Abstract
Objective
This study sought to evaluate the result of pars plana vitrectomy in patients with gunshot wounds involving double perforation.
Methods
This was a retrospective, noncomparative, interventional case series.
Results
Eighteen patients (18 eyes) with double-perforation gunshot injuries were treated from February 2010 to March 2012. The group included 16 men (88%) and two women (11%); the mean age was 24 (15–33) years. In each case, vitrectomy was scheduled 1–6 weeks after repair of the entrance site. Associated retinal detachments were observed in two eyes (11%), retinal incarceration was observed surrounding the exit site in three eyes (16%), and retention of an intraocular foreign body was observed in two cases. After a follow-up period of 8 ± 2 months, two eyes (11%) had achieved visual acuity (VA) of 0.5, nine eyes (50%) had achieved VA between 0.5 and 0.1, and seven eyes (38%) had achieved VA between 0.1 and hand movement. The main reasons for functional failure (VA 0.1 to hand movement) were macular dragging (due to fibrosis at the exit site near the macula) in seven cases (38%), submacular hemorrhage in four cases (22%), and epimacular fibrosis in five cases (27%). All cases developed postoperative exotropia. One case (5%) developed postoperative hemorrhage. No cases exhibited signs of postoperative redetachment.
Conclusion
The outcome of pars plana vitrectomy in cases with double perforations is variable. Factors including the surgeon’s skill level, the time to surgery, and the efficacy of the intraocular tamponade affect the postoperative outcome.
Introduction
The revolution that began on January 25, 2011 in Egypt has resulted in an increased number of gunshot wounds. The associated ocular injuries include retained intraocular foreign bodies (IOFBs) and double-perforation injuries. The standard approach to treating double-perforation injuries is primary repair to restore the structural integrity of the globe at the earliest opportunity.Citation1 If an intraocular or intraorbital foreign body exists, the retina should be examined carefully. If there is any damage, the physician must determine whether surgical intervention will be necessary. The visual prognosis in these cases depends on the degree of injury, and has improved since the advancement and refinement of vitreous microsurgical techniques.Citation2–Citation12 The present study aimed to evaluate the visual outcome in patients who had undergone pars plana vitrectomy after double-perforation gunshot injury.
Materials and methods
This retrospective, noncomparative, interventional case series included 18 patients (18 eyes) with double-perforation gunshot injuries treated by vitrectomy. Each was operated on using an injection of silicone oil 5000, from February 2010 to March 2012.
The exclusion criteria were corneal entry, central exit (optic disk or foveal) and/or visual acuity (VA) of less than light perception. All patients were fully informed of all aspects of the procedure, and all provided written informed consent. Ethics committee approval was obtained.
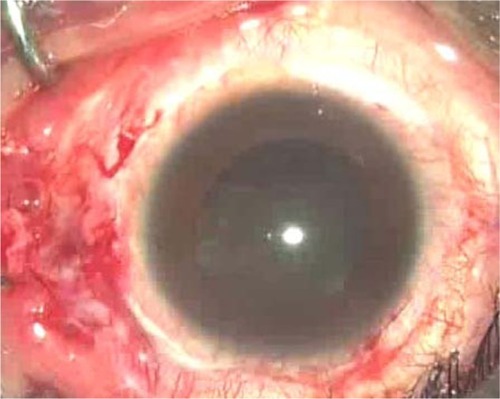
In each case, the preoperative examination included VA measurements and examination of the anterior segment to identify the entry site, to assess corneal clarity and evaluate any lens injury. In each case, the presence of vitreous hemorrhage precluded the use of fundus photography. B-scan ultrasonography was performed in all cases to locate the exit site, to detect the presence or absence of a retinal detachment or suprachoroidal hematoma and to localize any associated IOFB.
We obtained radiographs and computed tomography (CT) scans of the orbit. Conventional 20-gauge vitrectomy was performed. Before opening the infusion cannula, the entry site was examined to detect any leakage. In four cases, phacoemulsification and intraocular lens (IOL) implantation due to blood staining of the posterior capsule was done at the same time as the vitrectomy.
