Abstract
A 16-year-old boy presented to the emergency department with the complaint of a sudden, painful left eye and proptosis after an episode of sneezing. A few hours earlier, he had sustained a blunt trauma to the left orbit as the result of a fistfight. The initial examination showed subcutaneous and subconjunctival emphysema. Visual acuity in the left eye was 20/30 (0.67), the pupils were reactive with no relative afferent pupillary defect, and there were mild limitations in levoduction and supraduction. A slit-lamp examination showed normal anterior and posterior segments with an intraocular pressure of 26 mmHg. An orbital computed tomography scan showed orbital, subconjunctival, and subcutaneous emphysema associated with a small fracture of the orbital floor. Following conservative management with broad-spectrum oral antibiotics, a topical antiglaucoma drug, and lubricating eye drops, the patient improved dramatically within one week.
Keywords:
Introduction
Subconjunctival emphysema, which has rarely been reported in the literature because of its uneventful course,Citation1 is associated mostly with orbital emphysema in cases of medial orbital wall fractures due to a newly created sino-orbital communication.Citation2,Citation3 While orbital emphysema may cause compressive optic neuropathyCitation4 in severe cases, subconjunctival emphysema may cause exposure keratopathy when the ability to close the lids is compromised. The patient described here developed simultaneous orbital, subconjunctival, and subcutaneous emphysema after sustaining a small fracture of the orbital floor due to a sudden elevation in intranasal pressure.
Case report
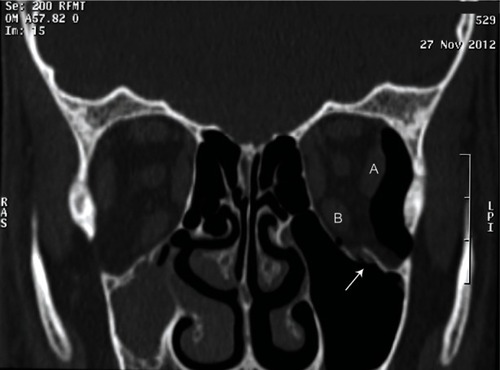
A 16-year-old boy sustained a trauma to the left orbit as the result of a fistfight. A few hours later, he developed sudden left periorbital pain, swelling, and proptosis after an episode of sneezing. He presented to the emergency department where an ophthalmologic examination showed left subcutaneous and subconjunctival emphysema (). The uncorrected visual acuity was 20/30 (0.67), and the pupillary responses were normal. There were a mild limitation in left eye levoduction and supraduction with an inability to close the lids, but no paresthesia of the cheek or teeth. A slit-lamp examination showed normal anterior and posterior segments. The intraocular pressure measured by applanation tonometry was 26 mmHg. There was 3 mm of proptosis in the left eye compared with the right eye. An orbital computed tomography scan showed a left linear, nondisplaced fracture of the orbital floor associated with peribulbar and retrobulbar emphysema without muscle entrapment or fat herniation. The emphysema caused medial displacement of the left lateral and inferior rectus muscles with mild proptosis ( and ). Uncorrected visual acuity in the right eye was 20/20 (1.0) and was normal upon examination and radiologically. The patient was treated with prophylactic broad-spectrum oral antibiotics, a topical antiglaucoma drug (timolol 0.5% twice daily), and lubricating eye drops (four times daily), and was instructed not to blow his nose and to return for a follow-up examination the next morning. After daily follow-up, there was dramatic improvement in the subcutaneous and subconjunctival emphysema and vision, with total resolution of the subconjunctival emphysema on the fifth day with no sequelae. The topical medications were stopped.
Figure 1 Left lower lid subcutaneous emphysema and medial and lateral subconjunctival emphysema (white arrow).

Figure 2 Left lower lid subcutaneous emphysema, lateral subconjunctival emphysema, and orbital emphysema.

Figure 3 Coronal orbital computed tomography scan shows a left linear, nondisplaced fracture of the orbital floor (white arrow) without muscle entrapment or fat herniation.
Discussion
Orbital emphysema most often results from a fracture of the orbital wall that allows air to enter the orbit from the paranasal sinuses.Citation5 The presence of orbital, subconjunctival, and subcutaneous emphysema may be due to air from the nasal cavity entering between the loose tissue planes of the orbit after fractures of the orbital walls.Citation3 Subconjunctival emphysema can be explained by probable communication between the subcutaneous and subconjunctival planesCitation6 or the probable spread from orbital emphysema through the orbital septum when the intraorbital pressure is high.
