Abstract
Purpose
To report an interesting case of infectious endotheliitis of presumed mycotic origin.
Methods
A case report of a 56-year-old male farmer who sought medical attention after a month-long evolution of irritative symptoms in his right eye, accompanied by visual acuity (VA) impairment. The patient received topical and oral broad-spectrum antibiotic treatment with no improvement before being referred to a cornea specialist, where he was found to have VA of 20/150 and was noted on biomicroscopy to have endothelial feathery coalescent lesions. The patient was admitted to the hospital for an aqueous humor sample and intravenous voriconazole.
Results
The microbiological studies did not isolate any micro-organisms. However, clinical evidence of improvement was confirmed after 5 days of antimycotic intravenous therapy. Complete clinical resolution was achieved at 1 month after treatment completion with oral voriconazole, as evidenced by VA of 20/20 and disappearance of endothelial lesions.
Conclusion
Endothelial involvement by fungi is a rare condition. In this case, no microbes were isolated, but the characteristic morphology of the lesions, the history of onychomycosis, and the spectacular response to voriconazole turn this case into a valid presumptive diagnosis.
Background
The cornea is the ocular structure most commonly affected by fungi. Most often, the source of infection is exogenous, such as vegetal trauma, among others. In addition, it is associated with any disease affecting the eye’s normal surface, such as persistent epithelial defects, neurotrophic ulcers, use of contact lenses, and secondary attenuation of cell defense mechanisms after topical steroids.Citation1–Citation5
Infectious endothelial involvement of the cornea has been mainly attributed to different viral species.Citation6 However, herein we present the case of a patient with a clear endothelial infectious involvement that successfully responded to systemic antifungal therapy with voriconazole.
Case description
A 56-year-old male banana grower sought medical attention after a month-long evolution of irritative symptoms in his right eye accompanied by visual acuity (VA) impairment. His medical history confirmed excision of bilateral pterygium 15 years earlier, but no recent ocular trauma was related by the patient. However, recurrent hand and feet onychomycosis treated with fluconazole is recorded.
The general medical practitioner (nonophthalologist) initiated treatment with topical prednisolone acetate 1% and gentamicin sulfate 0.3% every 6 hours for 1 week for a presumed bacterial conjunctivitis, but the patient was referred to the ophthalmologist after lack of success with this therapy. An initial diagnosis of infectious keratitis (with unaffected epithelium but endothelial involvement) was made, and treatment with topical moxifloxacin chlorhydrate 0.5% four times per day and gentamicin sulfate 0.3% three times per day plus oral ciprofoxacin 750 mg every 12 hours was prescribed.
After 6 days on this therapeutic regimen and with lack of clinical improvement, the patient was referred to a cornea specialist. He was found with right eye VA of 20/150 and normal VA in his left eye. The biomicroscopy performed on the affected eye confirmed the integrity of the epithelium with an unruptured bulla over the pupillary area, presence of folds on Descemet’s membrane, anterior chamber cells 2+(Standardization of Uveitis Nomenclature Working Group),Citation7 and multiple coalescent circular lesions of feathery and whitish appearance on the endothelium (). Fundoscopic examination with an indirect ophthalmoscope under midriasis was normal. Based on these findings, a clinical suspicion of mycotic endothelial keratitis arose. Therefore, the patient was admitted to hospital to further explore the etiology of the lesion. For this, an aqueous humor sample was examined for fungi detection by culture and polymerase chain reaction (PCR), and systemic antimycotic therapy was initiated immediately after sample taking. By recommendation of the infectologist, the patient was empirically treated with voriconazole 200 mg intravenously (IV) every 12 hours (diluted in 250 mL of 0.9% saline solution administrated over 2 hours) and topical gatifloxacin 0.3% every 6 hours for 1 week (as post puncture antibacterial prophylaxis).
Figure 1 (A) Endothelial lesions at admission: multiple coalescent circular lesions of feathery and whitish appearance on the endothelium with intact epithelium. (B) Reduction of the lesions after 3 days of intravenous voriconazole. (C) Complete resolution after 1 month of oral voriconazole.
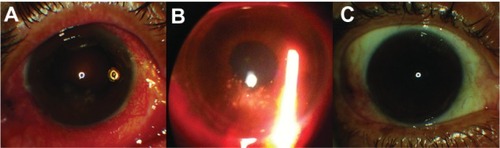
After 3 days on IV therapy with voriconazole, the patient showed significant clinical improvement, evidenced by an important decline in the number of cells within the anterior chamber and some reduction on the feathery endothelial lesions described previously. VA was 20/30 (). Aqueous humor microbiologic study was negative (Gram, potassium hydroxide staining, aerobic, anaerobic, and fungal cultures). PCR, Venereal Disease Research Laboratory, herpes simplex, and HIV testing were also negative.
