Abstract
Purpose
To report our experience of performing immediate sequential bilateral cataract surgery (ISBCS) in patients with visually significant cataracts and reduced preoperative corrected distance visual acuity (CDVA).
Methods
Data of patients who underwent ISBCS for visually significant cataracts and had preoperative CDVA ≤20/32 (≤0.2 logMAR) in each eye were retrospectively reviewed. Refractive and visual outcomes were evaluated for the last available postoperative visit. Intraoperative and serious postoperative adverse events occurring within the first three months of surgery were reviewed.
Results
A total of 1335 patients (2670 eyes) were included in the analysis, with a mean age of 71.9 ± 9.5 years. On the last visit, 50.2% and 89.1% of eyes achieved uncorrected distance visual acuity (UDVA) ≥20/20 (0.0 logMAR) and ≥20/32 (0.2 logMAR), respectively. Of all eyes, 83.8% were within ±0.50D, and 96.4% were within ±1.00 D of emmetropia. Ten patients had postoperative bilateral ametropia of more than 1.00D in each eye, but eight of them still achieved binocular UDVA ≥20/40. Intraoperative events occurred in 14 eyes of 13 patients (per-eye incidence: 0.524% or 1 in 191 eyes). A total of 86 postoperative adverse events occurred in 80 eyes of 53 patients (per-eye incidence 2.996% or 1 in 33 eyes), of which cystoid macular edema was the most common. Only three eyes had CDVA reduced by more than two Snellen lines compared to preoperative CDVA, two of which were not related to cataract surgery. There was no patient with bilateral CDVA loss.
Conclusion
In our cohort of patients with visually significant cataracts, ISBCS resulted in good refractive predictability and a low incidence of serious adverse events.
Introduction
Delayed sequential bilateral cataract surgery (DSBCS) has traditionally been considered to be the standard of care in the treatment of bilateral cataracts, with the primary reasons contributing to this decision being the potential risk of infection, blindness, and refractive surprise.Citation1,Citation2 However, there is growing evidence that same-day immediate sequential bilateral cataract surgery (ISBCS) is a safe alternative to DSBCS.Citation3 ISBCS affords the patient a more rapid and comfortable visual recovery, reduced symptoms caused by DSBCS of induced anisometropia, and a reduction in costs and wait times for surgery.Citation1,Citation2,Citation4 There is also a suggestion that same-day cataract surgery for both eyes has the potential to use financial, environmental, and human resources more effectively and also afford patients the opportunity to experience a faster return to binocular visual function.Citation5–7
The aim of this study is to report our experience of performing ISBCS in a large population of patients with visually significant cataracts with a reduced corrected distance visual acuity (CDVA) of 20/32 or less, focusing on the refractive predictability, visual outcomes, and adverse events rates.
Patients and Methods
This study was deemed exempt from review by the University of California, San Francisco Institutional Review Board because it used only retrospective, de-identified patient data. All patients provided full informed consent to undergo cataract surgery as well as to have their de-identified information used for statistical analysis and research purposes. The study adhered to the tenets of the Declaration of Helsinki.
The electronic medical record of Optical Express (Glasgow, United Kingdom) was searched to identify patients who underwent bilateral same-day surgery for visually significant cataracts (corrected distance visual acuity 20/32 or worse in each eye) between January 2019 and November 2022. Patients’ demographics, preoperative and postoperative clinical data, as well as intraoperative and serious postoperative adverse events occurring within the first three months of surgery were extracted from the electronic medical record. The main focus was on adverse events that manifest in the early postoperative period, have the potential to become sight-threatening and could potentially lead to bilateral reduction in visual acuity. Thus, the aim was to identify early adverse events that could have been diagnosed and managed had there been a delay between the first and the second eye. Late-onset postoperative events have not been evaluated because these have the same potential to affect patients bilaterally whether the patient has ISBCS or DSBCS.
The pros and cons of bilateral same-day vs delayed sequential surgery were discussed with the patients and they were given the opportunity to choose between the two approaches. Patients with hypermature cataracts or those with significant ocular co-morbidities that were more likely to lead to intraoperative or serious postoperative complications were not offered bilateral same-day surgery.
