Abstract
Purpose
To determine if qualitatively defining the appearance of optic disc change was a valid characteristic of myopia in subjects with Graves’ ophthalmopathy (GO) or primary open-angle glaucoma (POAG).
Methods
We defined typical tilt appearance as the simultaneous presence of the following: an elliptical optic disc, a crescent, unequal sharpness of the cupping margin (horizontally), and nasally displaced vessels in the optic cup. Ninety-two eyes from 92 subjects each with GO or with POAG and no severe complications were included in the study after matching for spherical refractive errors. Using our definition of tilt appearance, two independent observers subjectively judged optic disc photographs. One observer repeated judgments in 70 randomly selected eyes and judgment reproducibility was assessed using kappa statistics. Tilt ratio was used as a quantitative parameter.
Results
The numbers of eyes judged as having a typical tilt appearance in the GO group and in the POAG group were 25 (27.2%) and 39 (42.4%), respectively, by one observer (P = 0.0297), and 12 (13%) and 44 (47.8%), respectively, by another observer (P < 0.0001). Intra- and interobserver reproducibility of tilt judgment were very good (kappa = 0.93) and good (kappa = 0.65), respectively. Tilt ratio did not significantly differ between the two groups. Analytical results including background factors were essentially the same for the two observers: multivariate logistic regression for one observer’s judgment showed that the presence of the typical tilt appearance was associated with belonging to the glaucoma group (odds ratio [OR], 6.25; P = 0.0054), tilt ratio (OR per 0.01, 0.77; P < 0.0001), and spherical refractive error (OR per diopter, 0.80; P < 0.003).
Conclusion
The optic disc feature we designated as typical tilt was associated with myopia, and its frequency was higher in subjects with POAG compared to those with GO.
Introduction
Myopic eyes are often accompanied by tilted optic discs, which are associated with a series of findings, including a vertically oval optic disc,Citation1–Citation3 nasally undermined cupping, Citation1,Citation4 nasally displaced vessels in the cupping,Citation1,Citation3,Citation4 and the presence of a temporal crescent.Citation1–Citation3,Citation5 In our clinical practice in Japan, we observed that an optic disc with the simultaneous presence of the aforementioned features is a common finding and that these features occur more frequently in glaucoma patients than in patients with other ocular diseases. However, there are few reports describing this observation in the literature, which may suggest an association between this characteristic morphology with the pathological process involved in glaucomatous nerve damage.
Several objective parameters are used to evaluate characteristics associated with optic discs in myopic eyes. Among these are the ratio of minimum-to-maximum optic disc diameter (tilt ratio);Citation6 the ratio of horizontal-to-vertical optic disc diameter;Citation7,Citation8 the degree of optic disc rotation;Citation9–Citation11 the ratio of the maximum width of the peripapillary atrophy to the vertical disc diameter;Citation7,Citation8 an angle between a line fitted to the optic disc surface and a reference horizontal line in a cross-sectional optical coherence tomography image;Citation10 and an area of peripapillary atrophy.Citation11 However, findings expressed by these parameters seem to be limited, particularly regarding the characteristic appearances of the cupping and vessels mentioned above, which may be too qualitative to be expressed by objective parameters. Thus, we may be required to qualitatively and/or subjectively identify and define a typical form of myopic tilted disc.
On the other hand, qualitative definitions for tilted discs associated with myopia have been made on the basis of actual nerve tilting observed in stereoscopic views,Citation12–Citation14 presence of a crescent,Citation12 different steepness of the neuroretinal rim surface according to locations within the disc,Citation12 and the ovalness of the optic disc.Citation12,Citation14 It is apparent that an established qualitative definition that includes the characteristic appearances of cupping and vessels described above is not available at present. In addition, the reproducibility of procedures defining those characteristics is unknown.
Considering this background, we defined new subjective criteria for defining a typical form of myopic tilted disc and observed its frequency in patients with primary open-angle glaucoma (POAG) and in patients with Graves’ ophthalmopathy (GO), which was used as a representative ocular disease other than glaucoma. We also evaluated the reliability of this new judging system and explored potentially relevant factors, including tilt ratio, as objective parameters.
