Abstract
We report one case of malignant hypertensive retinopathy as a presenting sign of fetal death in utero. Ophthalmic examination (including intravenous fluorescein angiography and optical coherence tomography) and obstetric and systemic evaluation were performed, providing a multidisciplinary approach. A 33-year-old overweight woman (body mass index 47 kg/m2) with no systemic or ocular known disease was admitted to our emergency department with a one-week history of bilateral vision loss and no systemic complaints. On examination, best corrected visual acuity was 1/10 in the right eye and 1/10 in the left eye. Anterior segment examination of both eyes was unremarkable. Ophthalmoscopic fundus findings included bilateral optic disc edema, diffuse cotton wool spots, intraretinal exudates, retinal hemorrhages, and multiple serous retinal detachments involving both maculae. Physical examination revealed a blood pressure of 220/110 mmHg. Further systemic workup revealed a previously unknown 35-week pregnancy with a dead fetus. An emergency cesarean section was performed. Pre-eclampsia is a life-threatening disorder for both mother and fetus. This case highlights the need to rule out pre-eclampsia in all women of childbearing age presenting with ocular signs of malignant hypertension, even without external signs of pregnancy.
Introduction
Pre-eclampsia complicates 2%–8% of pregnancies, and remains a leading cause of maternal and perinatal morbidity and mortality.Citation1,Citation2 It is a pregnancy-specific disease generally defined as new hypertension (>140 mmHg systolic or >90 mmHg diastolic blood pressure)Citation3 and substantial proteinuria (≥300 mg in 24 hours) at or after 20 weeks’ gestation.Citation4 However, the precise definition of this syndrome and the criteria to differentiate mild from severe disease are still being debated.Citation3,Citation5 Several clinical and laboratory parameters have classically been used for defining the severity of pre-eclampsia.Citation6 Current determination of more severe cases depends mostly on pressure levels and proteinuria, and also the clinical presentation, namely the presence of symptoms such as headache, epigastric pain, and visual disturbances. This systemic disorder can affect almost every organ. Although the cause of pre-eclampsia remains largely unknown, it is characterized by vasospasm and endothelial activation.Citation7
The visual system may be affected in 30%–100% of patients with pre-eclampsia.Citation2,Citation8 Blurred vision, although rare, is the most common symptom. Other signs such as photophobia, visual spots and diplopia may be observed, and are usually attributed to posterior cerebral artery vasospasm with ischemia, or to cerebral edema in the occipital area. Although retina and its vasculature are more usually affected, the conjunctiva, choroid, the optic nerve and visual cortex may be also affected in pre-eclampsia.Citation7 The most prominent finding is terminal arteriolar vasospasm, associated with the development of systemic hypertension.Citation7
We herein report a case of severe pre-eclampsia with bilateral vision loss as the presenting symptom, in a woman with an unknown pregnancy.
Case report
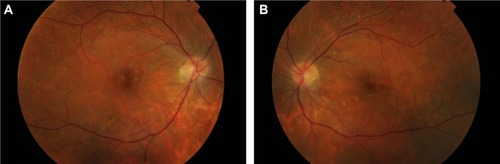
A 33-year-old woman with morbid obesity (body mass index 47 kg/m2; mean value approximately 25 kg/m2 for the age-matched and sex-matched populationCitation9), without a history of systemic or ocular disease, presented with a one-week history of bilateral vision loss and no systemic complaints. On examination, best corrected visual acuity was 1/10 in the right eye and 1/10 in the left eye. Anterior segment examination of both eyes was normal. Ophthalmoscopic fundus examination (with noncontact slit-lamp lens) revealed bilateral optic disc edema, cotton wool spots, intraretinal exudates, retinal hemorrhages, macular edema, and serous retinal detachments that were inferior to the optic disc and without macular involvement. Blood pressure was 220/110 mmHg. The patient was transferred to the intensive care unit for therapeutic management of hypertension and systemic workup. Laboratory examinations showed thrombocytopenia (67×109/L) and elevated beta-human chorionic gonadotrophin (6,000 mUI/mL), with no other relevant findings. Ultrasonography revealed a previously unknown pregnancy with a dead fetus. An emergency cesarean section was preferred, considering the surgical risk. Tensional control was achieved post partum. Ophthalmologic fundus examination 12 hours after delivery had similar results, ie, bilateral optic disc edema, narrowing and irregularity of the retinal arteries, with arteriovenous nicking, diffuse cotton wool spots, intraretinal and subretinal exudates, and multiple superficial and deep retinal hemorrhages ().