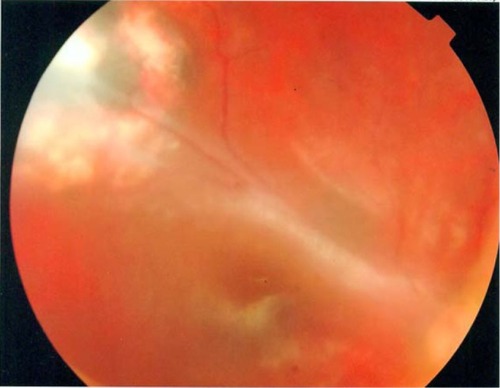
In all cases, the vitrectomy sought to remove vitreous that had coalesced around the sclerotomy site. This approach was designed to prevent retinal traction and rapid movement. During the procedure, the peripheral vitreous was shaved closely, in order to detect any peripheral breaks (either related to the sclerotomy or preexisting) to trim the vitreous surrounding the exit site and to release any retinal tissue that had coalesced around the exit site. Any hematoma proximal to the exit site was removed with caution, so as not to block the exit site. In some cases, only partial removal was possible.
An endolaser (diode laser) was applied to the area surrounding the exit site and any associated retinal tears. The data collected perioperatively included entrance-site patency, lens clarity, location of the exit site, the presence of an associated IOFB, and the presence of any associated damage, such as a retinal detachment or submacular hemorrhage.
The patients were examined 1 day, 1 week, 1 month, 2 months, 4 months, and 8 months after the surgery. The postoperative examination included VA assessment using logarithm of minimum angle of resolution units and intraocular pressure (IOP) measurements. Any associated complications were recorded.
Results
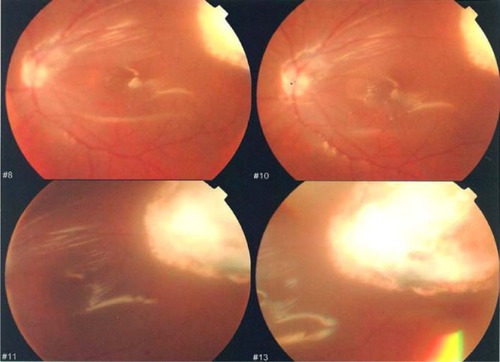
In total, 18 patients (18 eyes) with double-perforation gunshot injuries were treated. Five patients had bilateral involvement. The surgery was performed after repair of the primary scleral wound. This was <1 week in one patient (5%), 2–3 weeks after the primary repair in 13 patients (73%), and 3–6 weeks after the primary repair in four patients (22%) ().
Table 1 Age and sex distribution of the patient population and time to surgery after primary repair
Intraoperative results
Entrance-site closure
The scleral wound was well closed in 17 eyes. Leakage was observed in only one case that had been operated upon 1 week after the repair. Eleven patients (61%) exhibited temporal entry, and seven patients (38%) exhibited nasal entry ().
Lens clarity
The lens was clear in 14 cases (77%), while the other four cases (22%) exhibited blood staining of the posterior capsule. These cases were treated with phacoemulsification and IOL implantation at the time of surgery.
Exit site
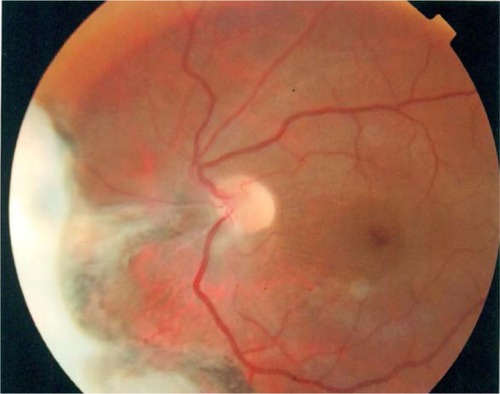
Exit sites were nasal in one case (5%) (), and between the temporal arcades in three cases (16%). Postoperative macular dragging developed in this latter group (); the exit site was in the inferior periphery in four cases (22%), and in the temporal periphery in ten cases (55%) ().