All patients underwent a full ophthalmic examination including but not limited to manifest refraction, visual acuity testing, anterior eye slit lamp examination, and dilated fundus examination. Diagnostic scans included autorefraction and tonometry (Tonoref II, Nidek Co. Ltd., Gamagory, Japan), corneal tomography (Pentacam, Oculus Optikgeräte GmbH, Wetzlar, Germany), endothelial cell count (SP 2000P specular microscope, Topcon Corp, Tokyo, Japan), biometry (IOLMaster 700, Carl Zeiss Meditec AG, Jena, Germany) and retinal optical coherence tomography (Cirrus 4000/5000 OCT, Carl Zeiss Meditec AG, Jena, Germany). Preoperative and postoperative visual acuity measurements included monocular corrected distance visual acuity (CDVA) and monocular and binocular uncorrected distance (UDVA) visual acuity.
Surgeries were performed with standard phacoemulsification, and the surgical procedure followed the recommendations of the “General Principles for Excellence in ISBCS”.Citation8 The surgeries were performed by 18 surgeons in 17 surgical centers across the United Kingdom. When deciding on the treatment sequence of the two eyes, the first treated eye was typically the worse eye according to the surgeon’s clinical judgment (eg, the eye with poorer corrected visual acuity or more advanced cataract). If the two eyes were similar, the non-dominant eye was treated first. Intracameral cefuroxime was used at the end of surgery as a prophylaxis for endophthalmitis (with the exception of patients with proven penicillin allergy, where moxifloxacin was used).
The standard postoperative regimen included 250mg acetazolamide tablet per oral taken 4–6 hours after discharge, topical broad-spectrum antibiotic drops (levofloxacin 5mg/mL) for 2 weeks (every two hours for the first 24 hours and then four times a day for the remaining 13 days), and topical steroid drops (dexamethasone 0.1%) for four weeks (every two hours for the first 24 hours, four times a day for 13 days and three times a day for further 14 days).
Statistical Analysis
The analysis of refractive and visual outcomes was based on the last available follow-up visit of each patient and included only patients that reached a minimum of one-month follow-up. The incidence of adverse events was calculated for all patients in the cohort (regardless of the follow-up length) and included intraoperative events and serious postoperative events that occurred within the first three months of surgery. The standards for reporting outcomes of lens-based surgery were used to present the clinical outcomes of the study group.Citation9 All calculations were performed in Microsoft Excel (Microsoft Corp.).
Results
The study included 1335 patients (2670 eyes), of whom 1192 patients (89.3%) reached a minimum of one-month postoperative visit. The mean age of the study group was 71.9 ± 9.5 years (median 73 years, range 34 to 96 years). Of all patients, 758 (56.8%) were male and 577 (43.2%) were female.
The mean axial length of the study group was 23.82 ± 1.34 mm (median 23.68 mm, range 19.85 to 29.75 mm). Of all eyes, 182 (6.8%) had an axial length shorter than 22.00 mm, 2308 eyes (86.4%) had an axial length between 22.00 and 26.00 mm and the remaining 180 eyes (6.7%) had an axial length longer than 26.00 mm. Most of the eyes (99.7% or 2662 eyes) had a monofocal lens implant, while only 8 eyes (4 patients, 0.3%) had an extended depth of focus or a low near addition multifocal IOL. A non-toric IOL was used in 2162 eyes (81.0%), and a toric IOL was used in 508 eyes (19.0%). Demographics of the study group, preoperative and postoperative clinical outcomes are summarized in .
Table 1 Preoperative and Postoperative Clinical Data of the Study Group
Visual and Refractive Outcomes
Visual and refractive outcomes were calculated for a group of patients who reached at least one-month follow-up visit. The mean follow-up of this group of patients was 3.3 ± 3.4 months (range 1 to 15 months). depicts standard graphs for reporting outcomes of lens-based surgery in the cataract population. Of all eyes, 50.2% (1196/2384) and 89.1% (2123/2384) achieved postoperative monocular UDVA 20/20 and 20/32 or better, respectively (). Binocularly, UDVA of 20/20 and 20/32 or better was achieved in 72.7% (866/1192) and 96.6% (1152/1192) of patients, respectively.
