Abstract
Background
The purpose of this study was to evaluate prospectively the efficacy of a topical carbonic anhydrase inhibitor in macular edema after vitrectomy.
Methods
Forty patients were included, all of whom had undergone vitrectomy combined with phacoemulsification and intraocular lens implantation for epiretinal membrane. Twenty eyes from 40 patients received topical 2% dorzolamide three times a day. The patients were followed up for at least 3 months. In this study, we evaluated the effect of dorzolamide on visual acuity, intraocular pressure, central macular thickness, and aqueous flare.
Results
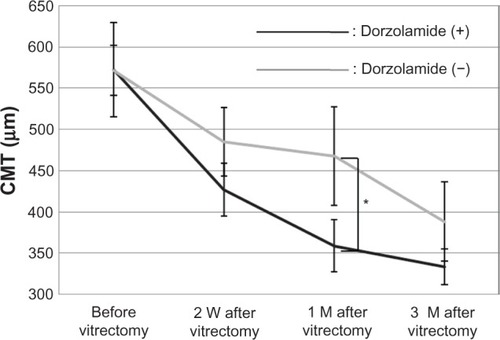
Mean logarithm of the minimum angle of resolution (logMAR) best-corrected visual acuity preoperatively and 2 weeks, 1 month, and 3 months after surgery was 0.48 ± 0.23, 0.60 ± 0.16, 0.40 ± 0.29, and 0.24 ± 0.32, respectively, in the treatment group, and 0.40 ± 0.09, 0.44 ± 0.12, 0.32 ± 0.10, and 0.16 ± 0.09, respectively, in the control group. No statistically significant difference was observed between the two groups. Mean central macular thickness preoperatively and at 2 weeks and 3 months after surgery was 572.6, 427.2, and 333.4 μm, respectively, in the treatment group, and 571.4, 485.2, and 388.4 μm, respectively, in the control group. Mean aqueous flare preoperatively, and 1 month and 3 months after surgery was 8.6, 34.2, and 23.5 photon counts per millisecond (pc/ms), respectively, in the treatment group, and 9.7, 24.7, and 23.4 pc/ms, respectively, in the control group. No statistically significant differences were observed between data from the two groups. However, statistically significant (P < 0.05) differences in mean central macular thickness at 1 month and mean aqueous flare at 2 weeks after surgery were found between the treatment group (358.8 μm, 36.8 pc/ms) and the control group (467.8 μm, 64.0 pc/ms). Differences in mean intraocular pressure preoperatively and at 2 weeks, 1 month, and 3 months after surgery were not statistically significant between the two groups. Intraocular pressure never exceeded 21 mmHg.
Conclusion
Topical dorzolamide significantly reduced mean central macular thickness at 1 month and mean aqueous flare at 2 weeks after surgery for epiretinal membrane compared with controls. Although further investigation of more cases and longer follow-up are needed, this study suggests that topical dorzolamide can be efficacious in reducing macular edema in the early phase after vitrectomy via its anti-inflammatory effect.
Introduction
Dorzolamide is a topical carbonic anhydrase inhibitor and is used widely in the treatment of glaucoma. Macular edema results from breakdown of the blood-retinal barrier, vitreous traction, and damage to the retinal pigment epithelial cells, leading to accumulation of intracellular and extracellular fluid.Citation1–Citation7 Macular edema occurs in a variety of pathologic conditions, including diabetic retinopathy, central and branch retinal vein occlusions, uveitis, retinitis pigmentosa, epiretinal membrane, and other nutritional and metabolic diseases, as well as after surgery. Recently, clinical interest has focused on retinal disorders as an indication for this drug. Since the first report by Cox in 1988,Citation8 several authors have described a positive effect of acetazolamide on the resolution of macular edema from various etiologies, including uveitis and postoperative inflammation after cataract extraction,Citation9 retinitis pigmentosa,Citation10 and serpiginous choroiditis,Citation11 and in conjunction with epiretinal membrane.Citation12 Findings on optical coherence tomography and improvement in visual acuity have demonstrated that dorzolamide has a curative effect on the macular cystic cavities found in congenital X-linked retinoschisis,Citation13 choroideremia,Citation14 and retinitis pigmentosa.Citation15 The pathogenesis of macular edema often involves a multifactorial background. We have reported that dorzolamide had an anti-inflammatory effect in a comparative study of eye drops in the treatment of glaucoma.Citation16 In that research, we studied the efficacy of dorzolamide in the treatment of macular edema and inflammation, based on our experience of administration of dorzolamide eye drops to treat ocular hypertension after vitreous surgery. To study the efficacy of a drug for macular edema, an ideal subject should have macular edema that results from a single cause, and the cause should be removed. In this study, we chose patients who underwent vitrectomy and removal of epiretinal membrane. The purpose of this study was to determine the efficacy and safety of topical dorzolamide for treating macular edema.
