Abstract
We report a case of cytomegalovirus (CMV) retinitis in an immunocompetent patient who was resistant to antiviral treatment, and in whom fatal metastatic liver cancer was later detected. A 74-year-old Japanese man visited our ophthalmology clinic in May 2011. He had a history of well controlled type 2 diabetes and colon cancer, and underwent successful surgical treatment in 2008. In April 2011, he was diagnosed with uveitis affecting his left eye and received posterior sub-Tenon injection of triamcinolone acetonide. He was referred to us because of aggravation of the retinal lesion. Funduscopic examination of the left eye revealed arcuate, whitish, necrotizing retinitis with hemorrhage along the temporal arcade of the retina. Polymerase chain reaction of the aqueous fluid was positive for CMV DNA. Because of diagnosis of CMV retinitis in his left eye, he was referred to an internist and investigated for systemic CMV infection or any serious disease which could cause immunocompromise, but neither was detected. Despite an intensive course of intravitreous ganciclovir and oral valganciclovir, the retinitis did not resolve. In June 2012, 14 months after the initial ocular symptoms, metastatic liver cancer was found and the patient passed away. When CMV retinitis is resistant to antiviral treatment or recurs in an immunocompetent patient, it is important that ophthalmologists undertake systemic investigation for occult malignancy.
Introduction
Cytomegalovirus (CMV) retinitis is one of the most common opportunistic ocular infections in immunocompromised patients. However, there have been recent reports that immunocompetent patients can also develop CMV retinitis. These patients had common risk factors, including old age, a history of intraocular surgery, intraocular administration of steroids, and diabetes. The ocular prognosis of these patients is not serious and the retinitis is usually treated successfully by antiviral agents, eg, ganciclovir and valganciclovir. Here we report a case of CMV retinitis in an immunocompetent patient in whom initial antiviral treatment was effective, but when therapy was discontinued, the retinitis regressed, and metastatic cancer was detected during subsequent follow-up.
Case report
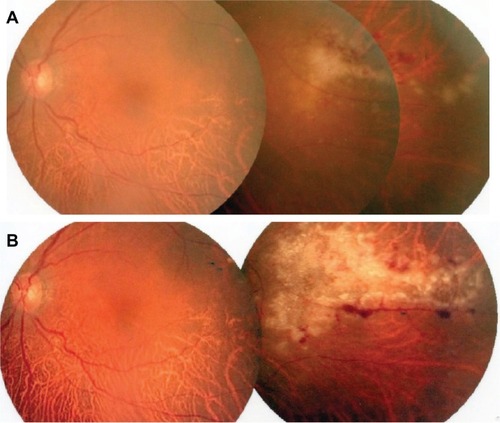
A 74-year-old Japanese man visited our ophthalmology clinic in May 2011. He had a history of well controlled type 2 diabetes and colon cancer, which had been treated successfully by surgical removal in 2008. In April, 2011 he was diagnosed as having uveitis in his left eye () which was unsuccessfully treated with posterior sub-Tenon injection of triamcinolone acetonide 20 mg. Because of aggravation of the retinal lesion, he was referred to us on May 7, 2011. His best corrected visual acuity was 0.9 OD and 1.2 OS. On slit-lamp examination of the left eye, there were no cells in the anterior chamber, but 1+ vitreous cells were observed. Funduscopic examination of the left eye revealed arcuate, whitish, necrotizing retinitis with hemorrhage along the temporal arcade of the retina (). On blood investigation, human T lymphotropic virus-1 antibody and CMV IgG were positive, but human immunodeficiency virus antibody, toxoplasma, herpes simplex virus IgM/IgG, varicella zoster virus IgM/IgG, and CMV IgM were negative. CD4 was 50.5% and CD8 was 21.0%, ie, the CD4/CD8 ratio was 2.4 (reference range 0.6–2.9). Angiotensin-converting enzyme was 7.2 mU/mL (reference range 8.3–21.4) and HbA1c was 6.5% (reference range 4.6–6.2).
Figure 1 Fundus photographs of the left eye. (A) Whitish retinitis with slight hemorrhage, observed on April 1, 2011. (B) Aggravation of retinitis and hemorrhage on May 6, 2011 (26 days after sub-Tenon injection of triamcinolone acetonide).
On May 11, 2011, 0.1 mL of aqueous fluid was collected from the left eye by 30 gauge needle under topical anesthesia and submitted for polymerase chain reaction. The result was positive for CMV DNA and negative for herpes simplex and varicella zoster virus DNA. With a diagnosis of CMV retinitis in his left eye, he was referred to an internist before commencement of antiviral treatment to determine if he suffered from systemic CMV infection or any serious disease which could make him immunocompromised, but neither was detected.