Figure 1 Refractive and visual outcomes of patients with a minimum of one-month postoperative visit. Outcomes are based on the last available follow-up visit (mean follow-up 3.3 ± 3.4 months). (A) Cumulative postoperative monocular uncorrected (UDVA) and corrected (CDVA) distance visual acuity; (B) A histogram of the difference between postoperative UDVA and postoperative CDVA; (C) The distribution of postoperative manifest spherical equivalent (MSE). (D) The distribution of preoperative and postoperative refractive astigmatism.
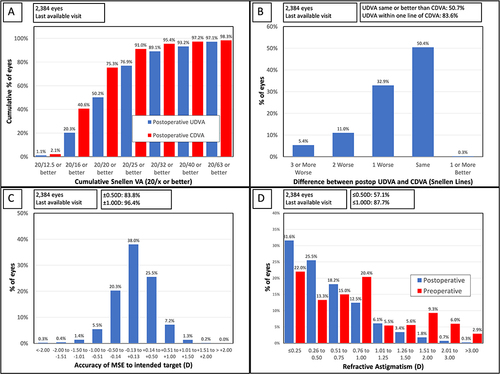
Of all eyes, 83.6% (1992/2384) had their postoperative monocular UDVA within one Snellen line of their postoperative CDVA (). The mean CDVA changed from a preoperative value of 0.48 ± 0.41 logMAR (≈20/60) to 0.02 ± 0.15 logMAR (≈20/20−2).
depicts the distribution of postoperative manifest spherical equivalent. Of all eyes, 83.8% (1998/2384) were within ±0.50D, while 96.4% (2299/2384) were within ±1.00 D of emmetropia. The mean postoperative manifest spherical equivalent of the study group was +0.02 ± 0.47 D. Of the eyes that reached one month follow-up, eyes with a toric IOL had a slightly lower percentage of eyes within ±0.50 D of emmetropia: 84.5% (1624/1922) of eyes with a non-toric IOL and 81.0% (374/462) of eyes with a toric IOL were within ±0.50D of emmetropia, but the difference did not reach statistical significance (p = 0.06). However, eyes with toric and non-toric IOLs had a very comparable percentage of eyes within ±1.00 D of emmetropia: 96.4% (1853/1922) of non-toric IOL eyes and 96.5% (446/462) of toric IOL eyes were within ±1.00 D of emmetropia; p = 0.90.
shows the distribution of preoperative and postoperative refractive cylinder. Postoperatively, 57.1% (1361/2384) of eyes had refractive cylinder ≤0.50D, while 87.7% (2091/2384) of eyes had refractive cylinder ≤1.00D.
Postoperative Bilateral Ametropia
Ten patients (0.84% or 10/1192) had postoperative bilateral ametropia of more than 1.00 D in each eye. No patients had postoperative bilateral ametropia of more than 1.50 D in each eye. Eight out of 10 patients with postoperative bilateral ametropia still achieved postoperative binocular UDVA of 20/40 or better. Of the ten patients with bilateral refractive surprise, two subsequently elected to undergo laser vision correction for treatment of the ametropia.
Adverse Events
shows the summary of all intraoperative and postoperative adverse events recorded within the first 3 months.
Table 2 Intraoperative and Postoperative Adverse Events
Intraoperative Adverse Events
Intraoperative events occurred in 14 eyes of 13 patients (per-eye incidence: 0.524% or 1 in 191 eyes, per-patient incidence 0.974% or 1 in 103 patients). Posterior capsule (PC) tear occurred in 5 eyes (per eye incidence; 0.187% or 1 in 534 eyes; per patient incidence 0.375% or 1 in 267 patients). Of the 5 eyes with PC tears, 2 needed a vitrectomy, and 1 eye was already vitrectomised following previous retinal detachment surgery. At the last postoperative appointment, 3 eyes had UDVA of 20/20, 1 had a UDVA of 20/25 corrected to 20/20, and 1 eye had a UDVA and CDVA of 20/25.
