Abstract
Interleukin-6 (IL-6) is a pleiotropic cytokine implicated in the pathogenesis of many immune-mediated disorders including several types of non-infectious uveitis. These uveitic conditions include Vogt-Koyanagi-Harada syndrome, uveitis associated with Behçet disease, and sarcoidosis. This review summarizes the role of IL-6 in immunity, highlighting its effect on Th17, Th1, and plasmablast differentiation. It reviews the downstream mediators activated in the process of IL-6 binding to its receptor complex. This review also summarizes the biologics targeting either IL-6 or the IL-6 receptor, including tocilizumab, sarilumab, sirukumab, olokizumab, clazakizumab, and siltuximab. The target, dosage, potential side effects, and potential uses of these biologics are summarized in this article based on the existing literature. In summary, anti-IL-6 therapy for non-infectious uveitis shows promise in terms of efficacy and side effect profile.
Role of interleukin-6 in immunity
Interleukin-6 (IL-6) is a pleiotropic cytokine produced by monocytes, macrophages, T-lymphocytes, and synovial fibroblasts, as well as other cell types. It is produced in response to damage-associated molecular patterns in injury, and pathogen-associated molecular patterns via toll-like receptor signaling in autoimmunity and infection (). IL-6 has a wide variety of effects on different cell types throughout the body, including induction of acute-phase reactant production by hepatocytes, B-lymphocyte differentiation, and T-lymphocyte subset differentiation (). Specifically, IL-6 plays a critical role in differentiation of CD4-positive T helper (Th) cells into Th17 cells which have been strongly implicated in the pathogenesis of immune-mediated diseases including noninfectious uveitis.Citation1,Citation2 IL-6 can also induce differentiation of CD8-positive cells into cytotoxic T-cells.Citation2,Citation3 IL-6 inhibits transforming growth factor β-mediated regulatory T-cell development, which is important in downregulating inflammatory responses.Citation2,Citation4 Additionally, IL-6 may be important in the pathogenesis of certain types of cancers, such as multiple myeloma.Citation5
Figure 1 Signaling and activity of IL-6.
Abbreviations: JAK, janus kinase; STAT3, signal transducer and activator of transcription 3; MAPK, mitogen activated protein kinase.
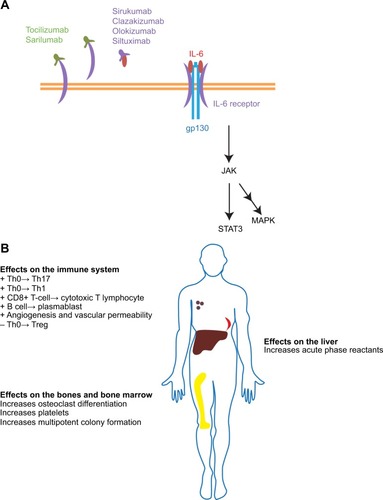
IL-6 signals in an autocrine and paracrine fashion by binding to the transmembrane cell surface IL-6 receptor as well as soluble IL-6 receptor.Citation2,Citation6 The IL-6 receptor includes the IL-6 binding domain (known as the IL-6 receptor) and the signal transduction chain, or gp130 ().Citation7 Gp130 is common to other IL-6 family cytokines including interleukin-27 (IL-27), interleukin-35 (IL-35), interleukin-11 (IL-11), leukemia inhibitory factor (LIF), oncostatin M (OSM), ciliary neurotrophic factor (CNTF), cardiotrophin 1 (CTF1), and cardiotrophin-like cytokine (CLC).Citation8
Activation of the IL-6 receptor requires a hexameric structure consisting of two molecules each of the IL-6 receptor, IL-6, and gp130.Citation7 Activated gp130 results in activation of Janus kinase (JAK) and signal transducer and activator of transcription 3 (STAT3) pathways.Citation2,Citation6,Citation8,Citation9 SH2-domain containing tyrosine phosphatase-2 and mitogen activated protein kinases (MAPK) are also activated.Citation8 IL-6 responsive genes include the acute phase reactants C-reactive protein, fibrinogen, and serum amyloid A.Citation10 They also include hepcidin which blocks the action of ferroportin, an iron transporter in the gut, thus contributing to anemia of chronic inflammatory disease.Citation11 Importantly, IL-6 can induce production of vascular endothelial growth factor, resulting in the neovascular process that can sometimes accompany inflammation.Citation12
The production of IL-6 is regulated by certain microR-NAs such as miRNA-155, and proteins such as Regnase-1, which negatively regulates IL-6 production by cells. Another regulator of IL-6 is the protein Arid5a (AT-rich interactive domain-containing protein 5a), which stabilizes IL-6 mRNA.Citation13
Role of IL-6 in uveitis and other immune-mediated diseases