Materials and methods
Study design
In this observational, cross-sectional study, the frequency of the optic disc feature we designated as typical tilt appearance was determined in a group of patients with GO and a group of patients with POAG, including normal-tension glaucoma. The study and data accumulation were carried out with the approval of the institutional review board of the Asai Dermatology Clinic, Yokohama, Kanagawa, Japan, which is an organization that conducts reviews for outside facilities. The data collecting facility (Olympia Eye Hospital, Shibuya, Tokyo, Japan) specializes not only in glaucoma, but also in thyroid-associated eye diseases, and the number of clinical records in the facility was expected to be sufficient enough to provide candidates who fulfilled the inclusion criteria described below.
The following conditions were considered inclusion criteria for both groups of patients: (1) patients were examined between December 2002 and June 2005 at the Olympia Eye Hospital and clinical records included refractometry, visual acuity testing, slit-lamp biomicroscopy and fundoscopy (both with dilated pupils), and digital fundus photography with high-quality results, taken with a Kowa VX-10i (Kowa Company Ltd, Nagoya, Aichi, Japan) or Canon CR5-NM (Canon Inc, Ota, Tokyo, Japan) camera; (2) the age at onset of each disease ≥ 20 years; (3) no apparent complication of ocular lesions except their original disease (GO or glaucoma), mild superficial punctate keratopathy, incipient cortical cataract, tessellated fundus, or peripapillary crescents; and (4) no history of intraocular surgery.
Apart from these common criteria, the following were considered as inclusion criteria for patients in the GO group: (1) a diagnosis of GO on the basis of findings including clinical manifestations, endocrinological examinations, and orbital MRI; (2) having undergone applanation tonometry or noncontact tonometry; (3) best-corrected visual acuity in decimal unit ≥ 1.0; (4) without complicating compressive optic neuropathy attributable to Graves’ ophthalmopathy; (5) proptosis, if present, was not sufficiently severe to be indicative for orbital decompression surgery. In terms of NOSPECS classification (classification of Graves’ eye disease),Citation15 patients with categories 2b, 2c, 5b, 5c, 6a, 6b, or 6c were excluded.
In addition to the common criteria above, the following were considered inclusion criteria for patients in the glaucoma group: (1) a diagnosis of POAG or normal-tension glaucoma; (2) having undergone applanation tonometry, gonioscopy, Goldman perimetry, and static perimetry (Octopus program 32 or G2); (3) localized glaucomatous visual field defects earlier than stage 5 of the Aulhorn–Greve classificationCitation16 that were reproducible in two or more repeated perimetric results; and (4) retinal nerve fiber bundle defect and/or decreased neural rim width in the optic disc, each corresponding to the visual field defect, clearly confirmed from the fundus photographs.
Only one eye per patient was selected so that the spherical refractive error was matched for both groups. The distribution of eyes with a range of spherical refractive errors were divided into groups every three diopters (D). Matching was performed because the frequency of the typical tilt appearance was expected to be affected by refractive errors. In patients in whom both eyes were eligible, the eye with the more severe visual field defect was chosen for the glaucoma group and a randomly selected eye was chosen for the GO group.
Definition and evaluation of typical tilt appearance
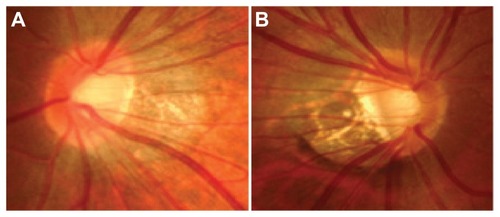
We considered the following four elements as features typically observed in optic discs in myopic eyes: (1) a vertically elliptical optic disc contour;Citation1–Citation3 (2) the presence of a temporal crescent;Citation1–Citation3,Citation5 (3) a blurred cup margin on the temporal side and a clear margin on the nasal side (we designated this as horizontally unequal sharpness of the cupping margin);Citation1,Citation4 and (4) retinal vessels displaced nasally and concealed by the nasal rim as they exited the eye (we designated this the nasally displaced vessels in the cupping).Citation1,Citation3,Citation4 We then defined the simultaneous presence of all four features as the typical tilt appearance (). Although the term “tilt” was originally used to describe a finding in which the optic nerve head is depressed in the temporal margin compared to the nasal margin, optic discs with our definition of typical tilt appearance usually share this three-dimensional characteristic. Citation1 Also, our definition is not intended to be applied to findings associated with tilted disk syndrome,Citation17 in which inferiorly and nasally tilting of the optic disc is observed.
