Abstract
Introduction
Hemorrhagic retinal macrocysts are extremely rare retinal lesions that can be mistaken for malignancy with subsequent enucleation. Such a case was diagnosed, by a retina specialist based on ultrasonography, as a choroidal melanoma with exudative retinal detachment and the patient was advised to have brachytherapy.
Case presentation
A 15-year-old Caucasian boy suffered sudden visual loss in the left eye and exam revealed vitreous hemorrhage. Magnetic resonance imaging revealed the mass as hyperintense on T1-weighted images and isointense on T2-weighted images with no enhancement after gadolinium dye. Following scleral buckle, the hemorrhagic retinal macrocyst collapsed gradually over a period of 5 weeks. The patient recovered visual acuity of 6/7.5 at the 1-year follow up.
Conclusion
A hemorrhagic retinal macrocyst can be erroneously diagnosed as choroidal melanoma. Hints for the presence of retinal macrocysts include: egg shape; cyst wall configuration; no attachment to the choroid; and presence of retinal detachment.
Introduction
Retinal macrocysts are large cysts commonly found after long-standing retinal detachmentCitation1–Citation7 and are clinically different from cysticercosis, retinal abscess, and medulloepithelioma. An unusual case of hemorrhagic retinal macrocyst, which was initially diagnosed as a malignant melanoma of the choroid, is presented.
Case presentation
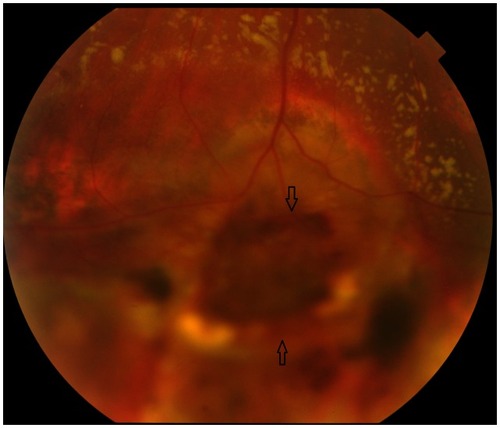
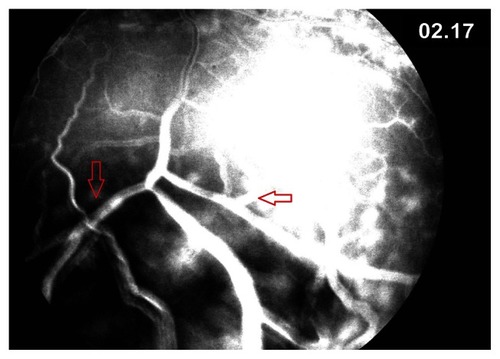
This 15-year-old Caucasian boy suffered sudden visual loss in the left eye and examination revealed vitreous hemorrhage. There was no history of ocular trauma or bleeding disorder. One month later he was referred to a fellowship trained retinal specialist for evaluation. Choroidal melanoma of the left eye was diagnosed based on ultrasound findings (). Brachytherapy was advised. Examination revealed best corrected visual acuity of 20/30, dark round well-delineated inferotemporal retinal mass (), inferotemporal dialysis, and shallow inferior retinal detachment. The clinical diagnosis was hemorrhagic retinal macrocyst. Repeat ultrasonography confirmed the smooth cystic contour to the mass. The macrocyst wall was continuous with the retina. The mass had low reflective internal contents without choroidal excavation ( and ). Intravenous fluorescein angiography revealed blockage of fluorescence by the mass (). There was autofluorescence of the center and edges of the retinal mass (). On magnetic resonance (MR) imaging, the mass appeared hyperintense on T1-weighted images and isointense on T2-weighted images. The mass disappeared gradually 5 weeks after scleral buckle with drainage of subretinal fluid (). Best corrected vision acuity improved to 6/7.5 at the 1-year follow up.
Figure 1 Ultrasound scan of the left eye.
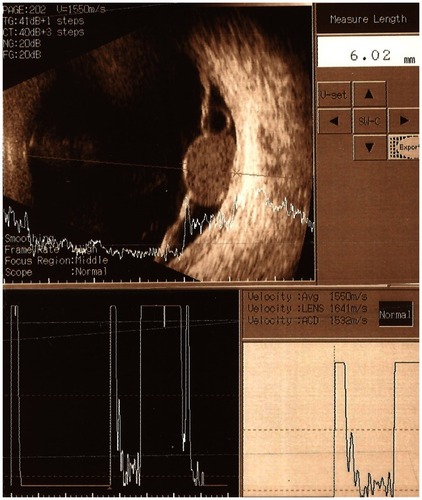
Figure 2 Fundus photograph of the left eye.
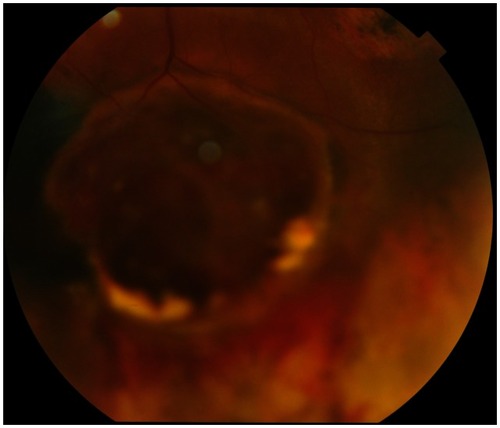
Figure 3 Repeat ultrasound scan of left eye (1 week later).