Materials and methods
Forty patients with macular edema following removal of epiretinal membrane and who fulfilled the criteria for this study were enrolled. Any patients with pre-existing ocular disease (glaucoma, high myopia, chronic inflammatory, or neoplastic disorders), a systemic disorder (eg, diabetes or uncontrolled hypertension), or a known life-threatening disease were excluded prior to enrolment. The study was approved by the institutional review board at our institution. Patients were informed of the purpose of our study and provided their signed consent to participate. This study prospectively evaluated the primary outcomes of visual acuity, intraocular pressure, central macular thickness, and aqueous flare. The surgical technique used was 23-gauge pars plana vitrectomy. All patients underwent phacoemulsification and polyacrylic intraocular lens implantation (AN6K, Kowa, Tokyo, Japan). A vitrectomy was done with prior application of triamcinolone acetonide (Kenacort-A®, Bristol Pharmaceuticals, Tokyo, Japan). In all eyes, the posterior hyaloid membrane was separated from the retinal surface with suction from the vitreous cutter. In the present study, the epiretinal membrane was removed using microforceps intraoperatively, but intentional removal of the internal limiting membrane was not performed in all cases. However, we could not exclude accidental removal of the internal limiting membrane during surgery. Postoperative treatment consisted of levofloxacin 0.5%, dexamethasone 0.02%, and diclofenac 0.1% eye drops applied topically three times daily for 1 month and oral cefcapene pivoxil hydrochloride 75 mg or 100 mg three times daily for 5 days, in all cases, in both groups. Twenty patients were randomly assigned in a prospective manner to receive dorzolamide three times a day. To evaluate the effects of treatment, all patients underwent a detailed ophthalmic examination, including slit-lamp biomicroscopy, optical coherence tomography, and a laser flare cell meter test (FC-2000, Kowa). Foveal configuration and retinal thickness were determined by optical coherence tomography, and retinal thickness was defined as the distance between the vitreoretinal interface and the retinal pigment epithelium in the center of the fovea. Aqueous flare was evaluated using a slit-lamp as well as a laser flare cell photometer, as described in detail in previous studies.Citation17,Citation18 Calibration was performed each day according to the manufacturer’s instructions, to ensure accurate measurements. Measurements were taken in a standardized fashion by the same experienced technician who was blinded as to the medical condition of the patients. From each eye, three individual measurements were averaged, and measurements contaminated by artifacts were discarded. Flare reading was expressed as photon counts per millisecond (pc/ms). Best-corrected visual acuity was examined using the decimal visual acuity system in 40 eyes, which was converted to the logarithm of the minimum angle of resolution (logMAR) scale. Goldmann tonometry was used to determine intraocular pressure. Safety was evaluated by determining the incidence of treatment-related complications and adverse reactions for both the treatment and control groups. The differences between the treatment group and the control group were assessed for statistical significance using the Student’s t-test when appropriate. A level of P < 0.05 was accepted as being statistically significant.
Results
Mean logMAR best corrected visual acuity preoperatively, and at 2 weeks, 1 month, and 3 months after surgery was 0.48 ± 0.23, 0.60 ± 0.16, 0.40 ± 0.29, and 0.24 ± 0.32, respectively, in the treatment group, and 0.40 ± 0.09, 0.44 ± 0.12, 0.32 ± 0.10, and 0.16 ± 0.09, respectively, in the control group. No statistically significant difference between the two groups was observed (). The difference in mean intraocular pressure preoperatively, and at 2 weeks, 1 month, and 3 months after surgery between the treatment group and the control group was not statistically significant. Intraocular pressure never exceeded 21 mmHg (). Mean central macular thickness preoperatively and at 2 weeks, and 3 months after surgery was 572.6, 427.2, and 333.4 μm, respectively, in the treatment group, and 571.4, 485.2, and 388.4 μm, respectively, in the control group. No statistically significant difference between the two groups was observed, except that the difference in mean central macular thickness at 1 month after surgery was statistically significant (P < 0.05, see and ) between the treatment group (358.8 μm) and the control group (467.8 μm).
Figure 1 The mean logMAR best-corrected visual acuity preoperatively and at 2 weeks (W), and 1 and 3 months (M) after surgery was not significantly different between the treatment and control groups.
