly developed Gore-Tex Most Versatile Patch (MVP) sheet.
Methods
All patients underwent surgery between April 2007 and September 2011 and were followed up for at least one year. The average follow-up duration was 18 months, with a range of 12–36 months. The average patient age was 45 (5–85) years, and the group included 11 males and nine females. Thirteen cases demonstrated ptosis in one eye, and seven cases involved both eyes. The patients were divided by age into a younger group and an older group. All ptosis procedures were performed using the Gore-Tex MVP sheet. The implant was normally 7 mm wide for adults and 5 mm wide for children. The implantation method was the same as that used for the sheet shape fascia.
Results
In all patients, satisfactory functional results were observed at the 6-month follow-up examination. Eyelid opening heights were also obtained. The average marginal reflex distance (MRD) was −0.5 mm preoperatively, which improved to +1.9 mm after surgery. After one year, average MRD was +1.6 mm. MRD attenuation was more frequent in the younger group. There were no cases requiring redo surgery and only one case of exposure.
Introduction
The frontalis suspension technique is the surgical method of choice in patients with ptosis and a levator function of 4 mm or less. Several types of material have been used, including expanded polytetrafluoroethylene (Gore-Tex®), which has been used successfully as a frontalis sling material since 1986.Citation1 Sheet-type fascia implantation for frontalis suspension has been reported by plastic surgeons.Citation2,Citation3 Recently, frontalis suspension using a Gore-Tex sheet was also reported.Citation4 To avoid leakage of fluid, Gore-Tex has been improved to have a triple-layer wafer structure, marketed as PDX®. To lessen glare under the microscope, a new dual-surface Most Versatile Patch (MVP) type of Gore-Tex was developed. This material has been assessed for frontalis suspension only in Japanese patients.Citation5 We used this material in 27 eyes from 20 patients, followed them for at least one year, and describe herein the surgical technique and results achieved.
Materials and methods
In this retrospective study, we performed frontalis suspension procedures for patients with congenital or severe ptosis using a Gore-Tex MVP sheet at the Hyogo College of Medicine Hospital and Ide Eye Hospital between April 2007 and September 2011. We selected 27 eyes from 20 cases that we could follow for at least one year. We then checked their records for any complications and marginal reflex distance (MRD) changes at 6 months and one year after surgery. MRD was judged on the basis of photographs taken before and after surgery. The differences in prevalence among the category variables were compared using the χ2 test, and the P value was calculated.
Cases
All patients underwent surgery between April 2007 and September 2011 and were followed for at least one year. The average follow-up duration was 18 (range 12–36) months. The average patient age was 45 (range 5–85) years and included 11 males and nine females. Thirteen cases demonstrated ptosis in one eye, and seven cases involved both eyes. The patients were divided by age into a younger group and an older group. The younger group (average age 10 [range 5–17] years) included 12 eyes from nine patients (four boys and five girls). The older group (average age 72 [56–85] years) included 15 eyes from 11 patients (seven males and four females, see ).
Table 1 Age distribution of patients
Surgery
All ptosis procedures were performed using the Gore-Tex MVP sheet. The implant was normally 7 mm wide for adults and 5 mm wide for children. The sheet was originally 60 × 100 mm, and was cut uniformly to 7 × 45 mm (a sufficient length for all patients) before surgery, packed individually, and then sterilized using ethylene oxide gas. The surgery was performed under general anesthesia in children and under local anesthesia in adults.
A skin incision was made 5 mm from the eyelid margin for children and 6 mm for adults. This incision forms a lid crease in the oriental eyelid. Vertical lateral skin marker lines showed the margin of the pupil, and a long middle line showed the pupil center (). After traction sutures were positioned above and below the incision, the orbicularis palpebrae was observed and incised until the tarsal plate was exposed. The lowest part of the aponeurosis was pulled caudally, and the orbital fat was then observed (). An 8 mm wide skin incision was made just above the eyebrow. A tunnel was bluntly dissected to maintain the depth of orbital fat from the brow frontalis muscle to the tarsus using mosquito forceps. By way of the tunnel, the orbital septum was penetrated using the forceps tip. The Gore-Tex sheet was inserted into the tunnel by pulling back the forceps.