There was one eye with a dropped nucleus that underwent a vitrectomy, lensectomy, and anterior chamber-fixated implant with the final postoperative UDVA and CDVA of 20/25 compared to the pre-operative CDVA of 20/100.
Other intraocular events (occurring in one eye each) were zonule dialysis, zonule rupture, and surgical equipment failure. Torn iris was recorded in 5 eyes of 4 patients, and it was the only intraoperative AE that was recorded bilaterally in one patient.
Postoperative Adverse Events
A total of 86 postoperative adverse events occurred in 80 eyes of 53 patients (per-eye incidence 2.996% or 1 in 33 eyes, per-patient incidence 3.970% or 1 in 25 patients). No patient developed endophthalmitis.
Most of the postoperative events were those expected after cataract surgery, with cystoid macular edema and corneal edema having the highest occurrence ().
Loss of More Than Two Lines of Corrected Distance Vision
Of all patients who attended a minimum of one month follow-up, only three eyes had CDVA reduced by more than two Snellen lines compared to preoperative CDVA. The reasons for CDVA loss were as follows: case 1 – worsening of pre-existing age-related macular degeneration, case 2 – displaced IOL postoperatively, requiring intervention, case 3 – development of central retinal artery occlusion. All three cases were unilateral and had the UDVA 20/25 or better in the fellow eye at the last available visit.
Discussion
The aim of this study was to report adverse events rates, as well as refractive and visual outcomes in a cohort of ISBCS cataract patients with preoperative reduced CDVA of 20/32 or less. Historically, concerns in offering same-day surgery to cataract patients revolved around safety, visual outcomes, and refractive surprise post-treatment, with the delayed approach allowing for adjustments to the IOL power on the second eye.Citation10,Citation11
In the literature reports, safety concerns have largely been mitigated by the dramatic reduction in endophthalmitis rates with the adoption of intracameral antibioticsCitation12–14 and with adherence to the ISBCS General Principles for Excellence.Citation8 The remaining outstanding major criticism of ISBCS has been the refractive accuracy.Citation15,Citation16
While this study included cataract patients with CDVA worse than 20/32, our results demonstrate that 89.1% of patients achieved UDVA of 20/32 or better monocularly, improving to 96.6% achieving at least 20/32 UDVA binocularly. Of all eyes, 83.6% had their postoperative monocular UDVA within one Snellen line of their postoperative CDVA.
Refractive predictability was good, with 83.8% of all eyes within ±0.50D, while 96.4% were within ±1.00 D of emmetropia. The mean postoperative manifest spherical equivalent of the study group was +0.02 ± 0.47 D. Only 0.84% (n=10) of patients had postoperative bilateral ametropia of more than 1.00 D in each eye, with eight out of 10 patients with postoperative bilateral ametropia still achieving postoperative binocular UDVA of 20/40 or better. This is within the expected outcomes of surgery utilizing modern biometry and formulas performed with DSBCS.Citation17
A study utilizing the Intelligent Research in Sight (IRIS) database in the United States found that patients undergoing ISBCS had, on average, a slight reduction in postoperative UDVA and CDVA compared to DSBCS patients.Citation16 These study results are likely not generalizable to the wider population as the adoption of ISBCS in the US has been hampered by reimbursement issues, and many practitioners confine the use of ISBCS to medically complex cases.Citation18 In contrast, a study of ISBCS versus DSBCS in the Kaiser population in the US found no difference in refractive outcomes.Citation19
These risks, whether substantiated or not, must be weighed against the risks of delayed surgery. This includes the risk of induced anisometropia and worsened stereopsis leading to the risk of falls following first eye surgery, especially in the elderly population. In a study by Keay et al,Citation20 the risk of injurious falls halved after the second eye surgery in a population of ≥65 years old patients with bilateral visually significant cataracts. The authors concluded that first eye surgery substantially improved vision in older patients with cataracts, but second eye surgery is required to minimize fall incidence. In a large population of almost 30,000 elderly patients, Meuleners et alCitation21 found that the risk of injurious falls requiring hospitalization was the highest between first and second eye surgery, with the greatest risk being within the first five months after the first eye surgery.