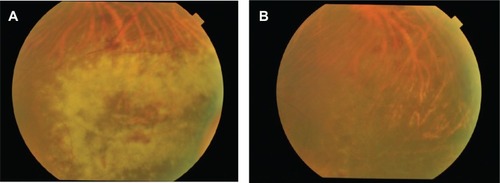
Intravitreous injections of ganciclovir 500 μg and 1000 μg were given on May 25 and June 11, 2011 respectively. Because of a poor response, oral valganciclovir 1800 mg/day was also initiated on June 28, 2011. This was effective, tapered to 900 mg/day on July 22, 2011, and discontinued on August 20, 2011. A month later the patient’s retinitis regressed, and he resumed oral valganciclovir 1800 mg/day on September 22, 2011, which was tapered to 900 mg/day on October 21, 2011. His CMV retinitis regressed again, and he received a third intravitreous ganciclovir injection at a dose of 1000 μg on November 17, 2011. shows the course of treatment and shows fundus photographs taken on June 28 and August 20, 2011.
Figure 2 The patient received a course of treatment.
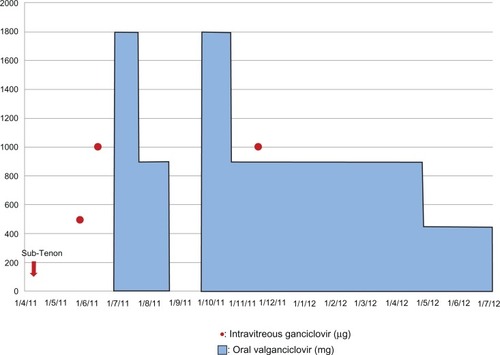
Figure 3 Fundus photographs of the left eye. (A) The retinal lesion did not resolve after intravitreous ganciclovir injection, and oral valganciclovir 1800 mg/day was initiated on June 28, 2011. (B) Resolution of retinitis was observed and valganciclovir was discontinued on August 20, 2011.
Best corrected visual acuity in his left eye was generally good, (variable between 0.7 and 1.2) except for the last two visits on May 11 and July 4, 2012. By this time he had developed posterior capsular opacification caused by chronic inflammation and senile cataract, and best corrected visual acuity of the left eye was 0.4 on May 11, 2012 and 0.2 on July 4, 2012. He was taking oral valganciclovir 450 mg/day at the last visit, but metastatic liver cancer was found in June 2012, and the patient passed away not long afterwards.
Discussion
It is now thought that CMV infection in immunocompetent patients is more common than was previously thought.Citation1 There have been reports of severe complications of CMV infection, including colitis, meningoencephalitis, pneumonitis, hematological disorders, and venous and arterial thrombosis.Citation1 CMV retinitis has been widely believed to affect mainly immunosuppressed patients with acquired immunodeficiency syndrome and a low CD4 cell count, those on long-term treatment with immunosuppressive agents, and neonates. However, there have been several reports of CMV retinitis in immunocompetent patients.Citation1–Citation8 These patients had risk factors in common, ie, old age, a history of intraocular surgery, intraocular administration of steroids, and diabetes.Citation1–Citation8
It is not clear how CMV becomes reactivated in immunocompetent patients. Sites of chronic infection are known, including monocytes, bone marrow-derived myeloid progenitors, endothelial cells, and the smooth muscle cells of blood vessels. Kercher et alCitation9 reported murine CMV persisting in ocular tissue could be reactive, but Vogel et alCitation10 suggested that the human eye (retina) was not a site of persistent CMV infection. Recent studies suggest that CMV retinitis could be caused by infiltration of virus-infected cells circulating in the retina.Citation11 It is assumed that reactivated CMV spreads hematologically to infect the retina. In diabetes, it has been reported that leukocytes are less deformable and that circulation of blood in the retina is significantly decreased.Citation12 Therefore, leukocytes could be trapped more easily in the capillary circulation of the retina.Citation11 Chen et alCitation13 also reported that dyslipidemia could induce inflammatory adhesion molecules in human retinal vascular endothelial cells. Dyslipidemia is generally observed in both elderly and diabetic patients, who may be exposed to risk factors for adhesion of activated CMV in the retina.
Immunological status is usually assessed by peripheral blood investigations, which include CD4/CD8 ratio and immunoglobulin levels. In the absence of abnormal findings in these tests or other systemic symptoms, patients are usually deemed to be immunocompetent. Although the present patient had a history of colon cancer, it was treated successfully by surgical removal and he had not taken anticancer medicine for 30 months when he had the initial ocular symptoms. Therefore, he was not considered to be immunosuppressed as a result of colon cancer or its treatment. According to previous reports, the ocular prognosis of CMV retinitis in immunocompetent patients is not serious, and the retinitis can usually be treated successfully by administration of ganciclovir and/or valganciclovir.Citation2–Citation5,Citation7 There have also been reports of some cases that did not require antiviral treatment and others in which retinitis has resolved spontaneously with steroid eye drops.Citation6,Citation8 Our patient had undergone an intensive course of antiviral treatment with intravitreous ganciclovir and oral valganciclovir, but the retinitis did not resolve, and 14 months after his initial ocular symptoms, colon cancer metastasis to the liver was detected. We suspect that, in spite of the normal CD4/CD8 result, this patient was immunocompromised, at least in the retina, so could not respond adequately to treatment.