Figure 1 Optic disc photographs fulfilling our criteria of the typical tilt appearance. (A) A subject with Graves’ ophthalmopathy. (B) A subject with glaucoma, in which a nerve fiber layer defect is recognized around the inferior temporal position of the optic disc.
According to these criteria, two independent, well-experienced ophthalmologists (TT as observer 1 and RI as observer 2), who were not involved in patient selection, subjectively judged the presence or absence of the typical tilt appearance. When being judged, optic disc photographs were displayed on a liquid crystal display with an arbitrary magnification, and any other clinical information was completely masked. No distinction was required between a crescent that was purely a myopic change or if it was accompanied by atrophic changes attributable to glaucoma or aging.Citation18,Citation19 To examine intraobserver reliability, one observer (observer 1) reevaluated photographs from 35 subjects randomly selected from each of the GO group and the glaucoma group 1–2 weeks after the initial assessment.
Assessment of the tilt ratio
Ovality of the optic disc was expressed as the tilt ratio (the ratio of minimum-to-maximum optic disc diameter).Citation6 In our measurement, the minimum disc diameter was defined as the width of the optic disc measured on the bisector perpendicular to the maximum disc diameter. An examiner (SY) who was not involved in the judgment of the optic disc appearance performed the diameter measurements using the Shape Tool in the software Photoshop Elements (v 4.0; Adobe Systems Inc, San Jose, CA, USA), while masked to all other clinical information.
Evaluation of data and statistical analyses
Mann–Whitney U tests and the chi-square tests were used for comparisons between the two groups. Multivariate logistic regression was used to determine the association between the presence of the typical tilt appearance and other factors as explanatory variables that included age, sex, spherical refractive error, intraocular pressure, disc ovality ratio, and group type (GO or glaucoma). For intraocular pressure, the average of two values measured on separate days was used. Although intraocular pressure had not been measured using a unified method for all the subjects, this difference was not considered when included in the analyses. The association between the optic disc appearance and use of ocular hypotensive agents in the glaucoma group subjects was not analyzed because we assumed that such an association was too complex to be evaluated properly in this retrospective study.
Kappa statistics were used to assess intra- and interobserver agreement for the methods used to judge the presence of the typical tilt appearance. Intraobserver kappa values were calculated from the paired data judged by observer 1. Interobserver kappa values were calculated from the paired data judged by the two observers. The strength of agreement was interpreted on the basis of the kappa values suggested by Altman,Citation20 as adapted from the method of Landis and Koch:Citation21 kappa values of 0.81–1.00 indicated very good agreement; 0.61–0.80, good agreement; 0.41–0.60, moderate agreement; 0.21–0.40, fair agreement; and 0.20 or lower, poor agreement. Software JMP (v 7.0.2; SAS Institute Inc, Cary, NC, USA) was used for all statistical analyses.
Results
After matching spherical refractive error (), 92 eyes from 92 patients were selected for the GO group and for the glaucoma group. All 184 patients were considered Japanese based on their names. Characteristics of the subjects of both groups are summarized in . There were statistically significant but unintentional differences in age and sex between the two groups. The tilt ratio did not show a significant difference between the two groups. None of the patients in the GO group had undergone perimetry because it was not ordered by their physicians. The number of ocular hypotensive ophthalmic solutions used in the glaucoma group subjects was 1 ± 0.9 (mean ± standard deviation) and 33 subjects (35.9%) did not use any hypotensive agents.