Other studies also reported numerous benefits after the second eye surgery, such as improved stereopsisCitation22,Citation23 or better patient-reported outcomes.Citation22,Citation24 Additionally, Lundstorm et alCitation24 evaluated the reasons why some patients reported more difficulties following cataract surgery and found that approximately a third of the cases reporting “no benefit” of cataract surgery were those who had anisometropia and problems with the non-operated eye following the first eye surgery. Another commonly discussed aspect is the effect of time delay of cataract surgery on mental health. A population-based study found that shortening the time interval between the first and second eye operation had a positive impact on mental health and was significantly correlated with the reduced number of mental health consultations.Citation25
Our study reports relatively low incidence of adverse events; however, the population was not large enough to establish the rates of some rare adverse events, such as endophthalmitis. The per-eye intra-operative adverse event rate was 0.524%, and the postoperative per-eye incidence was 2.996%. This is in line with prior studies of ISBCS, with the exception of a reduced posterior capsular rupture rate in our study.Citation5,Citation19,Citation26 Postoperative events in our study population were those that are expected following cataract surgery in this particular age group. Although we have not performed a direct comparison to a DSBCS group, various studies reported the intra-operative and post-operative complication rates being similar when comparing ISBCS to DSBCS.Citation19,Citation27,Citation28
Only 3 eyes had a CDVA reduced by more than two Snellen lines compared to preoperative CDVA. Two of these were not related to the cataract surgery (pre-existing age-related macular degeneration and development of central retinal artery occlusion). However, the loss of CDVA in 1 eye was attributed to a displaced IOL post-operatively that required surgical intervention. More important, there was no bilateral vision loss of more than two Snellen lines.
Recognizing that the occurrence of endophthalmitis has historically remained a barrier to many surgeons adopting an ISBCS approach, in this study, there was no occurrence of endophthalmitis. However, a larger study group may be needed to reveal the true rate of this sight-threatening complication in cataract patients with reduced CDVA undergoing ISBCS. Although there have been sporadic reports of bilateral endophthalmitis following ISBCS, most of them were related to inappropriate aseptic techniques.Citation29,Citation30 To date, there have been very few cases of bilateral endophthalmitis in ISBCS patients where all surgical recommendations have been followed,Citation29 making the calculation of the true incidence rate difficult.
Some study limitations need to be acknowledged. The retrospective design of the study has its inherent limitations and provides a lower level of evidence compared to prospective studies. A comparison to a control group of patients with delayed sequential surgery would be beneficial, especially for the comparison of bilateral ametropia rates. However, most patients who undergo DSBCS in our clinical practice are those who are unsuitable for immediate sequential surgery, and their preoperative characteristics are not comparable to ISBCS patients. The sample was relatively homogenous in terms of IOL selection, as most of the patients had monofocal IOLs. This is due to the fact that monofocal IOLs are often the main choice in patients with poorer preoperative corrected visual acuity in our practice. Assessing the refractive accuracy of ISBCS in patients with premium IOLs would be beneficial, but this has already been addressed in our previous study in a population of refractive lens exchange patients.Citation3
A small proportion of patients included in the adverse event count did not reach 1-month postoperative visit, and this could be a potential limitation of this study. However, these patients were mostly those who achieved very good outcomes in the early postoperative period and did not want to return for further follow-ups. Quite often (mainly during the Covid-19 pandemic), these patients were followed with a telemedicine consultation (a phone call), questioned about changes in their visual acuity and symptoms, and were advised to return to the clinic when experiencing any problems. However, a larger study population is needed to yield the true rate of endophthalmitis.
Conclusions
In a relatively large cohort of patients with visually significant cataracts, we have not observed any complications that would lead to bilateral vision loss. We believe the growing literature evidence of ISBCS safety will add to the acceptance of this approach among surgeons and increase the efficiency of cataract surgery.