Figure 1 (A) A skin incision was made 5 mm from the eyelid margin for children and 6 mm for adults. This incision was used to create a lid crease in the oriental eyelid. Vertical lateral skin marker lines show the pupil margin and a middle long line shows the pupil center. (B) After the traction sutures were positioned above and below the incision, the orbicularis palpebrae was observed and incised until the tarsal plate was exposed. The lowest part of the aponeurosis was pulled caudally, and the orbital fat was then observed. (C) Gore-Tex® strips (tarsal part) were sutured with 7-0 Prolene using a 3/8-circle round needle (to avoid tearing the sheet) at one half to one third the height of the tarsal plate. Two Prolene sutures were needed to fix one strip on the tarsus. This photograph shows the mid course of surgery. (D) The cranial (frontalis) part of the Gore-Tex sheet was sutured to the frontalis muscle using 7-0 Prolene while eye opening was confirmed.
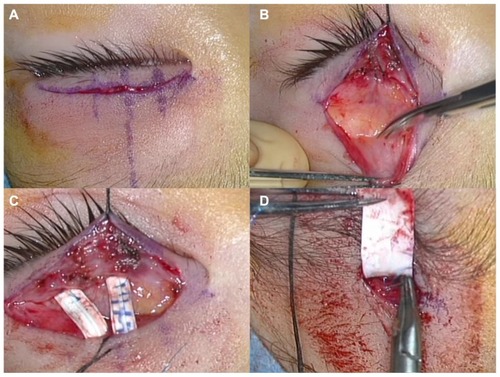
The caudal (tarsal) side of the Gore-Tex sheet was divided into double 8 mm long strips. These strips were sutured with 7-0 Prolene and a 3/8-circle round needle (using care to avoid tearing the sheet) at one half to one third the height of the tarsal plate (). The cranial (frontalis) side of the sheet was sutured to the frontalis muscle using 7-0 Prolene while opening of the eye was confirmed (). The patients under local anesthesia were required to sit on the surgical table during surgery, and their eyelid heights were measured. The target MRD was 2–3 mm; however, if manual closing could not shut the eye, the MRD needed downward adjustment. If the opening height of the eyelid was not adequate, the suture was cut at the frontalis part, and the sheet was adjusted until optimal opening was achieved. The brow and eyelid incisions were sutured with 7-0 Nylon for adults and 7-0 Vicryl for children. Oral and topical ofloxacin ointments were spread to prevent infection.
Results
Satisfactory functional results were observed at follow-up in all patients ( and ). The levator function had been less than 4 mm before surgery; however, eyelid elevation was enabled by frontalis muscle contraction. Patients who had lesser levator function and younger patients were better at blinking. In addition, eyelid opening heights were also maintained for 6 months. The average MRD was −0.46 mm preoperatively, but improved significantly to +1.89 mm by 6 months after surgery (P < 0.0001). After one year had passed, the MRD was attenuated to 1.65 mm (P = 0.05). MRD in the younger age group at one year after surgery was relatively lower than that in the older group (1.46 versus 1.8 mm, P = 0.04).
Table 2 Eyelid height before and after surgery
Table 3 Recurrence rate according to age group
Ten of 27 (37%) operated eyes experienced partial recurrence, which was more common in the children. Fifty-eight percent of the eyes in the younger age group showed partial recurrence, with an average MRD of 0.4 mm, whereas 20% of the eyes in the older age group attenuated at 0.1 mm. The incidence was higher in the younger group (P = 0.04). However, no case has needed redo surgery at the time of writing.
One case of exposure of the Gore-Tex sheet occurred. This was in a 71-year-old man who experienced more bleeding than the other patients, and wound recovery was slow. At 2 months after surgery, the Gore-Tex sheet was visible in the wound, and a skin infection had occurred. The infection was treated conservatively with iodine sterilization and antibiotic ointment for 2 months, but the eyelid skin did not cover the exposure area. Finally, the 5 mm edge of the Gore-Tex sheet over the tarsus was removed, after which shrinkage of the tunnel still occurred, along with mild lagophthalmos, although no corneal damage was seen. He experienced a mild sensation of suspension, which made eyelid closure slightly difficult.
A 5-year-old boy () and a 76-year-old female () are shown as representative successful cases.