Table 1 Distribution of the spherical refractive errors matched for the Graves’ ophthalmopathy group and the glaucoma group
Table 2 Characteristics of the Graves’ ophthalmopathy group and the glaucoma group
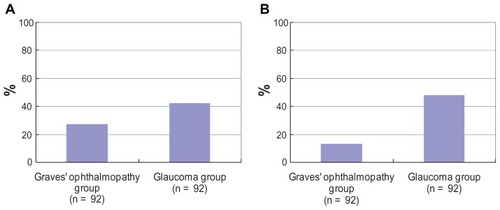
The judgment results of the two independent observers were similar and both showed a significant difference in the frequency of the typical tilt appearance between the two groups (): according to the judgment by observer 1, the number of eyes with the typical tilt appearance was 25 (27.2%) in the GO group (n = 92) and 39 (42.4%) in the glaucoma group (n = 92) (P = 0.0297 between the two groups); according to observer 2, the number was 12 (13%) in the GO group (n = 92) and 44 (47.8%) in the glaucoma group (n = 92) (P < 0.0001 between the two groups).
Figure 2 Frequency of eyes judged as having the typical tilt appearance by two independent observers. (A) Observer 1; (B) observer 2.
summarizes the kappa statistics calculated from the subjective judgments for the presence of the typical tilt appearance. Interobserver agreement was moderate for the GO group, good for the glaucoma group, and good for both groups as a whole. Intraobserver agreement was very good for the GO group, very good for the glaucoma group, and very good for both groups as a whole.
Table 3 Reliability of the judgments for the presence of the typical tilt appearance
We analyzed the associations between the background factors and optic disc appearance judged by each observer. Because the analytical results were essentially the same for both observers’ judgments, we will present the results from the data judged by observer 1 throughout the rest of this section. summarizes the relevance of the background factors and the judged status of the optic disc appearance in the GO group, and for the glaucoma group. Only in the glaucoma group were subjects with the typical tilt appearance significantly younger than subjects without. In both groups, spherical refractive error was more myopic in subjects with the typical tilt appearance than in subjects without. In addition, the tilt ratio was smaller in subjects with the typical tilt appearance than in subjects without in both groups. summarizes the results of multivariate logistic regression for the presence of typical tilt appearance in which both groups were analyzed as a whole. Similar to the results of simple comparisons, a greater degree of myopia, smaller disc ovality ratio, and having glaucoma were factors having a significant association with the presence of typical tilt appearance. On the other hand, the effect of age was not significant, contrary to the result of the simple comparison in the glaucoma group (). Thus, we consider the association of age with the typical tilt appearance in the glaucoma group simply a visual result caused by confounding variables.
Table 4 Relevance of background factors on optic disc appearance in the Graves’ ophthalmopathy group
Table 5 Relevance of background factors on optic disc appearance in the glaucoma group
Table 6 Results of multivariate logistic regression for the effects on the presence of typical tilt appearance
Discussion
We defined a qualitative optic disc feature consisting of four elements as the typical tilt appearance () and observed its frequency in subjects with POAG and in subjects with GO under a condition in which the refractive error was matched for both groups of subjects. According to subjective judgments by each of the two independent observers, the typical tilt appearance was determined to be a familiar finding in both of the current subject groups, and was associated with a higher degree of myopia and smaller tilt ratios, whereas its frequency was higher in the glaucoma group than in the GO group. Considering that the tilt ratio is an index correlating with the degree of myopia,Citation6 our observations may support the assumption that the typical tilt appearance we defined is a characteristic entity of optic disc types seen in myopic eyes. To the best of our knowledge, this is the first attempt to validate a qualitative definition of an optic disc appearance consisting of several features as a typical myopic type. However, instances of optic disc photographs seeming to fulfill our definition may be found in previously published papers that dealt with optic disc findings in Asian subjects with myopia.Citation7,Citation8–Citation11,Citation13,Citation14,Citation22–Citation24
On the basis of the results of the kappa statistics (), the intraobserver and interobserver reliability in this study was sufficient for us to consider the subjective judging system using our criteria acceptable to evaluate an optic disc appearance. In addition, the similarity of two independent observers’ judgments with respect to the fact that the frequency of the typical tilt appearance differed significantly between the two groups () may be a finding that supports the reproducibility of the judging system.