Disclosure
Dasi Raju, Stephen Hannan, Mirna Belovari, Noelle Hannan, Colin Berry, Jan Venter, and David Teenan are employees of Optical Express. Steven Schallhorn is a chief medical officer for Carl Zeiss Meditec and a chairman of medical advisory board for Optical Express. Julie Schallhorn received personal fees from Carl Zeiss Meditec, Allergan, ViaLase, Long Bridge, and Forsight V6 and has a financial interest in Journey 1, Neurotrigger, and Novus Vision. The authors report no other conflicts of interest in this work.
References
- Amsden LB, Shorstein NH, Fevrier H, Liu L, Carolan J, Herrinton LJ. Immediate sequential bilateral cataract surgery: surgeon preferences and concerns. Can J Ophthalmol. 2018;53(4):337–341. doi:10.1016/j.jcjo.2017.10.034
- Singh R, Dohlman TH, Sun G. Immediately sequential bilateral cataract surgery: advantages and disadvantages. Curr Opin Ophthalmol. 2017;28(1):81–86. doi:10.1097/ICU.0000000000000327
- Hannan SJ, Schallhorn SC, Venter JA, Teenan D, Schallhorn JM. Immediate sequential bilateral surgery in refractive lens exchange patients: clinical outcomes and adverse events. Ophthalmology. 2023;130(9):924–936. doi:10.1016/j.ophtha.2023.04.013
- Mills EC, Zarei-Ghanavati M, Liu CSC. Immediate sequential bilateral cataract surgery: the rationale, implementation, and beliefs of ophthalmic surgeons across Europe. J Cataract Refract Surg. 2019;45(12):1725–1731. doi:10.1016/j.jcrs.2019.07.027
- Buchan JC, Donachie PHJ, Cassels-Brown A, et al. The royal college of ophthalmologists’ national ophthalmology database study of cataract surgery: report 7, immediate sequential bilateral cataract surgery in the UK: current practice and patient selection. Eye. 2020. doi:10.1038/s41433-019-0761-z
- Arshinoff SA. Same-day cataract surgery should be the standard of care for patients with bilateral visually significant cataract. Surv Ophthalmol. 2012;57(6):574–579. doi:10.1016/j.survophthal.2012.05.002
- Arshinoff SA, Odorcic S. Same-day sequential cataract surgery. Curr Opin Ophthalmol. 2009;20(1):3–12. doi:10.1097/ICU.0b013e32831b6daf
- Arshinoff SA, Claoue C, Johansson B iSBCS general principles for excellence in ISBCS 2009. Available from: https://itgo.ca/eyefoundationcanada/wp-content/uploads/sites/5/2020/05/2010-09-01-FINAL-ISBCS-SBCS-suggestions-from-ESCRS-Barcelona.pdf. Accessed December 2, 2022.
- Reinstein DZ, Archer TJ, Srinivasan S, et al. Standard for reporting refractive outcomes of intraocular lens-based refractive surgery. J Cataract Refract Surg. 2017;43(4):435–439. doi:10.1016/j.jcrs.2017.04.005
- Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL. First eye prediction error improves second eye refractive outcome results in 2129 patients after bilateral sequential cataract surgery. Ophthalmology. 2011;118(9):1701–1709. doi:10.1016/j.ophtha.2011.05.010
- Covert DJ, Henry CR, Koenig SB. Intraocular lens power selection in the second eye of patients undergoing bilateral, sequential cataract extraction. Ophthalmology. 2010;117(1):49–54. doi:10.1016/j.ophtha.2009.06.020
- ESCRS Endophthalmitis Study Group. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007;33(6):978–988. doi:10.1016/j.jcrs.2007.02.032
- Haripriya A, Chang DF, Ravindran RD. Endophthalmitis reduction with intracameral moxifloxacin prophylaxis: analysis of 600 000 Surgeries. Ophthalmology. 2017;124(6):768–775. doi:10.1016/j.ophtha.2017.01.026
