Abstract
Diabetic macular edema (DME) resembles a chronic, low-grade inflammatory reaction, and is characterized by blood–retinal barrier (BRB) breakdown and retinal capillary leakage. Corticosteroids are of therapeutic benefit because of their anti-inflammatory, antiangiogenic, and BRB-stabilizing properties. Delivery modes include periocular and intravitreal (via pars plana) injection. To offset the short intravitreal half-life of corticosteroid solutions (~3 hours) and the need for frequent intravitreal injections, sustained-release intravitreal corticosteroid implants have been developed. Dexamethasone intravitreal implant provides retinal drug delivery for ≤6 months and recently has been approved for use in the treatment of DME. Pooled findings (n=1,048) from two large-scale, randomized Phase III trials indicated that dexamethasone intravitreal implant (0.35 mg and 0.7 mg) administered at ≥6-month intervals produced sustained improvements in best-corrected visual acuity (BCVA) and macular edema. Significantly more patients showed a ≥15-letter gain in BCVA at 3 years with dexamethasone intravitreal implant 0.35 mg and 0.7 mg than with sham injection (18.4% and 22.2% vs 12.0%). Anatomical assessments showed rapid and sustained reductions in macular edema and slowing of retinopathy progression. Phase II study findings suggest that dexamethasone intravitreal implant is effective in focal, cystoid, and diffuse DME, in vitrectomized eyes, and in combination with laser therapy. Ocular complications of dexamethasone intravitreal implant in Phase III trials included cataract-related events (66.0% in phakic patients), intraocular pressure elevation ≥25 mmHg (29.7%), conjunctival hemorrhage (23.5%), vitreous hemorrhage (10.0%), macular fibrosis (8.3%), conjunctival hyperemia (7.2%), eye pain (6.1%), vitreous detachment (5.8%), and dry eye (5.8%); injection-related complications (eg, retinal tear/detachment, vitreous loss, endophthalmitis) were infrequent (<2%). Dexamethasone intravitreal implant offers a viable treatment option for DME, especially in cases that are persistent or treatment (anti-vascular endothelial growth factor/laser) refractory.
Introduction
Diabetic retinopathy is a frequent microvascular complication of diabetes types 1 and 2 and represents the leading cause of blindness among adults of working age in the developed world.Citation1 Diabetes-related central vision loss can arise either from microvascular occlusion (macular ischemia) or from microvascular leakage due to breakdown of the inner blood–retinal barrier (BRB), leading to thickening or swelling of the macula (macular edema).Citation2,Citation3 Diabetic macular edema (DME) affects an estimated 21 million individuals worldwide.Citation4
Once diabetic retinopathy progresses to macular edema, treatment is indicated to slow the rate of vision loss and improve the long-term prognosis. For the past three decades, laser photocoagulation has been the mainstay of treatment for patients with DME; however, although effective in preserving vision, this form of therapy is of limited effect in restoring lost vision.Citation5
In recent years, several alternative treatment options have emerged that offer the promise of long-term improvement in visual acuity, including intravitreal anti-vascular endothelial growth factor (anti-VEGF) agents and corticosteroids.Citation5 Intravitreal anti-VEGF agents, either alone or as an adjunct to laser photocoagulation, have emerged as the preferred treatment for DME (particularly DME with foveal involvement) on account of their established efficacy, low incidence of complications, and relative ease of administration. Injectable intravitreal corticosteroids are effective agents for persistent or treatment-refractory DME, but their high rates of intraocular pressure (IOP) elevation and cataract consign their role to second-line therapy for most patients. In order to reduce the frequent dosing requirements of injectable intravitreal corticosteroid solutions and the associated risk of injection-related complications, sustained-release corticosteroid intravitreal implants have been developed.
Dexamethasone intravitreal implant 0.7 mg (Ozurdex®, Allergan, Inc., Irvine, CA, USA) is a biodegradable drug delivery system that has been approved for use in the treatment of macular edema secondary to retinal vein occlusion, noninfectious posterior uveitis, and more recently DME. This review evaluates the current evidence of the efficacy and safety of dexamethasone intravitreal implant in the treatment of DME.