The significant association between the tilt ratio and the myopic tilted disc was expected because our criteria included an elliptical optic disc contour, although it was judged subjectively. At the same time, this finding suggests that our judging system for the typical tilt appearance succeeded in retaining characteristics resembling the tilt ratio. However, in spite of the similarity of the two parameters, the distribution of the tilt ratio did not show a significant difference between the GO group and the glaucoma group, unlike the frequency of the typical tilt appearance. These dissociative observations may indicate a difficulty in substituting the tilt ratio alone for the qualitative optic disc features that we defined as the typical tilt appearance. In addition, such a difficulty probably arose from essential differences between the two parameters, in that the tilt ratio does not incorporate three of the four elements that the typical tilt appearance does: the temporal crescent, horizontally unequal sharpness of the cupping margin, and nasally displaced vessels in the cupping. Alternatively, it is natural to assume that these three features presented with a higher frequency in the glaucoma group than in the GO group, although both the tilt ratio and the refractive error were distributed equally between the two groups.
The difference in the frequency of the typical tilt appearance between the two groups may suggest some underlying mechanisms. For example, in eyes with glaucoma, the crescent may appear or become exaggerated with peripapillary atrophy,Citation18,Citation19 and an excavation of the cupping may occur, especially in the nasal region, and these acquired changes could enhance the appearance of myopic tilted disc. Conversely, such changes may not occur as readily in subjects with GO, although, to the best of our knowledge, the association of myopic optic disc changes with GO has not been previously studied. On the other hand, it is possible that the appearance of the tilted discs had already presented to a marked degree and remained relatively stationary from before the onset of the disease in the glaucoma group. Consistent with this possibility, Doshi et alCitation22 hypothesized a causative contribution of tilted disc to the occurrence of nerve fiber damage that corresponded to a diagnosis of glaucoma from their frequent observations of such morphology in a series of young myopic male Chinese patients.
However, the association between group type and the typical tilt appearance in our observation does not prove that a presence of glaucomatous nerve damage is associated with the typical tilt appearance, because the complete normality of visual function of the current subjects in the GO group was not proven as they had not undergone visual field testing. Studies using glaucoma subjects as well as subjects with normal visual function may be worthwhile to determine associations with myopic optic disc changes and glaucomatous nerve damage. The current study only indicates a possibility that the frequency of a typical tilt appearance may differ according to the type of complicating ocular disease.
There are limitations to this study. For instance, in judging optic disc appearances, we employed an all-or-nothing system; thus, some cases judged as not having the typical tilt appearance may have actually had a mild or moderate degree of tilted myopic disc. Methods that can classify the optic disc appearance into more detailed categories may be ideal. Next, intraocular pressure had not been measured using unified methods for all subjects and the use of ocular hypotensive agents in the glaucoma group subjects was not considered in the analyses. As a result, the data pertaining to intraocular pressure may have induced some bias to the analytical results for relevancy of background factors with the optic disc appearances. Thus, whether an associative manner of clinical factors with typical tilt appearance in this study is reproducible needs further confirmation. The accuracy of the refractive error in the GO group may be questionable and present as another limitation because a hypermetropic shift in the refraction can complicate severe cases of the disease, probably because of a flattening of the posterior globe caused by an increased volume of orbital tissues.Citation25 However, the GO group in this study did not include patients with severe proptosis indicating decompression surgery or patients with complicating compressive optic neuropathy. Therefore, we considered such a flattening effect of the globe unlikely in our subjects although further studies may be required to verify our estimation.
Conclusion
We defined an optic disc feature as typical tilt appearance, which was observed to have a considerable association with myopic eyes in subjects with POAG or GO and is thought to represent qualitative characteristics that are difficult to ascertain from the tilt ratio alone; however, the frequency of the typical tilt appearance was higher in subjects with POAG than in those with GO despite matching both groups for spherical refractive error. Further studies may be necessary to confirm our findings as well as to investigate potential associations between typical tilt appearance and other factors.