Both preclinical and clinical data support the importance of IL-6 in uveitis. Yoshimura et alCitation14 demonstrated the importance of IL-6 in an animal model of T-cell mediated uveitis, experimental autoimmune uveitis (EAU), by showing that treatment of EAU mice with an anti-IL-6 receptor antibody or, alternatively, EAU induction in IL-6-deficient mice results in dramatically reduced uveitic inflammation. This effect in EAU appears to occur via the suppression of both Th1 and Th17 differentiation, both of which are important in this animal model of uveitis.Citation15 These same authors demonstrated elevated IL-6 concentrations in the vitreous fluid of chronic uveitis patients (with Vogt–Koyanagi–Harada syndrome, Behçet disease, sarcoidosis, and idiopathic uveitis), compared to nonuveitic patients (samples obtained from diabetic retinopathy, epiretinal membrane, and macular hole patients).Citation14 Perez et alCitation16 demonstrated that IL-6 was higher in the vitreous of patients with active intermediate or posterior uveitis compared to control patients. Even prior to the two above publications, however, Murray et alCitation17 had demonstrated elevated aqueous humor levels of IL-6 in 24 patients with uveitis including in Fuchs’ heterochromic iridocyclitis (n=16) and Toxoplasma uveitis (n=8). IL-6 levels are elevated in the serum of active uveitis patients as well.Citation18
While rheumatoid arthritis (RA) is not commonly associated with uveitis, IL-6 production is dysregulated in the synovial fluid of RA patients.Citation19 IL-6 and soluble IL-6 receptor are elevated in the serum of RA patients, and appear to correlate with disease activity.Citation20 Castleman disease, a condition resulting in lymphadenopathy, fever, night sweats, fatigue, and weight loss, is very rarely associated with uveitis.Citation21 Oshitari et alCitation21 showed that IL-6 aqueous levels were elevated in a patient with Castleman disease with anterior uveitis and retinal vasculitis resistant to oral steroid treatment but amenable to anti-IL-6 receptor antibody treatment. In juvenile idiopathic arthritis (JIA), serum IL-6 appears to be elevated in patients with active disease compared to inactive disease. It has been demonstrated that IL-6 levels decrease upon treatment in these patients.Citation22,Citation23 summarizes the uveitic and systemic disorders associated with dysregulated IL-6 or IL-6 receptor ().
Table 1 Conditions in which IL-6 plays a role in pathogenesis
Targeting IL-6 for uveitis and systemic inflammatory disorders
Tocilizumab (Genentech, South San Francisco, CA, USA) is a monoclonal antibody against soluble and membrane-bound IL-6 receptor that is approved for the treatment of moderate to severe RA and JIA that has failed treatment with other disease modifying biologics. It has been used successfully in case reports in JIA uveitis refractory to prior TNF-α blockade,Citation24,Citation25 Castleman disease-associated uveitis, birdshot chorioretinopathy, Behçet disease, and refractory idiopathic uveitis.Citation15,Citation26–Citation28 Doses used are described in .
Table 2 Summary of anti-IL-6 or IL-6R biologics
In a retrospective study of eight eyes from five patients with uveitic cystoid macular edema (CME) refractory to traditional immunosuppressive therapy or anti-TNF-α treatment, Adan et alCitation26 showed that tocilizumab was effective in treating CME at month 1, and as late as 6 months after follow-up. Tocilizumab maintained control of macular edema even after tapering other immunosuppressive agents.Citation26
The same group also published a series involving eleven eyes from seven patients with uveitic CME due to birdshot chorioretinopathy, JIA, and idiopathic panuveitis.Citation27 Both mean logMAR visual acuity and central foveal thickness by optical coherence tomography (OCT) improved after treatment with tocilizumab at the 1 year follow-up. Two patients withdrew from the study due to sustained remission at 12 months, but in both patients, CME relapsed within 3 months after tocilizumab withdrawal. No serious adverse events were reported in this small study of uveitis patients.Citation27 In a separate study, Papo et alCitation28 treated eight consecutive severe refractory uveitis patients with 8 mg/kg of tocilizumab, IV, every 4 weeks. They showed that six out of the eight patients responded to tocilizumab with visual acuity improvement in five patients. Side effects included bronchitis (n=1), leukopenia (n=1), and thrombocytopenia (n=1). Two separate Phase I/II clinical trials are ongoing (www.clinicaltrials.gov) to study the efficacy of tocilizumab in noninfectious intermediate, posterior or panuveitis (STOP-Uveitis) and in JIA-associated uveitis.Citation13 A Phase III clinical trial for tocilizumab (also at www.clinicaltrials.gov) in the treatment of sight-threatening Graves orbitopathy not responsive to intravenous corticosteroids is also enrolling patients.