- Kato A, Horita N, Namkoong H, et al. Prophylactic antibiotics for postcataract surgery endophthalmitis: a systematic review and network meta-analysis of 6.8 million eyes. Sci Rep. 2022;12(1):17416. doi:10.1038/s41598-022-21423-w
- Olsen T. Use of fellow eye data in the calculation of intraocular lens power for the second eye. Ophthalmology. 2011;118(9):1710–1715. doi:10.1016/j.ophtha.2011.04.030
- Owen JP, Blazes M, Lacy M, et al. Refractive outcomes after immediate sequential vs delayed sequential bilateral cataract surgery. JAMA Ophthalmol. 2021;139(8):876–885. doi:10.1001/jamaophthalmol.2021.2032
- Melles RB, Holladay JT, Chang WJ. Accuracy of Intraocular Lens Calculation Formulas. Ophthalmology. 2018;125(2):169–178. doi:10.1016/j.ophtha.2017.08.027
- Neel ST. A cost and policy analysis comparing immediate sequential cataract surgery and delayed sequential cataract surgery from the physician perspective in the United States. JAMA Ophthalmol. 2014;132(11):1359–1362. doi:10.1001/jamaophthalmol.2014.3335
- Herrinton LJ, Liu L, Alexeeff S, Carolan J, Shorstein NH. Immediate sequential vs. Delayed sequential bilateral cataract surgery: retrospective comparison of postoperative visual outcomes. Ophthalmology. 2017;124(8):1126–1135. doi:10.1016/j.ophtha.2017.03.034
- Keay L, Ho KC, Rogers K, et al. The incidence of falls after first and second eye cataract surgery: a longitudinal cohort study. Med J Aust. 2022;217(2):94–99. doi:10.5694/mja2.51611
- Meuleners LB, Fraser ML, Ng J, Morlet N. The impact of first- and second-eye cataract surgery on injurious falls that require hospitalisation: a whole-population study. Age Ageing. 2014;43(3):341–346. doi:10.1093/ageing/aft177
- Castells X, Comas M, Alonso J, et al. In a randomized controlled trial, cataract surgery in both eyes increased benefits compared to surgery in one eye only. J Clin Epidemiol. 2006;59(2):201–207. doi:10.1016/j.jclinepi.2005.06.007
- Comas M, Castells X, Acosta ER, Tuni J. Impact of differences between eyes on binocular measures of vision in patients with cataracts. Eye. 2007;21(6):702–707. doi:10.1038/sj.eye.6702305
- Lundstrom M, Brege KG, Floren I, Stenevi U, Thorburn W. Impaired visual function after cataract surgery assessed using the Catquest questionnaire. J Cataract Refract Surg. 2000;26(1):101–108. doi:10.1016/s0886-3350(99)00324-7
- Hou CH, Chen KJ, Lee JS, Lin KK, Pu C. Effect of the time interval between cataract surgery for both eyes on mental health outcome: a cohort study of 585,422 patients. BMC Ophthalmol. 2021;21(1):110. doi:10.1186/s12886-021-01876-9
- Sharma TK, Worstmann T. Simultaneous bilateral cataract extraction. J Cataract Refract Surg. 2001;27(5):741–744. doi:10.1016/s0886-3350(00)00741-0
- Ramsay AL, Diaper CJ, Saba SN, Beirouty ZA, Fawzi HH. Simultaneous bilateral cataract extraction. J Cataract Refract Surg. 1999;25(6):753–762. doi:10.1016/s0886-3350(99)00035-8
- Arshinoff SA, Strube YN, Yagev R. Simultaneous bilateral cataract surgery. J Cataract Refract Surg. 2003;29(7):1281–1291. doi:10.1016/s0886-3350(03)00052-x
- Chen MY, Qi SR, Arshinoff SA. Bilateral simultaneous postoperative endophthalmitis: review of cases reported over the past 50 years. J Cataract Refract Surg. 2022;48(7):850–854. doi:10.1097/j.jcrs.0000000000000875
- Kogawa S, Suzuki Y, Furukawa A, Kurosaka N, Nozuki N, Ueno S. Bilateral simultaneous endophthalmitis after immediately sequential bilateral cataract surgery. Am J Ophthalmol Case Rep. 2023;32:101886. doi:10.1016/j.ajoc.2023.101886