Disclosure
The authors report no conflicts of interest in this work.
References
- TanakaMStudies of the crescent, tigroid fundus and cup of the disc. Report I. Fundamental observationNihon Ganka Gakkai Zasshi195963821372143 Japanese
- YanoffMSassaniJWOcular Pathology6th edPhiladelphiaMosby2009497527
- CurtinBJThe posterior staphyloma of pathologic myopiaTrans Am Ophthalmol Soc1977756786613534
- NakaseYPrimary open angle glaucoma in high myopia. Report 2. Effect of high myopia on glaucomatous cupping of the optic discNihon Ganka Gakkai Zasshi1987914442447 Japanese3618393
- SpencerWHOphthalmic Pathology. An Atlas and Textbook3rd edPhiladelphiaWB Saunders Co1985913924
- TayESeahSKChanSPOptic disk ovality as an index of tilt and its relationship to myopia and perimetryAm J Ophthalmol2005139224725215733984
- HyungSMKimDMHongCYounDHOptic disc of the myopic eye: relationship between refractive errors and morphometric characteristicsKorean J Ophthalmol19926132351434043
- KimTWKimMWeinrebRNWooSJParkKHHwangJMOptic disc change with incipient myopia of childhoodOphthalmology20121191212621978594
- HowACTanGSChanYHPopulation prevalence of tilted and torted optic discs among an adult Chinese population in Singapore: the Tanjong Pagar StudyArch Ophthalmol2009127789489919597111
- HwangYHYooCKimYYCharacteristics of peripapillary retinal nerve fiber layer thickness in eyes with myopic optic disc tilt and rotationJ Glaucoma201221639440021946540
- ParkHYLeeKParkCKOptic disc torsion direction predicts the location of glaucomatous damage in normal-tension glaucoma patients with myopiaOphthalmology201211991844185122595297
- LimLGazzardGChanYHCorneal biomechanics, thickness and optic disc morphology in children with optic disc tiltBr J Ophthalmol200892111461146618703551
- SamarawickramaCMitchellPTongLMyopia-related optic disc and retinal changes in adolescent children from SingaporeOphthalmology2011118102050205721820741
- KumarRSBaskaranMSinghKAungTClinical characterization of young Chinese myopes with optic nerve and visual field changes resembling glaucomaJ Glaucoma201221528128621623224
- WiersingaWMPrummelMFMouritsMPKoornneefLBullerHRClassification of the eye changes of Graves’ diseaseThyroid1991143573601841734
- GreveELLangerhorstCTvan den BergTTJPPerimetry and other visual function tests in glaucomaCairnsJEGlaucomaLondonGrune and Stratton19863777
- YoungSEWalshFBKnoxDLThe tilted disk syndromeAm J Ophthalmol19768211623937453
- JonasJBFernándezMCNaumannGOGlaucomatous parapapillary atrophy. Occurrence and correlationsArch Ophthalmol199211022142221736871
- FantesFEAndersonDRClinical histologic correlation of human peripapillary anatomyOphthalmology198996120252919048
- AltmanDGPractical Statistics for Medical ResearchLondonChapman and Hall1991396439
- LandisJRKochGGThe measurement of observer agreement for categorical dataBiometrics1977331159174843571
- DoshiAKreidlKOLombardiLSakamotoDKSinghKNonprogressive glaucomatous cupping and visual field abnormalities in young Chinese malesOphthalmology2007114347247917123617
- NakazawaMKurotakiJRuikeHLong-term findings in peripapillary crescent formation in eyes with mild or moderate myopiaActa Ophthalmol200886662662918577184
- NakazawaTFuseNOmodakaKAizawaNKuwaharaSNishidaKDifferent types of optic disc shape in patients with advanced open-angle glaucomaJpn J Ophthalmol201054429129520700795
- ChandrasekaranSPetsoglouCBillsonFASelvaDGhabrialRRefractive change in thyroid eye disease (a neglected clinical sign)Br J Ophthalmol200690330730916488951