Subconjunctival emphysema has been reported in patients on mechanical ventilationCitation6 and after direct injury to the conjunctiva through macroscopic or microscopic conjunctival lacerations associated with injury due to compressed air.Citation7–Citation10 Subcutaneous emphysema usually occurs during a brief period after trauma when air can be forced into the tissues. After this, the escape routes are sealed by blood clots or herniated tissues in the sinuses at the fracture sites.Citation3
The current case was unusual in that it had all three types of emphysema () with a small fracture of the orbital floor (). Weber et al reported the occurrence of orbital and subconjunctival emphysema after orbital floor fracture in a patient after blowing his nose, but without subcutaneous emphysema.Citation11 To the best of the author’s knowledge, this is the first reported case of simultaneous subcutaneous, subconjunctival, and orbital emphysema associated with orbital floor fracture. Because of the location of the orbital floor fracture, the initial air was more likely in the orbit, and with the subsequent sneezing and increased intraorbital pressure, direct spread occurred from the orbit into the subconjunctival and later into the subcutaneous planes, although the orbital septum usually forms a barrier between these potential spaces,Citation6 which might be torn by blunt trauma.
Elevated intraocular pressure is a concern in orbital more than subconjunctival emphysema. A prolonged increase in intraocular pressure can lead to optic nerve damage from ischemia similar to compartment syndromes in 1–2 hours if the intraocular pressure approaches ophthalmic artery perfusion pressure.Citation12 Previous reports have described increases in intraocular pressure to 28 mmHg.Citation8 In the current patient, the intraocular pressure increased to 26 mmHg and he was treated with topical timolol 0.5% twice daily, with return of the intraocular pressure to 13 mmHg with treatment and on resolution of the emphysema. Cartwright et alCitation4 also reported that an elevation in intraocular pressure after orbital trauma with orbital emphysema is usually not severe or long enough to result in visual compromise but requires continuous monitoring.
Most orbital emphysema requires no specific treatment, since the process is self-limiting, with an approximate duration of 2 weeks.Citation3,Citation13 Attention must be paid to prevent compressive optic neuropathy and exposure keratopathy. Although a good visual outcome is common, serious vision-threatening sequelae have been reported.Citation10 Increases in intraorbital pressure may cause damage to the blood supply of the optic nerve, leading to optic atrophy and poor visionCitation14 or central retinal artery occlusion.Citation15 The surgical treatment of orbital emphysema includes lateral canthotomy or cantholysis, orbital decompression by needle aspiration, and bone decompression.Citation11,Citation16,Citation17 Therefore, the presence of any type of periocular emphysema after blunt trauma should raise suspicion for orbital blowout fracture and mandates orbital computed tomography with careful follow-up of the patient.
Disclosure
The author reports no conflict of interest in this work.
References
- AggarwalECoglanPMadgeSNSelvaDBilateral subconjunctival emphysema as a complication of pneumothoraxClin Experiment Ophthalmol20113958158221176049
- JordanDRWhiteGLJrAndersonRLTheiseSMOrbital emphysema: a potentially blinding complication following orbital fracturesAnn Emerg Med1988178538553394993
- BalajiSMSubcutaneous emphysemaJournal of Maxillofacial and Oral Surgery Available from: http://link.springer.com/content/pdf/10.1007/s12663-010-0158-9#Accessed April 16, 2013
- CartwrightMJGinsburgRNNelsonCCTension pneumoorbitusOphthal Plast Reconstr Surg19928303304
- YukselMYukselKZOzdemirGUgurTBilateral orbital emphysema and pneumocephalus as a result of accidental compressed air exposureEmerg Radiol20071319519817115095
- SeiffSRJohnsonRNMorganCMSubconjunctival emphysema associated with mechanical ventilationArch Ophthalmol1985103127712783899063
- MathewSVasuUFrancisFNazarethCTransconjunctival orbital emphysema caused by compressed air injury: a case reportIndian J Ophthalmol20085624724918417833
- BigerYAbulafiaCSubconjunctival emphysema due to trauma by compressed air tubeBr J Ophthalmol1986702272283954982
- LiTMafeeMFEdwardDPBilateral orbital emphysema from compressed air injuryAm J Ophthalmol199912810310410482105
- CaesarRGajusMDaviesRCompressed air injury of the orbit in the absence of external traumaEye (Lond)20031766166212855983
- WeberDShawSWinslowJTraumatic eye swelling. Subconjunctival and orbital emphysema with orbital floor fractureAnn Emerg Med20095463519769893
- CarrimZIAndersonIWKylePMTraumatic orbital compartment syndrome: importance of prompt recognition and managementEur J Emerg Med20071417417617473616
- ReevesDLLucarelliMJRoseJGJrSevere subcutaneous emphysema following orbital blowout fractureOphthal Plast Reconstr Surg200521465467
- GrossJGDoxanasMTTraumatic optic atrophy caused by compressed airAnn Ophthalmol19871969703566027
- HuntsJHPatrinelyJRHoldsJBAndersonRLOrbital emphysema. Staging and acute managementOphthalmology19941019609668190488
- LeeSLMillsDMMeyerDRSilverSMOrbital emphysemaOphthalmology20061132113e1e217074576
- ChakGJosephJMTaoJPNeedle decompression of acute orbital emphysema: case report with videoBr J Ophthalmol2012961346134722914499