Abstract
Background
There are some cases that reported central retinal vein occlusion accompanied by ciliary artery occlusion, however, combined branch retinal artery and vein occlusion is a rare condition that has been infrequently reported. We describe in this report one case of retinal vein occlusion and branch retinal artery occlusion occurring simultaneously.
Case presentation
A 50 year-old woman presented with acute visual loss in her right eye. Fundus photography showed retinal ischemia and tortuous, dilated retinal veins in the right eye. With early phase fluorescein angiography, retinal arteries revealed areas absent of branches. Late phase fluorescein angiography demonstrated that areas absent of branches were still present.
Conclusion
It is a rare case of branch retinal artery and vein occlusion.
Background
The pathophysiology of branch retinal vein occlusion (BRVO) consists of thrombosis caused by narrowing of the retinal vein at the arteriovenous crossing site and consequent retinal vein occlusion. When the retinal vein is obstructed, the blood pressure increases in the retinal vein distal to the site of occlusion, which eventually causes hemorrhage due to vascular breakdown.
On the other hand, branch retinal artery occlusion (BRAO) is a disorder that shows an occluded branch retinal artery because of thrombosis, emboli or some other causes. Consequently the blood flow to the retina will be suspended.
There are some case reports on central retinal vein occlusion accompanied by retinal artery occlusion, however, there are few reports on BRVO and BRAO occurring simultaneously in the same quadrant of the retina.
We observed a case in which BRAO and BRVO occurred at the same time because of hypertension.
Case presentation
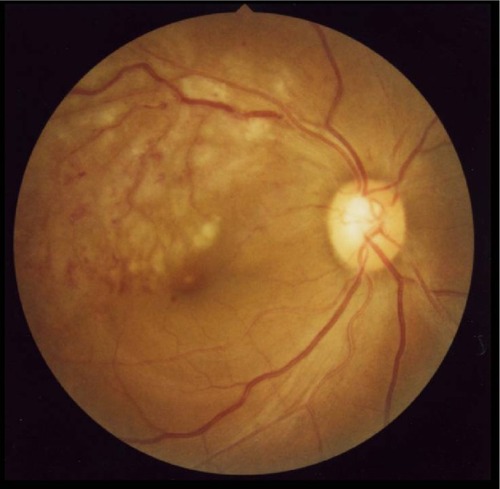
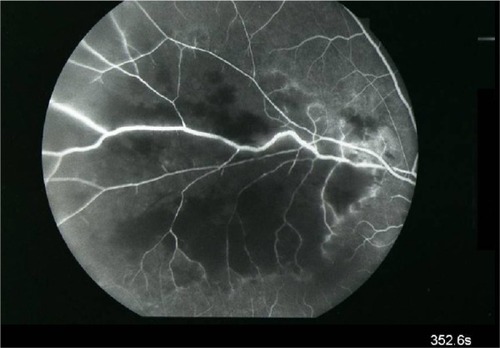
A 50 year-old female noticed a sudden vision loss in her right eye. Decimal visual acuity was 0.2 in the right eye and 1.5 in the left eye. Intraocular pressure was 15 mmHg in both eyes. Biomicroscopic examination of the anterior segment was unremarkable bilaterally. Fundus examination was unremarkable in the left eye. Fundus examination in the right eye revealed retinal ischemia and tortuous, dilated retinal veins in the supra temporal quadrant of the retina (). Fluorescein angiography of the right eye showed significantly delayed filling of the branches of the superior retinal artery in the ischemic area (27.9 sec) (). The retinal vein was dilated and tortuous. The retinal artery exhibited sludging (70 sec) (). Late phase examination revealed areas absent of branches (352.6 sec) (). We diagnosed the case as BRAO combined with BRVO. Therefore, aspirin was prescribed one tablet/day. She had previously been diagnosed with hypertension but abandoned the treatment. Immediately, we consulted the Department of Internal Medicine of the university hospital, where her blood pressure was measured as 180/110 mmHg.
Figure 2 Fluorescein angiography of the right eye showed significantly delayed filling of the branches of the superior retinal artery in the ischemic area (27.9 sec).

Figure 3 The retinal vein was dilated and tortuous.