Sirukumab (Janssen Biologics, Horsham, PA Glaxo SmithKline, Brentford, UK), a human monoclonal antibody that binds IL-6, is currently undergoing a Phase III clinical trial for RA not responsive to methotrexate or anti-TNF-α treatment, and is being studied as monotherapy in a comparative efficacy trial with adalimumab.Citation29 Smolen et alCitation30 reported the results of a Phase II study in RA patients refractory to methotrexate. In their study, the primary endpoint of ACR50 scores was achieved at week 12 using sirukumab 100 mg every 2 weeks. ACR50 refers to a 50% improvement in RA as determined by guidelines set forth by the American College of Rheumatology. This is determined by the percentage of improvement in tender and swollen joints.
Sarilumab (Regeneron Pharmaceuticals, Tarrytown, NY, USA) is a human anti-IL-6 receptor monoclonal antibody also undergoing several Phase III clinical trials for use as monotherapy and in conjunction with drugs like methtorexate therapy for RA. In a study in which 306 active RA patients refractory to methotrexate treatment were randomized to 1 of 6 treatment arms of varying doses of sarilumab, the proportion of patients achieving the primary endpoint, based on an ACR20 (20% improvement according to guidelines set forth by the American College of Rheumatology) at week 12, was higher in sarilumab 150 mg weekly or every other week groups compared with the placebo.Citation31 A multicenter Phase II trial, the SATURN Study, to evaluate the efficacy of sarilumab in noninfectious intermediate, posterior, and panuveitis is currently enrolling subjects.Citation13
Other IL-6 biologics include olokizumab (UCB, Brus-sels, Belgium), clazakizumab (Alder BioPharmaceuticals, Bothell, WA, USA), and siltuximab (Janssen, Horsham, PA, USA). Olokizumab is a humanized anti-IL-6 monoclonal antibody that was effective in a 12 week Phase IIb study in RA patients who were refractory to TNF inhibitors.Citation32 Clazakizumab is also a humanized anti-IL-6 monoclonal antibody that achieved its primary endpoint in treating RA patients refractory to methotrexate.Citation33 Siltuximab (CNTO 328) is a human–murine anti-IL-6 monoclonal antibody, which has been studied in clinical trials for a number of diseases including prostate cancer, renal cancer, ovarian cancer, Castleman disease, and multiple myeloma.Citation6,Citation34 summarizes the biologics targeting IL-6 or the IL-6 receptor.
Adverse side effects and work up
Commonly reported adverse events that have been reported in the clinical trials for anti-IL-6 or IL-6 receptor antibodies appear to be similar, and include gastrointestinal disorders, respiratory tract infections, urinary tract infections, and nervous system disorders.Citation29 No cases of tuberculosis were reported, although most patients will have received testing to rule out tuberculosis prior to receiving these therapies. Common laboratory findings included neutropenia or other hematologic changes, elevated liver function tests, and elevated serum lipids, although establishing a causal role for these changes with these biologics requires further investigation.Citation29–Citation31,Citation33
Disclosure
The author reports no conflicts of interest in this work.