In the case operated upon after 1 week, the exit site had not healed completely. Leakage was observed at the site during the air–fluid exchange. The presence of an associated IOFB was observed in two cases (11%). Two cases exhibited retinal detachment (11%), retinal tissue abnormalities were observed at the exit site in three cases (16%), and submacular hemorrhage was observed in four cases (22%) ().
Table 2 Intraoperative results
In all phakic patients, silicone oil removal and cataract removal were performed simultaneously 3–6 months after the vitrectomy. The postoperative follow-up period was 8 ± 2 months from the date of this dual procedure. Two eyes (11%) achieved best-corrected visual acuity (BCVA) of 0.5, nine eyes (50%) achieved BCVA of 0.5–0.1, and seven eyes (38%) achieved BCVA between 0.1 and hand movement (HM).
The first two patients described had nasal and inferior peripheral exit sites. Eyes with BCVA between 0.1 and HM exhibited intraoperative submacular hemorrhage and postoperative macular dragging, due to contraction around the exit site. The average postoperative IOP was 19 mmHg ().
Table 3 Postoperative results
The main reasons for functional failure (VA 0.1–HM) were macular dragging (due to fibrosis at the exit site) in seven cases (38%), submacular hemorrhage in four cases (22%), and epimacular fibrosis in five cases (27%) (). All cases developed postoperative exotropia; one case (0.05%) developed postoperative hemorrhage after removal of the silicone oil. No instance of retinal detachment was reported postoperatively.
Table 4 Causes of functional failure
Discussion
The incidence of open-globe injury is about 3.6 to 3.8 per 100,000 around the world.Citation13–Citation15 According to the Birmingham Eye Trauma Terminology system, open-globe injury can be classified as laceration or rupture injuries; among laceration injuries, those in which a single foreign body has created the entrance and exit sites are considered a double-penetrating globe. If the entrance wound is not associated with an exit, the injury is defined as a penetrating injury.Citation16
The incidence of this type of injury peaks among young adults and elderly individuals aged >70 years. Open-globe injuries are much more common among men. This may reflect the more aggressive characteristics of male behavior.Citation14 In the current study, the mean age was 24 (15–33) years; there were 16 men (88%) and two women (11%).
Perforations often occur at the weak points of the globe, such as the limbus and insertion area of the extraocular muscle, and most perforations (70%) are located anterior to the ora serrata.Citation17 Endophthalmitis occurs in 2%–7% of patients with penetrating injuries. The incidence increases to 7%–31% if the IOFB remains in the eye.Citation17
Experimental and clinical studies suggest that among all types of globe wounds, double-perforating injuries have the worst prognosis.Citation18–Citation20 Shotgun injuries affecting both sides are also associated with poor visual prognosis. The factors limiting complete or near-complete visual recovery include direct injury to the optic nerve or macula, intraocular scarring and fibrosis with secondary retinal detachment, and severe ocular disorganisation.Citation21,Citation22
There are several predictive factors relative to the prognosis for final VA. These include poor presenting BCVA, the presence of a relative afferent pupillary defect, old age, blunt injury with eyeball rupture, a posterior injury site, lid laceration, lens damage, vitreous hemorrhage, and the presence of an IOFB.Citation23,Citation24 In all cases, a prompt preoperative evaluation and meticulous vitrectomy will increase the likelihood of a good anatomical and visual outcome.
Among the patients profiled here, the main reasons for functional failure (VA 0.1–HM) were macular dragging (due to fibrosis at the exit site near the macula) in seven cases (38%), submacular hemorrhage in four cases (22%), and epimacular fibrosis in five cases (27%).