Figure 2 A 5-year-old boy with a congenital ptosis of the left eye.

Figure 3 A 76-year-old woman with congenital ptosis in both eyes.

Discussion
In Japan, both oculoplastic surgeons and plastic surgeons perform frontalis suspension surgeries. Plastic surgeons prefer to use autologous material, (ie, fascia lata, fascia temporalis) and sometimes fabricate harvested fascia into slings. Recently, sheet-type materials have become popular because they require only one tunnel and are more easily adjusted than strips or slings.Citation2,Citation3 In contrast, oculoplastic surgeons prefer using artificial material to avoid an accessory wound, bleeding, and extended surgical time. Several artificial materials (eg, nylon suture, silicone rods) have been used for congenital ptosis surgery, and Gore-Tex is becoming a popular material for frontalis suspension.Citation6–Citation8
Gore-Tex is a well known microporous material, which is often used in brain or cardiac surgery.Citation9,Citation10 To avoid leakage of fluid, Gore-Tex PDX was improved with a triple-layer wafer structure. Also, to lessen glare under the microscope, a dual-surface type of Gore-Tex MVP was developed with a textured and smooth surface (). In our procedure, which followed the technique reported by Kanemori,Citation5 the textured surface is buried in contact with the orbicularis or dermis, while the smooth surface stays in contact with the orbital fat or septum.
Figure 4 Photograph showing the textured and smooth dual surface of the MVP® sheet magnified under a microscope.
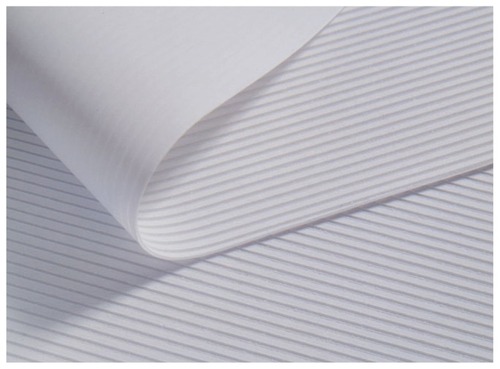
The Gore-Tex sheet is available in various sizes and can be cut into any form needed during surgery. At our institution, the width of the MVP sheet is 5–7 mm, which is wider than a sling. Once we tried a 10 mm wide sheet, but it was found to be too bulky for the oriental eyelid. As an additional advantage, its striped nature helps the surgeon to cut the sheet vertically and horizontally in a straight line.
The thickness of an MVP sheet is 0.3 mm, which is thin enough to suspend the eyelid. The normal Gore-Tex sheet is softer and more pliable than MVP. Because of the sheet-like shape, the surface area that attaches to the frontalis portion is larger than that of slings or strips. Therefore, we suggest that the suspension achieves more stable traction than linear traction. The partitioning dual strips were fixated at the nasal and middle parts of the tarsus and would have contributed to the acceptable contour at the eyelid margin. Our results also indicate that the tensile strength of the Gore-Tex sheet remains stable for a relatively long time and results in less need for redo surgery (0%).
One reportCitation8 has indicated a higher infection rate with Gore-Tex if it is not soaked in an antibiotic solution before use. Gore-Tex has a microporous structure which may allow proliferation of bacterial contaminants and lead to abscess formation.Citation8 In our series, the Gore-Tex sheet was divided and sterilized by ethylene oxide gas preoperatively. No cases of infection occurred despite lack of soaking in an antibiotic solution.
The micropores are too small to allow infiltration of fibrovascular tissues.Citation11 However, sheath formation around Gore-Tex material has been reported.Citation12 In addition, capsular formation around the Gore-Tex sheet might enable easy removal or manipulation to adjust eyelid height after surgery.
We experienced one case of exposure (4%), for which we followed a conservative course of management as reported,Citation13 but unfortunately, removal of the Gore-Tex was necessary. In this case, eyelid shrinkage continued after the exposed portion of Gore-Tex was removed. The cause of the shrinkage is unknown, but may be related to a foreign body reaction. Fibrovascular tissue is reportedly strong enough to maintain a sufficient upper eyelid height even after removal of the material.Citation6 In sum, its unique biocompatible surface, together with its thinness, may contribute to a lower exposure rate.