Figure 1 Retinography 12 hours post partum.
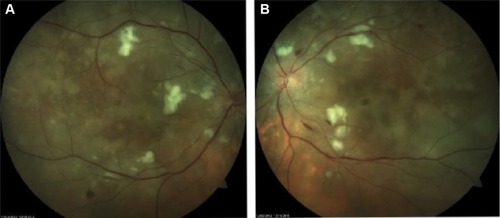
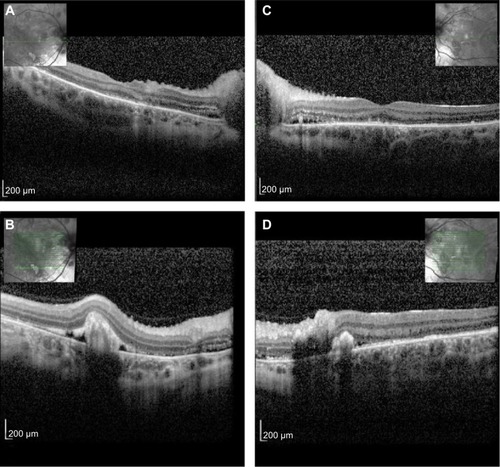
Fluorescein angiogram 12 hours post partum revealed delayed perfusion of the choriocapillaris in both eyes. The posterior pole and peripheral retina presented multiple capillary dilations, focal venous beading, capillary nonperfusion areas, retinal hemorrhages, and late leakage in the optic disc. Multiple areas of focal choroidal ischemia (Elschnig’s spots) were seen (). Optical coherence tomography 12 hours post partum showed retinal edema, retinal serous detachments presenting with a hyperreflective posterior surface of the detached retina, subretinal hyperreflective lesions corresponding to subretinal exudates, and a thickened peripapillary retinal nerve fiber layer corresponding to optic disc edema (). Follow-up examination 6 months after the acute phase revealed complete resolution of previous serous detachments, diffuse arteriolar constriction, and multiple yellowish subretinal discoloration spots ().
Figure 2 Fluorescein angiogram in early and late phases 12 hours post partum.
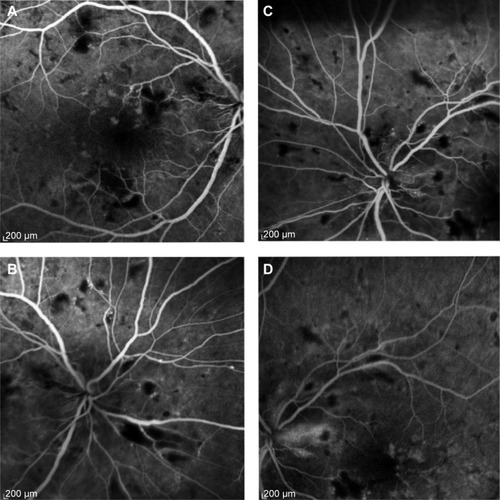
Figure 3 Optical coherence tomography 12 hours post partum.