The standard practice for open-globe injury is to undertake primary surgical repair to restore the structural integrity of the globe, to resolve any hypotonia and to recreate the barrier against infection at the earliest opportunity. Only when the injury is beyond primary repair is enucleation considered. In the case of a double-penetrating injury, the posterior exit wound is often left to heal spontaneously without surgical intervention. Experimental animal studies have shown that scleral wounds are closed with fibrosis by day 7 after injury.
Plain radiography, ultrasonography examination, and orbital scan
CT scans can provide enough information to locate an IOFB, to identify any choroidal hemorrhage, and to evaluate ocular integrity. In the current study, all cases underwent vitrectomy 1–6 weeks after entrance-site repair. The surgery was performed <1 week after repair of the primary scleral wound in one patient (5%), within 2–3 weeks after the primary repair in 13 patients (73%), and 3–6 weeks after the primary repair in four patients (22%).
The ideal timing of vitrectomy in ocular trauma is still controversial, but early vitrectomy is crucial in the presence of associated retinal detachment and/or endophthalmitis. In the animal model developed by Cleary and Ryan, intraocular blood triggered posterior vitreous detachment 1 week after an artificial penetrating injury. Cell proliferation on the retinal surface and vitreous induced tractional retinal detachment 6 weeks later. On the basis of these results, the authors advised that vitrectomy should be performed <14 days after the injury.Citation25
For perforating injuries with involvement of the posterior segment, several vitreoretinal surgeons have reported that the vitrectomy should be performed within 2 weeks. Coleman preferred early surgery within 72 hours in order to reduce inflammation by removing any inciting agents in an expedient fashion.Citation11 Ryan and Allen believed the optimum time for vitrectomy to be 4–10 days after the original injury in cases with IOFB.Citation26 Winthrop et al reported histological findings for 34 eyes that had severe penetrating trauma; 32 of 34 eyes had retinal detachments. The authors concluded that vitrectomy should not be delayed beyond the second week of injury, by which time massive cellular ingrowth may already be under way.Citation27
With regard to the use of silicone oil for most vitrectomies, the superiority of silicone oil over SF6 in cases of retinal detachment with proliferative vitreoretinopathy has previously been established.Citation28 An overall reattachment rate of 78.18% and functional success of 56.36% has been reported, while those that had proliferative vitreoretinopathy and underwent silicone oil implantation had a reattachment rate of 63.64%.Citation29 Other investigators reported total reattachment caused by trauma in silicone oil-filled eyes in 52%–62% of cases.Citation30 In the current study, silicone oil 5000 was used in all cases to prevent rebleeding from the exit wound.
In a similar case report on a patient with double-perforation gunshot injury with a scleral entrance and a nasal exit, the patient’s BCVA recovered to 6/12 1 week postoperatively, and 6/8.6 at 20-month follow-up.Citation31 In the current study, two eyes (11%) achieved BCVA of 0.5, nine eyes (50%) achieved BCVA of 0.5–0.1, and seven eyes (38%) achieved BCVA of 0.1–HM.
In conclusion, the outcome of vitrectomy with silicone oil tamponade in cases of double-perforation gunshot injury depends on various factors performed <2 weeks after the primary repair. A meticulous vitrectomy with peripheral shaving to release any retinal traction at the exit site should be performed using a silicone oil tamponade.
Disclosure
The author reports no conflicts of interest in this work.