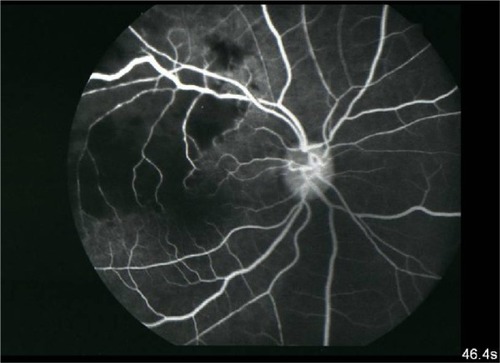
Figure 4 A capillary non-perfusion in the circulation of the supratemporal vein was also noticed.
Amlodipine besilate was administered 5 mg/day. Two weeks later, her right visual acuity had improved to 0.5. One month after administration of amlodipine, her blood pressure did not recover to normal. Therefore, telmisartan was prescribed additionally for 40 mg/day. Afterwards, fundus appearance was improved, and retinal opacity and retinal vessel abnormality disappeared. Nine months later, her visual acuity improved to 1.5. Her blood pressure was 125/80 mmHg.
Conclusion
It is very rare that retinal artery occlusion and retinal vein occlusion occur simultaneously. In these cases of combined retinal artery and vein occlusion, the most frequent cases are central retinal vein occlusion accompanied by ciliary artery occlusion.Citation1
The main fundus finding of this case was retinal opacity, therefore, BRAO could be suspected. However, we also saw dilated, tortuous retinal veins. Therefore, we diagnosed it as BRAO accompanied by BRVO. Usually BRAO has thrombosis in the retinal artery, however, this case did not exhibit thrombosis.
There were three cases that reported branch retinal artery and vein occlusion (BRAVO) in the past: the first case occurred with a foreign object causing a laceration of the optic nerve and subsequent retinal vascular occlusions,Citation2 the second case happened during hepatitis C treatment with interferon and ribavirin,Citation3 and the third one presented with hypertension and type 2 diabetes mellitus.Citation4
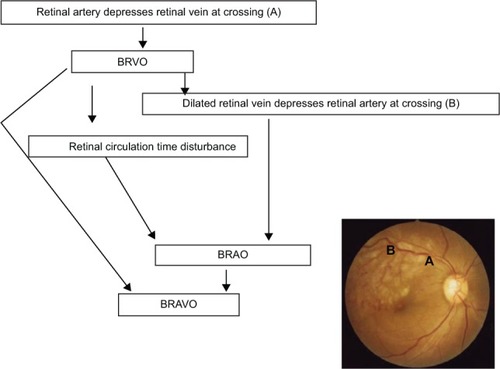
The case reported by An and Kwon resembles the present case.Citation4 Compared to the present case, their case showed pale retinal artery indicating more severe occlusion and a higher degree of retinal opacity than our case. Their case did not show remarkable dilatation or tortuosity of retinal veins. Fluorescein angiography revealed nonvascular areas and remarkable dye leakage. Their case showed severe retinal ischemia that should have triggered neovascular glaucoma. Our case did not develop neovascular glaucoma; we suggest that it was because the retinal ischemia improved at an early stage. We speculate that it might have followed the mechanism shown in . First, hypertension probably causes compression of the retinal vein by the retinal artery at the crossing point, which, in return, causes retinal vein pressure to elevate (BRVO). Next, the elevated retinal vein pressure may cause the retinal vein to be dilated and tortuous. Then, the dilated and tortuous retinal vein, in return, compresses the retinal artery at the reverse-crossing point, where the vein crosses over the artery (BRAO). And finally BRAVO is formed.
Figure 5 Suggested mechanism of BRAVO.
Abbreviations: BRVO, branch retinal vein occlusion; BRAO, branch retinal artery occlusion; BRAVO, branch retinal artery and vein occlusion.
Acknowledgments
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Disclosure
The authors report no conflicts of interest in this work.
References
- HayrehSSFraterrigoLJonasJCentral retinal vein occlusion associated with cilioretinal artery occlusionRetina200828458159418398361
- NicoloMArtioliSLa MattinaGCGhiglioneDCalabriaGBranch retinal artery occlusion combined with branch retinal vein occlusion in a patient with hepatitis C treated with interferon and ribavirinEur J Ophthalmol200515681181416329072
- LeeMWLeeSYOngSGOptic disc laceration with combined retinal artery and vein occlusion following penetrating injuryClin Experiment Ophthalomol2007355486490
- AnTSKwonSINeovascular Glaucoma Due to Branch Retinal Vein Occlusion Combined with Branch Retinal Artery OcclusionKorean J Ophthalmol2013271646723372385