References
- KornTMitsdoerfferMCroxfordALIL-6 controls Th17 immunity in vivo by inhibiting the conversion of conventional T cells into Foxp3+ regulatory T cellsProc Natl Acad Sci U S A200810547184601846519015529
- TanakaTNarazakiMKishimotoTIL-6 in inflammation, immunity, and diseaseCold Spring Harb Perspect Biol2014610a01629525190079
- OkadaMKitaharaMKishimotoSMatsudaTHiranoTKishimotoTIL-6/BSF-2 functions as a killer helper factor in the in vitro induction of cytotoxic T cellsJ Immunol19881415154315493261754
- BettelliECarrierYGaoWReciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cellsNature2006441709023523816648838
- VoorheesPMChenQSmallGWTargeted inhibition of interleukin-6 with CNTO 328 sensitizes pre-clinical models of multiple myeloma to dexamethasone-mediated cell deathBr J Haematol2009145448149019344406
- Ataie-KachoiePPourgholamiMHMorrisDLInhibition of the IL-6 signaling pathway: a strategy to combat chronic inflammatory diseases and cancerCytokine Growth Factor Rev201324216317323107589
- YamasakiKTagaTHirataYCloning and expression of the human interleukin-6 (BSF-2/IFN beta 2) receptorScience198824148678258283136546
- TanakaTNarazakiMOgataAKishimotoTA new era for the treatment of inflammatory autoimmune diseases by interleukin-6 blockade strategySemin Immunol2014261889624594001
- KimNHLeeMYParkSJChoiJSOhMKKimISAuranofin blocks interleukin-6 signalling by inhibiting phosphorylation of JAK1 and STAT3Immunology2007122460761417645497
- HeinrichPCCastellJVAndusTInterleukin-6 and the acute phase responseBiochem J199026536216361689567
- NemethERiveraSGabayanVIL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidinJ Clin Invest200411391271127615124018
- TzengHETsaiCHChangZLInterleukin-6 induces vascular endothelial growth factor expression and promotes angiogenesis through apoptosis signal-regulating kinase 1 in human osteosarcomaBiochem Pharmacol201385453154023219526
- MayaJRSadiqMAZapataLJEmerging therapies for noninfectious uveitis: what may be coming to the clinicsJ Ophthalmol2014201431032924868451
- YoshimuraTSonodaKHOhguroNInvolvement of Th17 cells and the effect of anti-IL-6 therapy in autoimmune uveitisRheumatology200948434735419164426
- MesquidaMLeszczynskaALlorencVAdanAInterleukin-6 blockade in ocular inflammatory diseasesClin Exp Immunol2014176330130924528300
- PerezVLPapaliodisGNChuDAnzaarFChristenWFosterCSElevated levels of interleukin 6 in the vitreous fluid of patients with pars planitis and posterior uveitis: the Massachusetts eye and ear experience and review of previous studiesOcul Immunol Inflamm200412319320115385196
- MurrayPIHoekzemaRvan HarenMAde HonFDKijlstraAAqueous humor interleukin-6 levels in uveitisInvest Ophthalmol Vis Sci19903159179202335453
- KramerMMonseliseYBaharICohenYWeinbergerDGoldenberg-CohenNSerum cytokine levels in active uveitis and remissionCurr Eye Res2007327–866967517852191
- HiranoTMatsudaTTurnerMExcessive production of interleukin 6/B cell stimulatory factor-2 in rheumatoid arthritisEur J Immunol19881811179718012462501
- StuartRALittlewoodAJMaddisonPJHallNDElevated serum interleukin-6 levels associated with active disease in systemic connective tissue disordersClin Exp Rheumatol199513117227774098
- OshitariTKajitaFTobeARefractory uveitis in patient with castleman disease successfully treated with tocilizumabCase Rep Ophthalmol Med2012201296818023198204
- Kaminiarczyk-PyzalkaDAdamczakKMikosHKlimeckaIMoczkoJNiedzielaMProinflammatory cytokines in monitoring the course of disease and effectiveness of treatment with etanercept (ETN) of children with oligo- and polyarticular juvenile idiopathic arthritis (JIA)Clin Lab20146091481149025291944
- SpirchezMSamascaGIancuMBolbaCMiuNRelation of interleukin-6, TNF-alpha and interleukin-1alpha with disease activity and severity in juvenile idiopathic arthritis patientsClin Lab2012583–425326022582498
- TappeinerCHeinzCGanserGHeiligenhausAIs tocilizumab an effective option for treatment of refractory uveitis associated with juvenile idiopathic arthritis?J Rheumatol20123961294129522661419
- TsangACRothJGottliebCTocilizumab for severe chronic anterior uveitis associated with juvenile idiopathic arthritis in a pediatric patientOcul Immunol Inflamm201422215515724377416
- AdanAMesquidaMLlorencVTocilizumab treatment for refractory uveitis-related cystoid macular edemaGraefes Arch Clin Exp Ophthalmol2013251112627263223893042