Role of inflammation in the pathogenesis of DME
Early retinal microvascular changes in diabetes include thickening of the capillary basement membrane, loss of pericytes, vascular hyperpermeability, and capillary dilatation. Animal models have suggested that these changes can occur within weeks of diabetes onset.Citation3,Citation6,Citation7 Hyperglycemia is the major driver of initial pathophysiology, with both the Diabetes Control and Complications Trial and the UK Prospective Diabetes Study firmly establishing an inverse correlation between proactive glycemic control and development of retinopathy.Citation8,Citation9 While the inciting events are still unclear, high concentrations of glucose are known to induce endothelial dysfunction, leading to BRB breakdown and retinal vascular leakage.Citation3,Citation7,Citation10,Citation11 Disruption of tight junctions between vascular endothelial cells is a critical process in the development of DME. In the healthy retina, water and solute flux is actively controlled to maintain an effective osmotic gradient.Citation11,Citation12 Diabetes-induced retinal vascular inflammation critically modifies these processes, leading to BRB breakdown, extravasation of plasma proteins, and tissue edema. Formation of edema is often perpetuated by coexisting pathologies, such as dyslipidemia and hypertension, which has both pressure and inflammatory contributions.
DME displays features characteristic of a chronic, low-grade, local inflammatory response.Citation10 Vitreous fluid from patients with DME shows evidence of active inflammation, containing elevated levels of pro-inflammatory cytokines (tumor necrosis factor-α [TNF-α], interleukin [IL] 1β and IL-6, and high-mobility group box-1 protein [HMGB1]), chemokines (monocyte chemotactic protein 1 [MCP-1], RANTES [CCL5], IL-8, interferon gamma-induced protein 10 [CXCL10], and stromal cell-derived factor 1 [CXCL12]), angiogenic factors (VEGF and platelet-derived growth factor), and adhesion molecules (intercellular adhesion molecule 1 [ICAM-1] and vascular cell adhesion molecule 1) ().Citation13–Citation19 Levels of anti-inflammatory proteins, such as pigment epithelium-derived factor, are concurrently reduced.Citation14 Activated microglia play an important role in early retinal inflammatory responses through the release of TNF-α, while local inflammation directs the recruitment and irreversible attachment of circulating leukocytes to the retinal vascular endothelium (leukostasis), providing another important source of pro-inflammatory mediators.Citation20–Citation22 These elevations in ocular levels of inflammatory mediators do not correlate with plasma levels, indicating that the inflammation is locally driven,Citation15,Citation23 and this is further supported by evidence of enhanced pro-inflammatory gene transcription in DME-affected eyes.Citation24
Table 1 Key inflammatory mediators driving BRB breakdown in diabetic macular edema
Intravascular and extravasated neutrophils perpetuate local inflammation by inciting microvascular damage and the release of stored mediators, and additionally have the potential to cause capillary occlusion.Citation20,Citation22,Citation25 Leukostasis is temporally and spatially linked to vascular leakage in murine models of diabetes.Citation22 Neutrophils are also prominent producers of reactive oxygen species, which are thought to be important in regulating vascular permeability.Citation6,Citation13,Citation26
Breakdown of the BRB and enhancement of vascular permeability in response to pro-inflammatory factors (most notably VEGF, TNF-α, ICAM-1, MCP-1, and IL-1β)Citation27,Citation28 and reactive oxygen speciesCitation29 are mediated through disassembly of tight junction proteins (occludins and cadherins) at intercellular tight junctionsCitation30–Citation32 and adherens junctionsCitation33 on vascular endothelial cells and retinal pigment epithelial cells.Citation30,Citation31 BRB breakdown can also be caused by cytokine-induced vascular cell death and by leukocyte-mediated vascular occlusion.Citation22
Although a number of anti-inflammatory therapies significantly inhibit the development of DME, inhibition of specific mediators has been largely unsuccessful.Citation13,Citation23 This is likely because of the redundant nature of inflammation and suggests that a broader dampening of the immune response might offer the best means of restoring and protecting vision.