After 5 days on this regimen, the patient was discharged with voriconazole 200 mg orally every 12 hours. After a week, the patient was found to have VA of 20/30, considerable improvement of endothelial lesions, and faint residual corneal edema. The same treatment regimen was administered for a further week, and fluorometholone 0.1% every 12 hours was added to therapy for edema. Examination 2 weeks after discharge confirmed further edema reduction and almost complete resolution of endothelial lesions. After 4 weeks of antifungal treatment (3 weeks of those were as an outpatient), the patient showed full edema resolution, the presence of a few small endothelial scars, and 20/20 VA (). Fluorometholone was then withheld and oral voriconazole was continued until completion of 2 months with antifungal therapy.
Discussion
Infectious endothelial involvement of the cornea has been mainly attributed to different viral species.Citation6 However, we report an interesting case of a patient whose endothelial lesions suggest mycotic etiology that successfully responded to systemic antifungal therapy with voriconazole.
Usual manifestations of fungal keratitis include epithelial and stromal ulceration, abscessing with stromal necrosis, epithelial or stromal edema and, rarely, cell reaction in the anterior chamber, hypopyon, and fibrin deposits within the anterior chamber and endothelial plates.Citation1,Citation5 Nevertheless, the most striking finding in this case was the confinement of damage to endothelial plates with subsequent central corneal edema, bulla formation, folds on Descemet’s membrane, and cell reaction in the anterior chamber. The epithelium and stroma remained unaffected. Therefore, we propose an endogenous source of infection, and postulate the presence of recurrent onychomycosis as a risk factor in the absence of prior trauma or epithelial disruption. However, microbiological isolates turned out to be negative both in blood and in aqueous humor.
A characteristic clinical sign of fungal keratitis is the irregular nature of infiltrates, traditionally described as “feathery” or “cotton wool.”Citation1,Citation4,Citation8 This feature prompted the suspicion of fungal origin in our patient, as this pattern was observed on the endothelium. Although Gram and potassium hydroxide staining, as well as PCR, were negative, our diagnosis was established on clinical grounds and confirmed by the success of empirical therapy with voriconazole.
It is important to point out that laboratory diagnosis in this case has been limited by the low volume of sample taken, which was destined for multiple studies (stains, cultures, PCR). In addition, experience with these tests and available primers in our country are also limited.
Some authors have reported on the good efficacy of intracameral injection with amphotericin B and voriconazole in cases of endophthalmitis secondary to keratitis.Citation9–Citation11 Although this is an adequate therapeutic alternative, it was not required, as the patient showed an excellent response to systemic therapy with oral voriconazole.
Conclusion
An interesting case of a presumed endogenous mycotic endotheliitis is herein reported in a patient with a history of recurrent onychomycosis who develops endothelial lesions of mycotic morphology. The patient responds to a systemic IV and oral scheme with voriconazole, and thus an endogenous and mycotic etiology is presumed. However, this could not be confirmed by microbiological studies, due to the limitations that we have cited.
Acknowledgment
The authors want to acknowledge the support given by the Hospital Pablo Tobón Uribe and Universidad Pontificia Bolivariana in Medellín, Colombia.
Disclosure
The authors declare no conflicts of interest.
References
- SrinivasanMFungal keratitisCurr Opin Ophthalmol200415432132715232472
- YildizEHAbdallaYFElsahnAFUpdate on fungal keratitis from 1999 to 2008Cornea201029121406141120847685
- KeayLJGowerEWIovienoAClinical and microbiological characteristics of fungal keratitis in the United States, 2001–2007: a multicenter studyOphthalmology2011118592092621295857
- ChangH-YPChodoshJDiagnostic and therapeutic considerations in fungal keratitisInt Ophthalmol Clin2011514334221897138
- KalkanciAOzdekSOcular fungal infectionsCurr Eye Res201136317918921158591
- SuzukiTOhashiYCorneal endotheliitisSemin Ophthalmol200823423524018584561
- Standardization of Uveitis Nomenclature for Reporting Clinical Data. Results of the first international workshopAm J Ophthalmol2005140350951616196117
- TuliSSFungal keratitisClin Ophthalmol2011527527921468333
- YilmazSTureMMadenAEfficacy of intracameral amphotericin B injection in the management of refractory keratomycosis and endophthalmitisCornea200726439840217457185
- ShenY-CWangC-YTsaiH-YLeeH-NIntracameral voriconazole injection in the treatment of fungal endophthalmitis resulting from keratitisAm J Ophthalmol2010149691692120434131
- MittalVMittalRIntracameral and topical voriconazole for fungal corneal endoexudatesCornea201231436637022410613