According to surveys conducted in Japan and the US, CMV is a common viral infection. In Japan, Nishimura et alCitation14 reported that the rate of CMV IgG antibody seropositivity was 67.7% in pregnant women younger than 25 years, and Numazaki et alCitation15 reported that 83.9% of pregnant women at 10–12 weeks of gestation were seropositive. In the US, Staras et alCitation16 reported that CMV seroprevalence increased gradually with age and was 90.8% in those older than 80 years. The positive CMV IgG and negative CMV IgM result in our patient indicated that he had been infected by CMV previously. Because he was 74 years of age and diabetic, it is possible that onset of CMV retinitis was associated with his known risk factors of diabetes and old age. Certainly it is important to suspect CMV and obtain aqueous humor for polymerase chain reaction before treatment of retinitis in patients with these risk factors. In addition, it was obvious that this patient’s retinitis had been aggravated by sub-Tenon injection of triamcinolone acetonide prior to referral to us. Intraocular steroids have benefits in the treatment of inflammation, although their side effects are also widely recognized. However, because of their simplicity, ophthalmologists are inclined to administer steroids without enough consideration. This could be a trigger for local reactivation of CMV.
According to past reports, the prognosis of CMV retinitis in immunocompetent patients is not critical. In the present case, the patient passed away without complete resolution of his retinitis. It was possible that our early treatment was inadequate, and we could have performed intravitreous ganciclovir injections regularly once a week for induction therapy, as suggested by an earlier study.Citation17 However, the patient was diagnosed as immunocompetent at 74 years of age, his visual acuity was good, and he did not want frequent invasive therapy. When CMV retinitis is resistant to antiviral treatment or recurs in an immunocompetent patient, as in this case, it is important for ophthalmologists to order systemic investigations to exclude serious occult disease.
Disclosure
The authors report no conflicts of interest in this work.
References
- RafailidisPIMourtzoukouEGVarbobitisICFalagasMESevere cytomegalovirus infection in apparently immunocompetent patients: a systematic reviewVirol J200854718371229
- SaidelMABerreenJMargolisTPCytomegalovirus retinitis after intravitreous triamcinolone in an immunocompetent patientAm J Ophthalmol200514061141114316376669
- DelyferMNRougierMBHubschmanJPAouizérateFKorobelnikJFCytomegalovirus retinitis following intravitreal injection of triamcinolone: report of two casesActa Ophthalmol Scand200785668168317403022
- SekiryuTIidaTKanekoHSaitoMCytomegalovirus retinitis after intravitreal triamcinolone acetonide in an immunocompetent patientJpn J Ophthalmol200852541441618991048
- VertesDSnyersBDe PotterPCytomegalovirus retinitis after low-dose intravitreous triamcinolone acetonide in an immunocompetent patient: a warning for the widespread use of intravitreous corticosteroidsInt Ophthalmol201030559559720931263
- YoshinagaWMizushimaYAbematsuNNakaoKSakamotoTCytomegalovirus retinitis in immunocompetent patientsNihon Ganka Gakkai Zasshi20088684687 Japanese.18767494
- StewartMWBollingJPMendezJCCytomegalovirus retinitis in an immunocompetent patientArch Ophthalmol2005123457257415824240
- ChoWBKimHCMoonJWSpontaneous resolution of intravitreal steroid-induced bilateral cytomegalovirus retinitisKorean J Ophthalmol201226215115522511845
- KercherLMitchellBMPersisting murine cytomegalovirus can reactivate and has unique transcriptional activity in ocular tissueJ Virol200276189165917512186900
- VogelJUFleckensteinCWagnerMThe human eye (retina): a site of persistent HCMV infection?Graefes Arch Clin Exp Ophthalmol2005243767167615672249
- MiyamotoKHiroshibaNTsujikawaAOguraYIn vivo demonstration of increased leukocyte entrapment in retinal microcirculation of diabetic ratsInvest Ophthalmol Vis Sci19983911219021949761301
- SchröderSPalinskiWSchmid-SchönbeinGWActivated monocytes and granulocytes, capillary nonperfusion, and neovascularization in diabetic retinopathyAm J Pathol19911391811001713023
- ChenWJumpDBGrantMBEsselmanWJBusikJVDyslipidemia, but not hyperglycemia, induces inflammatory adhesion molecules in human retinal vascular endothelial cellsInvest Ophthalmol Vis Sci200344115016505014578429
- NishimuraNKimuraHYabutaYPrevalence of maternal cytomegalovirus (CMV) antibody and detection of CMV DNA in amniotic fluidMicrobiol Immunol199943878178410524796
- NumazakiKFujikawaTChibaSRelationship between seropositivity of husbands and primary cytomegalovirus infection during pregnancyJ Infect Chemother20006210410611810545
- StarasSADollardSCRadfordKWFlandersWDPassRFCannonMJSeroprevalence of cytomegalovirus infection in the United States, 1988–1994Clin Infect Dis20064391143115117029132
- Cochereau-MassinILehoangPLautier-FrauMEfficacy and tolerance of intravitreal ganciclovir in cytomegalovirus retinitis in acquired immune deficiency syndromeOphthalmology1991989134813531658703