- MesquidaMMolinsBLlorencVSainz de la MazaMAdanALong-term effects of tocilizumab therapy for refractory uveitis-related macular edemaOphthalmology2014121122380238625204610
- PapoMBielefeldPValletHTocilizumab in severe and refractory non-infectious uveitisClin Exp Rheumatol2014324 Suppl 84S75S7925268663
- TanakaYMartin MolaEIL-6 targeting compared to TNF targeting in rheumatoid arthritis: studies of olokizumab, sarilumab and sirukumabAnn Rheum Dis20147391595159724833786
- SmolenJSWeinblattMEShengSZhuangYHsuBSirukumab, a human anti-interleukin-6 monoclonal antibody: a randomised, 2-part (proof-of-concept and dose-finding), phase II study in patients with active rheumatoid arthritis despite methotrexate therapyAnn Rheum Dis20147391616162524699939
- HuizingaTWFleischmannRMJassonMSarilumab, a fully human monoclonal antibody against IL-6Ralpha in patients with rheumatoid arthritis and an inadequate response to methotrexate: efficacy and safety results from the randomised SARIL-RA-MOBILITY Part A trialAnn Rheum Dis20147391626163424297381
- GenoveseMCFleischmannRFurstDEfficacy and safety of olokizumab in patients with rheumatoid arthritis with an inadequate response to TNF inhibitor therapy: outcomes of a randomised Phase IIb studyAnn Rheum Dis20147391607161524641941
- MeasePStrandVShalamberidzeLA phase II, double-blind, randomised, placebo-controlled study of BMS945429 (ALD518) in patients with rheumatoid arthritis with an inadequate response to methotrexateAnn Rheum Dis20127171183118922328739
- KurzrockRVoorheesPMCasperCA phase I, open-label study of siltuximab, an anti-IL-6 monoclonal antibody, in patients with B-cell non-Hodgkin lymphoma, multiple myeloma, or Castleman diseaseClin Cancer Res201319133659367023659971
- El-AsrarAMStruyfSKangaveDCytokine profiles in aqueous humor of patients with different clinical entities of endogenous uveitisClin Immunol2011139217718421334264
- Montero-JulianFAThe soluble IL-6 receptors: serum levels and biological functionCell Mol Biol200147458359711502067
- MuangchantCPopeJEThe significance of interleukin-6 and C-reactive protein in systemic sclerosis: a systematic literature reviewClin Exp Rheumatol2013312 Suppl 7612213423910616
- PignattiPCiapponiLGallePHigh circulating levels of biologically inactive IL-6/SIL-6 receptor complexes in systemic juvenile idiopathic arthritis: evidence for serum factors interfering with the binding to gp130Clin Exp Immunol2003131235536312562400
- ShimamotoKItoTOzakiYSerum interleukin 6 before and after therapy with tocilizumab is a principal biomarker in patients with rheumatoid arthritisJ Rheumatol20134071074108123637318
- BorgesAHO’ConnorJLPhillipsANFactors associated with plasma IL-6 levels during HIV infectionJ Infect Dis Epub2262015
- LykeKEBurgesRCissokoYSerum levels of the proinflammatory cytokines interleukin-1 beta (IL-1beta), IL-6, IL-8, IL-10, tumor necrosis factor alpha, and IL-12(p70) in Malian children with severe Plasmodium falciparum malaria and matched uncomplicated malaria or healthy controlsInfect Immun200472105630563715385460
- ZhouYHoriuchiSYamamotoMYamamotoNElevated serum levels of the soluble form of gp130, the IL-6 signal transducer, in HTLV-1 infection and no involvement of alternative splicing for its generationMicrobiol Immunol19984221091169572042
- ChiNTanZMaKBaoLYunZIncreased circulating myeloid-derived suppressor cells correlate with cancer stages, interleukin-8 and -6 in prostate cancerInt J Clin Exp Med20147103181319225419348
- LuCCKuoHCWangFSJouMHLeeKCChuangJHUpregulation of TLRs and IL-6 as a marker in human colorectal cancerInt J Mol Sci201516115917725547486
- MarkkulaASimonssonMIngvarCRoseCJernstromHIL6 genotype, tumour ER-status, and treatment predicted disease-free survival in a prospective breast cancer cohortBMC Cancer20141475925305747
- NeematKRaniaKTarekMHamdyAAEffect of 13q deletion on IL-6 production in patients with multiple myeloma: a hypothesis may hold trueClin Lab20146081393139925185427
- MalmestromCAnderssonBAHaghighiSLyckeJIL-6 and CCL2 levels in CSF are associated with the clinical course of MS: implications for their possible immunopathogenic rolesJ Neuroimmunol20061751–217618216626811
- UsluSAkarkarasuZEOzbabalikDLevels of amyloid beta-42, interleukin-6 and tumor necrosis factor-alpha in Alzheimer’s disease and vascular dementiaNeurochem Res20123771554155922437436