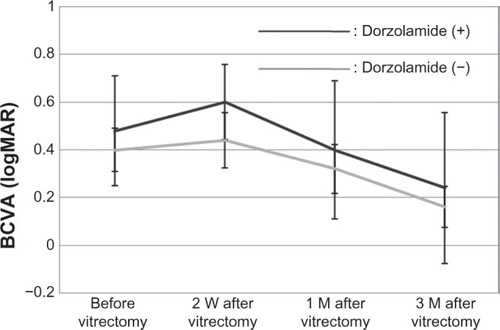
Figure 2 The mean intraocular pressure preoperatively and at 2 weeks (W), and 1 and 3 months (M) after surgery was not significantly different between the treatment and control groups, and intraocular pressure never exceeded 21 mmHg.
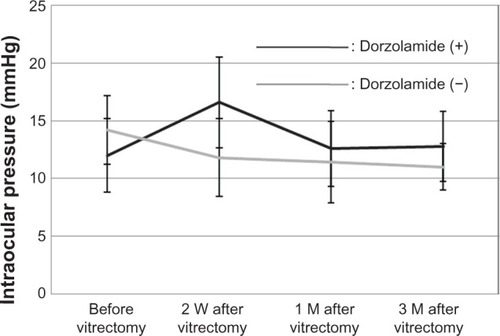
Figure 3 Fundus photography (A and B), and horizontal optical coherence tomography (OCT) macular scans (a and b) before and 1 month after vitrectomy and removal of epiretinal membrane (nontreatment). Fundus photography (C and D), and horizontal OCT macular scans (c and d) before and 1 month after vitrectomy and removal of epiretinal membrane (dorzolamide treatment).
Abbreviation: OCT, optical coherence tomography.
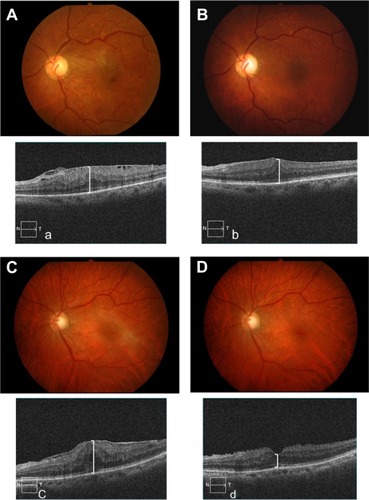
Figure 4 Mean CMT preoperatively and at 2 weeks (W), and 1 and 3 months (M) after surgery was not significantly different between the treatment and control groups, but the difference was statistically significant 1 month after surgery.
Abbreviation: CMT, central macular thickness.
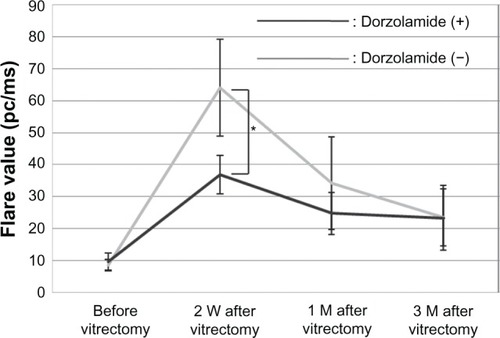
Mean aqueous flare preoperatively and at 1 month, and 3 months after surgery was 8.6, 34.2, and 23.5 pc/ms, respectively, in the treatment group, and 9.7, 24.7, and 23.4 pc/ms, respectively, in the control group. No statistically significant difference was observed between the two groups, but the difference in mean aqueous flare at 2 weeks after surgery was statistically significant (P < 0.05) between the treatment group (36.8 pc/ms) and the control group (64.0 pc/ms, see ). Patients were monitored for any possible adverse effects that could be attributed to the drugs throughout the study. No significant systemic or ocular complications or adverse events occurred during the study.
Figure 5 Mean aqueous flare preoperatively and at 2 weeks (W), and 1 and 3 months (M) after surgery was not significantly different between the treatment and control groups.
Discussion
Epiretinal membrane traction is believed to stimulate inflammation, exudates, and a leukocyte response in the macula, leading to macular edema. The efficacy of anti-inflammatory agents, including triamcinolone acetonide and topical nonsteroidal anti-inflammatories, has been demonstrated in several studies, both for the prevention and treatment of inflammatory macular edema.Citation19 We have previously reported that dorzolamide suppresses production of the proinflammatory cytokine, interleukin-6, which is a major participant in the inflammatory process.Citation16 It has been reported that in patients with rheumatoid arthritis already on 25 mg/ day of oral prednisone and 20 mg/week of intramuscular methotrexate, addition of tocilizumab, an anti-interleukin-6 receptor antibody, improved the acute-phase response (erythrocyte sedimentation rate and C-reactive protein) after 3 months of treatment.Citation20 In the present study, dorzolamide reduced aqueous flare at 2 weeks after surgery. Topical dorzolamide may suppress postsurgical inflammation, and it has been reported that subretinal fluid is removed by inhibition of membrane-bound carbonic anhydrase IV in the retinal pigment epithelium.