It is commonly assumed that the frontalis suspension procedure will promote contracture of the eyelid in younger patients because the length between the brow and eyelid gets wider as the face grows. In addition, the implanted fascia sometimes shrinks after surgery.Citation3,Citation14 The incidence in children is higher than in older patients (58% versus 20%, P = 0.04). If the strips are not adjustable in length, the eyelid contour will contract in children. However, the 0.4 mm decrease suggests material expansion, tearing of loose tissue, or an anatomical defect in the patient. In our opinion, preadolescent patients are likely to stop using the frontalis muscle because they become tired of holding the eyelid open and are not vigilant about their appearance (). Yoon and Lee reported the same problem,Citation15 observing an attenuation of approximately 0.4 mm during one year of follow-up by using autologous fascia lata. Among our cases, we observed no severe recurrent cases, with MRD of 0 mm or under and no patients requiring redo surgery. However, with longer follow-up, severe recurrence or cases with contraction requiring reoperation may develop.
Conclusion
Experimentally, we have shown that frontalis suspension using a Gore-Tex sheet is safe and effective. Although there was a high rate of partial recurrence, no redo surgeries were necessary. Further observation is needed for more comprehensive evaluation of this technique.
Disclosure
The authors report no conflicts of interest in this work.
References
- AdenisJPLebraudPMathonMUse of polytetrafluoroethylene (Goretex) in the palpebrofrontalis muscle suspension in ptosisJ Fr Ophtalmol198710607609 French3443710
- MatsuoKYuzurihaSFrontalis suspension with fascia lata for severe congenital blepharoptosis using enhanced involuntary reflex contraction of the frontalis muscleJ Plast Reconstr Aesthet Surg20096248048718249045
- FanJFrontalis suspension technique with a temporal-fasciae-complex sheet for repairing blepharoptosisAesthetic Plast Surg20112514715111426303
- TakahashiYLeibovitchIKakizakiHFrontalis suspension surgery in upper eyelid blepharoptosisOpen Ophthalmol J201014919721331314
- KanemoriYFrontalis suspension for blepharoptosis with polytetrafluoroethyleneJournal of the Eye200825545548 Japanese
- SteinkoglerFJKucharAHuberEArocker-MettingerEGore-Tex soft-tissue patch frontalis suspension technique in congenital ptosis and in blepharophimosis-ptosis syndromePlast Reconstr Surg199392105710608234502
- Ben SimonGJMacedoAASchwarczRMWangDYMcCannJDGoldbergRAFrontalis suspension for upper eyelid ptosis: evaluation of different surgical designs and suture materialAm J Ophthalmol200514087788516214102
- WassermanBNSprungerDTHelvestonEMComparison of materials used in frontalis suspensionArch Ophthalmol200111968769111346396
- YamagataSGotoKOdaYKikuchiHClinical experience with expanded polytetrafluorethylene sheet used as an artificial dura materNeurol Med Chir (Tokyo)1993335825857692335
- HaradaYImaiYKurosawaHHoshinoSNakanoKLong-term results of the clinical use of an expanded polytetrafluoroehylene surgical membrane as a pericardial substituteJ Thorac Cardiovasc Surg1988968118153184974
- ZweppHPSpauwenPHMEvaluation of expanded polytetrafluoroethylene and autogenous fascia lata in frontalis suspensionActa Chir Plast1992341291371284263
- UgurbasSCKocerNEOtoSKaharamanBAkovaYAComparison of alloplast materials in experimental extraocular muscle surgeryOphthalmic Res201044505620215807
- DetorakisETTsilimbarisMKSuccessful conservative management of expanded polytetrafluoroethylene band exposure in frontalis suspensionOphthal Plast Reconstr Surg200925416417
- DoraCDDimarcoDSZobitzMEElliottDSTime dependent various in biomechanical properties of cadaveric fascia, porcine dermis, porcine small intestine submucosa, polypropyrene mesh and autologous fascia in the rabbit model: implications for sling surgeryJ Urol20041711970197315076323
- YoonJSLeeSYLong-term functional and cosmetic outcomes after frontalis suspension using autogenous fascia lata for pediatric congenital ptosisOphthalmology20091161405141419481809