Discussion
Pre-eclampsia is a life-threatening disorder for both the mother and fetus, and complicates 2%–8%Citation1,Citation2 of all pregnancies. It occurs from 20 weeks of gestation up to 6 weeks post partum. It is classified as hypertension developing after 20 weeks of gestation and the coexistence of one or more of the following new-onset conditions: proteinuria, other maternal organ dysfunction (renal insufficiency, liver involvement, neurologic complications, hematologic complications) or uteroplacental dysfunction (fetal growth restriction).Citation3 The commonest ocular finding is severe arteriolar spasm, evidenced by either segmental or generalized constriction of the retinal arterioles, reported in 70% of cases.Citation10 Retinal hemorrhages, edema, and cotton wool spots secondary to arteriolar damage may follow. The severity of retinal arteriolar changes is more closely related to the degree of underlying vasospasm, which may or may not be associated with the blood pressure level. Schultz and O’Brien described the fundus appearance of 47 patients with pre-eclampsia.Citation11 Hemorrhages, cotton wool spots, and exudates were seen in 12 patients, all of whom had blood pressure ranging from 170/115 mmHg to 230/160 mmHg. Serous retinal detachment is an unusual but well documented cause of visual loss in pre-eclampsia. It affects 1%–2% of patients in its most severe form and is slightly more common in the eclamptic patient.Citation7 It may be present either before or after delivery. Bilateral, bullous, and serous detachments are usually present, and are frequently observed in the absence of significant retinal vascular abnormalities. It is believed that choroidal ischemia secondary to intensive arteriolar vasospasm is the cause of these serous retinal detachments.Citation12
There is still controversy as to whether the presence of these detachments may influence fetal or maternal prognosis. The choroid vascular insufficiency can lead to lesions in the retinal pigment epithelium, fluid transudation, and focal retinal detachment.Citation12,Citation13 The Elschnig’s spots, also found in this case, demonstrate areas of focal occlusion of the choriocapillaris that lead to necrosis and focal atrophy of the retinal pigment epithelium. The optic disc edema seen in this case was caused by local ischemia, as a result of intensive vasospasm of the posterior ciliary arteries supplying its head.
Unusual in this case was the unknown late pregnancy masked by the extreme obesity in a woman who presented with ocular signs of malignant hypertension that included hypertensive retinopathy, choroidopathy and optic neuropathy. This case highlights the need to rule out pre-eclampsia in all women of childbearing age who present with ocular signs of malignant hypertension, even without a known history or external signs of pregnancy, which were masked by morbid obesity in our patient. This case also highlights the critical role ophthalmologists may play in the diagnosis of this potentially devastating disease.
Disclosure
The authors report no conflicts of interest in this work.
References
- DuleyLThe global impact of pre-eclampsia and eclampsiaSemin Perinatol200933313013719464502
- KhanKSWojdylaDSayLGulmezogluAMVan LookPFWHO analysis of causes of maternal death: a systematic reviewLancet200636795161066107416581405
- TranquilliALDekkerGMageeLThe classification, diagnosis and management of the hypertensive disorders of pregnancy: a revised statement from the ISSHPPregnancy Hypertens20144297104
- MilneFRedmanCWalkerJThe pre-eclampsia community guideline (PRECOG): how to screen for and detect onset of pre-eclampsia in the communityBMJ2005330749157658015760998
- TranquilliABrownMZeemanGDekkerGSibaiBThe definition of severe and early-onset preeclampsia. Statements from the International Society for the Study of Hypertension in Pregnancy (ISSHP)Pregnancy Hypertens2013314447
- [No authors listed]Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in PregnancyAm J Obstet Gynecol20001831S1S22
- OberRRPregnancy-induced hypertension (pre-clampsia eclampsia)RyanSJRetina, Volume 2St LouisCV Mosby199413931403
- RoosNMWiegmanMJJansoniusNMZeemanGGVisual disturbances in (pre)eclampsiaObstet Gynecol Surv201267424225022495060
- CarreiraHPereiraMAzevedoALunetNTrends of BMI and prevalence of overweight and obesity in Portugal (1995–2005): a systematic reviewPublic Health Nutr201215697298122369750
- WagnerHPArterioles of the retina in toxemia of pregnancyJAMA19331011813801384
- SchultzJFO’BrienCSRetinal changes in hypertensive toxemia of pregnancy: A report of 47 casesAm J Ophthalmol193821767774
- FastenbergDMFetkenhourCLChoromokosEShochDEChoroidal vascular changes in toxemia of pregnancyAm J Ophthalmol19808933623687369296
- SaitoYTanoYRetinal pigment epithelial lesions associated with choroidal ischemia in preeclampsiaRetina19981821031089564689