References
- RahmanIMainoADevadasonDLeatherbarrowBOpen globe injuries: factors predictive of poor outcomeEye (Lond)2006201336134116179934
- ColesWHHaikGMVitrectomy in intraocular trauma. Its rationale and its indications and limitationsArch Ophthalmol1972876216285032732
- HuttonWLSnyderWBVaiserAVitrectomy in treatment of ocular perforating injuriesAm J Ophthalmol197681733779937426
- ClearyPERyanSJExperimental posterior penetrating eye injuries in the rabbit. I. Method of production and natural historyBr J Ophthalmol197963306311465404
- ToppingTMAbramsGWMachemerRExperimental double-perforating injury of the posterior segment in rabbit eyes: the natural history of intraocular proliferationArch Ophthalmol197997735742426694
- GregorZRyanSJComplete and core vitrectomies in the treatment of experimental posterior penetrating eye injury in the rhesus monkey. II. Histologic featuresArch Ophthalmol19831014464506830500
- HsuHTRyanSJExperimental retinal detachment in the rabbit. Penetrating ocular injury with retinal lacerationRetina1986666693704354
- BensonWEMachemerRSevere perforating injuries treated with pars plana vitrectomyAm J Ophthalmol197681728732937425
- ConwayBPMichelsRGVitrectomy techniques in the management of selected penetrating ocular injuriesOphthalmology197885560583673335
- MichelsRGVitrectomy methods in penetrating ocular traumaOphthalmology1980876296456995897
- ColemanDJEarly vitrectomy in the management of the severely traumatized eyeAm J Ophthalmol1982935435517081352
- MeredithTAGordonPAPars plana vitrectomy for severe penetrating injury with posterior segment involvementAm J Ophthalmol19871035495543565515
- FongLPEye injuries in Victoria, AustraliaMed J Aust199516264687838028
- WongTYTielschJMA population-based study on the incidence of severe ocular trauma in SingaporeAm J Ophthalmol199912834535110511030
- GilbertCMSoongHKHirstLWA two-year prospective study of penetrating ocular trauma at the Wilmer ophthalmological instituteAnn Ophthalmol1987191041063566032
- KuhnFMorrisFWitherspoonCDMesterVThe Birmingham Eye Trauma Terminology system (BETT)J Fr Ophthalmol200427206210
- WirostkoWJWilliamFMMcCabeCMDieckertJPIntraocular foreign bodiesAlbertDMJakobiecFAPrinciples and Practice of Ophthalmology2nd edPhiladelphiaSaunders200052415250
- AbramsGWToppingTMMachemerRVitrectomy for injury: the effect on intraocular proliferation following perforation of the posterior segment of the rabbit eyeArch Ophthalmol197997743748426695
- De JuanEJrSternbergPJrMichelsRGAuerCEvaluation of vitrectomy in penetrating ocular trauma. A case-control studyArch Ophthalmol1984102116011636466178
- RamsayRCCantrillHLKnoblochWHVitrectomy for double penetrating ocular injuriesAm J Ophthalmol19851005865894050932
- MorrisREWitherspoonCDFeistRMBymeJBJrOttemillerDBBilateral ocular shotgun injuryAm J Ophthalmol19871036957003578468
- SternbergPJrde JuanEJrGreenWRHirstLWSommerAOcular BB injuriesOphthalmology198491126912776514290
- HattonMPThakkarMMRaySOrbital and adnexal trauma associated with open globe injuriesOphthal Plast Reconstr Surg200218458461
- SchmidtGWBromanATHindmanHBGrantMPVision survival after open globe injury predicted by classification and regression tree analysisOphthalmology200811520220917588667
- ClearyPERyanSJMethod of production and natural history of experimental posterior penetrating eye injury in the monkeyAm J Ophthalmol197988212220112869
- RyanSJAllenAWPars plana vitrectomy in ocular traumaAm J Ophthalmol197988483491484675
- WinthropSRClearyPEMincklerDSRyanSJPenetrating eye injuries: a histopathological reviewBr J Ophthalmol1980648098177426552
- [No authors listed]Vitrectomy with silicone oil or sulfur hexafluoride gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 1Arch Ophthalmol19921107707791596224
- WarrasakSEuswasAHongsakornSPosterior segment trauma: types of injuries, result of vitreo-retinal surgery and prophylactic broad encircling scleral buckleJ Med Assoc Thai2005881916193016518994
- SkorpikCMenapaceRGnadHParousisPSilicone oil implantation in penetrating ocular injuries complicated by PVR. Result from 1982 to 1986Retina198998142717807
- HungKHYangCSKaoSCLeeFLLeeSMManagement of double-penetrating ocular injury with retained intraorbital metallic foreign bodyJ Chin Med Assoc20117452352622100024