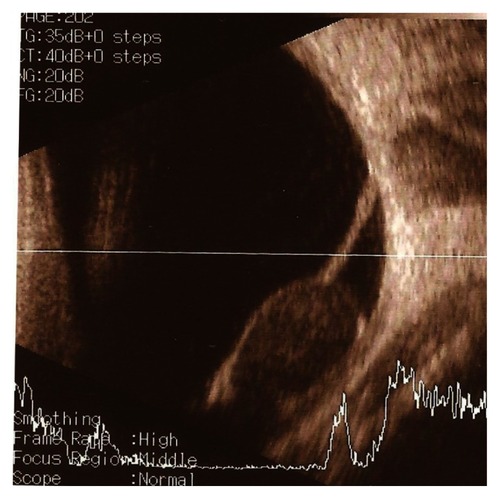
Figure 4 Late frame of fluorescein angiography.
Discussion
The differential of a peripheral retinal cystic lesion includes retinoschisis, cysticercosis, medulloepithelioma, toxocariasis, localized Coats disease, peripheral choroidal neovascularization, and intraocular choristoma. Retinal macrocysts are usually asymptomatic, single or multiple fluid-filled cavities that are associated with long-standing retinal detachment, particularly of the traumatic type with retinal dialysis.Citation7 They arise often from the outer plexiform layer of the retina and require no specific attention during retinal detachment repair.Citation4 Surgical collapse of the macrocyst is required only when the macrocyst prevents closure of the primary retinal break. Hemorrhagic macrocysts are rare. The presence of blood in the macrocyst cavity could stem from rupture of the retinal blood vessels lining the macrocyst,Citation4–Citation6 bridging retinal vessels over a retinal tear, or peripheral neovascularization.Citation8,Citation9
RuizCitation1 described the enucleation of a blind eye with a long history of retinal detachment. A choroidal melanoma was suspected by funduscopy. However by histopathology this eye contained a retinal macrocyst with organized blood. VogelCitation2 reported two cases also initially diagnosed as choroidal melanoma that were histologically hemorrhagic retinal cysts. WolterCitation3 found a blackish retinal mass during dissection of a blind eye that turned out also to be a blood-filled retinal macrocyst. Rishi et alCitation4 documented the collapse of a large hemorrhagic retinal macrocyst 3 years after a scleral buckle. The current case was a seeing eye, initially diagnosed as choroidal melanoma. Retinal macrocysts usually collapse spontaneously within weeks after successful retinal reattachment.Citation5,Citation6
Melanoma of the choroid appears hyperintense on T1-weighted image and hypointense on T2-weighted image.Citation10 Acute hemorrhagic macrocyst appears hypointense on T2 images. Subacute hemorrhagic macrocyst has heterogeneous signals on T1 and T2 images. Chronic hemorrhagic macrocyst appears hyperintense on both T1 and T2 images.Citation10 Hence MR signals are generally of little help to differentiate between melanoma and hemorrhagic retinal cyst except in chronic hemorrhagic cysts (). In the current case the cyst has similar MR features to that of a melanoma.
Table 1 Differentiating signs between choroidal melanoma and hemorrhagic retinal macrocyst
There is usually blockage of autofluorescent light by intraretinal blood in hemorrhagic retinal macrocyst. Choroidal melanoma displays variable degrees of autofluorescence depending on the state of the overlying retinal pigment epithelium, the presence of orange pigment, the size and the pigmentation of the tumor.Citation11 Shields et alCitation11 detected the following percentages in 51 consecutive patients with choroidal melanoma: hypo-autofluorescence (39%), isoautofluorescence (6%) and hyper-autofluorescence (55%) (). In the current case, there was autofluorescence of the center and edges of the macrocyst, a feature that cannot be used to differentiate it from a melanoma.
In conclusion a macrocyst of the retina filled with organized hemorrhage is one more example of a condition which can be erroneously diagnosed as choroidal melanoma even with current technological advances. Egg shape, cyst wall configuration, and associated rhegmatogenous retinal detachment are some hints for the correct diagnosis of hemorrhagic retinal macrocysts.
Acknowledgment
The authors have obtained written, informed consent from the patient for publication of this case report.
Disclosure
The authors declare no conflicts of interest.
References
- RuizRSHemorrhagic macrocyst of the retina. mistaken for malignant melanoma of the choroidArch Ophthalmol1970835885905442149
- VogelMHMakrozysten der netzhaut blut gefüllt. Ein beitrag zur differentialdiagnose des malignen melanoms der aderhautBlood-filled macrocysts of the retina. A contribution to the differential diagnosis of malignant melanoma of the choroidKlin Monbl Augenheilkd1975167855864 German1226023
- WolterJRBlood-filled macrocyst of the peripheral retinaSurv Ophthalmol196411813513814143472
- RishiPRishiESenPRSharmaTHemorrhagic intraretinal macrocyst: Differential diagnoses and report of an unusual caseOman J Ophthalmol20114283121713238
- GoelSDAugsburgerJJHemorrhagic retinal macrocysts in advanced Coats diseaseRetina1991114374401813964
- ConwayBPWelchRBX-chromosone-linked juvenile retinoschisis with hemorrhagic retinal cystAm J Ophthalmol197783853855868987
- MarcusDFAabergTMIntraretinal macrocysts in retinal detachmentArch Ophthalmol19799712731275454261
- VerdaguerPNadalJIntraretinal cyst secondary to longstanding retinal detachmentEur J Ophthalmol20122250650821928257
- LabriolaLTBrantAMEllerAWChronic retinal detachment with secondary retinal macrocyst and peripheral neovascularizationSemin Ophthalmol2009242419241283
- StroszczynskiCHostenNBornfeldNChoroidal hemangioma: MR findings and differentiation from uveal melanomaAm J Neuroradiol199819144114479763374
- ShieldsCLBianciottoCPirondiniCMaterinMAHarmonSAShieldsJAAutofluorescence of choroidal melanoma in 51 casesBr J Ophthalmol20089261762218441171