However, it has also been reported that the response to carbonic anhydrase inhibitor therapy is better in patients with diffuse retinal pigment epithelial disease than in those with overt retinal vascular disease, such as diabetes or retinal vein occlusion.Citation21 In this study, we chose patients who had macular edema with epiretinal membrane. Epiretinal membranes are not usually associated with changes in the retinal pigment epithelium, so carbonic anhydrase inhibitors may act little through facilitation of transport across the retinal pigment epithelium. In addition, use of a topical carbonic anhydrase inhibitor decreases the risk of the well known systemic side effects of oral carbonic anhydrase inhibitor preparations.Citation21
Our study demonstrates that topical dorzolamide may reduce central macular thickness and aqueous flare in the early period following vitrectomy. Although further investigation of more cases is needed, this study suggests that topical dorzolamide can be efficacious in reducing macular edema during the early period following vitrectomy via its anti-inflammatory effects.
Disclosure
The authors report no conflicts of interest in this work.
References
- FineSBruckerAJMacular edema and cystoid macular edemaAm J Ophthalmol1981924664817294109
- YanoffMFineSBruckerAJEagleRCJrPathology of human cystoid macular edemaSurv Ophthalmol198428Suppl5055116463850
- GassJMDAndersonDRDavisEBA clinical, fluorescein angiographic, and electron microscopic correlation of cystoids macular edemaAm J Ophthalmol198510082854014384
- BresnickGHDiabetic maculopathy. A critical review highlighting diffuse macular edemaOphthalmology198390130113176664669
- BirdACRetinal edema. Introduction to the first international cystoid macular edema symposiumSurv Ophthalmol198428Suppl4334366463845
- TsoMOMPathology of cystoid macular edemaOphthalmology1982899029157133637
- SchepensCLAvilaMPJalkhAETrempeCLRole of the vitreous in cystoid macular edemaSurv Ophthalmol198428Suppl4995046463849
- CoxSNHayEBirdACTreatment of chronic macular edema with acetazolamideArch Ophthalmol1988106119011953415543
- FarberMDLamSTesslerHHJenningsTJCrossARusinMMReduction of macular edema by acetazolamide in patients with chronic iridocyclitis: a randomized prospective crossover studyBr J Ophthalmol199478478110697
- FishmanGAGilbertLDAcetazolamide for treatment of chronic macular edema in retinitis pigmentosaArch Ophthalmol1989107144514522803090
- ChenJCFitzkeFWBirdACLong-term effect of acetazolamide in a patient with retinitis pigmentosaInvest Ophthalmol Vis Sci199031191419182211037
- MarmorMFHypothesis concerning carbonic anhydrase treatment of cystoid macular edema: example with epiretinal membraneArch Ophthalmol1990108152415252244830
- ApushkinMAFishmanGAUse of dorzolamide for patients with X-linked retinoschisisRetina20062674174516963845
- GeneadMAMcAnanyJJFishmanGATopical dorzolamide for treatment of cystoid macular edema in patients with choroideremiaRetina20123282683321886018
- IkedaYHisatomiTYoshidaNThe clinical efficacy of a topical dorzolamide in the management of cystoid macular edema in patients with retinitis pigmentosaGraefes Arch Clin Exp Ophthalmol201225080981422215259
- KawaiKOhashiHSuzukiTKitagakiHFujisawaSヒトおよびマウス末梢血単核球の炎症性サイトカイン産生に及ぼす緑内㢓治療薬の作用. [Effect of anti-glaucoma drugs on inflammatory cytokine production by human and murine peripheral blood mononuclear cells.]Nippon Ganka Gakkai Zasshi2010114669677 Japanese20803986
- YangPFangWJinHClinical features of Chinese patients with Fuchs’ syndromeOphthalmology200611347348016458965
- LadasJGWheelerNCMorhunPJLaser flare-cell photometry: methodology and clinical applicationsSurv Ophthalmol200550274715621076
- WolfensbergerTJHerbortCPTreatment of cystoid macular edema with non-steroidal anti-inflammatory drugs and corticosteroidsDoc Ophthalmol19999738138610896354
- SavinoSDanielaRDarioRInterleukin 6 blockade as steroid-sparing treatment for 2 patients with giant cell arteritisJ Rheumatol2011382080208121885526
- WolfensbergerTJThe role of carbonic anhydrase inhibitors in the management of macular edemaDoc Ophthalmol19999738739710896355