Mechanism of action of intraocular corticosteroids in DME
The ocular corticosteroids dexamethasone, triamcinolone acetonide, and fluocinolone acetonide are potent and selective agonists at the glucocorticoid receptor, of which multiple isoforms are expressed in ocular tissues.Citation34 The resulting steroid–receptor complex translocates from the cell cytoplasm to the nucleus, where it brings about induction/repression of gene transcription, mRNA, and protein synthesis.Citation35,Citation36 In addition to these nuclear events, the steroid–receptor complex can trigger signal transduction events within the cytosol,Citation35 such as the release of annexin-1,Citation37 a modulator of leukocyte trafficking.Citation38 In contrast to the nuclear actions of glucocorticoids, these “non-genomic” effects are rapid, since they are not mediated through mRNA/protein synthesis.
In DME, corticosteroids stabilize the existing retinal vasculature and are antiangiogenic, directly suppressing the production of paracrine angiogenic factors, including VEGF, and reducing the formation of new blood vessels.Citation12,Citation39 Through repression of key pro-inflammatory transcription factors, such as nuclear factor-kappa B (NFκB) and activator protein 1, the pro-inflammatory feedback loop established in macular edema is disrupted.Citation13,Citation23 Corticosteroids inhibit phospholipase A2,Citation12 which is upregulated in the retinal microvasculature of the streptozotocin-induced diabetic ratCitation40,Citation41 and is implicated in retinal VEGF, ICAM-1, and TNF-α expression and retinal edema formation.Citation41,Citation42 Corticosteroids also induce expression of several anti-inflammatory proteins, including IL-10, adenosine, and IκBα, the natural inhibitor of NFκB,Citation35 actively dampening the reaction. Intravitreal dexamethasone has been shown to reduce retinal leukostasis and vascular endothelial ICAM-1 expression in the diabetic rat model.Citation43
At the BRB, corticosteroids act to maintain tight junction integrity by promoting tight junction protein expression and translocation to the endothelial/epithelial cell border,Citation28 and by protecting against oxidative stress-induced disruption of tight junction proteins in retinal pigment epithelial cells.Citation44 In addition to reducing retinal vascular permeability, corticosteroids also promote retinal fluid clearance through their effects on transcellular aquaporin-4 (AQP4) and potassium channels, the two main channels controlling retinal fluid movement on retinal Müller cells.Citation45,Citation46
The commonly used ocular corticosteroids, dexamethasone, triamcinolone acetonide, and fluocinolone acetonide, differ in their glucocorticoid receptor-binding affinity (dexamethasone > triamcinolone acetonide > fluocinolone acetonide) and lipophilicity (triamcinolone acetonide > fluocinolone acetonide > dexamethasone),Citation34 which could potentially translate into clinically important differences in ocular activity.
Barriers to intraocular delivery of corticosteroids
The principal challenge in pharmacotherapy of retinal disease is how to achieve effective and sustained intraretinal drug concentrations while minimizing unwanted drug effects on other ocular structures. Ocular penetration of systemically administered drugs (particularly large and/or hydrophilic molecules) is restricted by the BRB, which comprises the tight junctions of the retinal vascular endothelium (inner BRB) and the retinal pigment epithelium (outer BRB). For those drugs that do cross the BRB (small lipophilic molecules), the diluting effect of blood volume requires the use of large systemic doses, with the attendant risk of systemic adverse effects, while the rapid flow rate in the choroidal and retinal circulation limits drug exposure time.
The topically applied drug has to diffuse through multiple ocular tissues to reach the posterior segment of the eye.Citation47 Ocular surface tear mechanisms are a major factor limiting initial drug exposure, while any drug that does manage to penetrate the corneal/conjunctival epithelia and sclera is liable to be removed by subconjunctival–episcleral blood and lymph flow, the choroidal circulation, and the transcellular xenobiotic efflux transporters of the retinal pigment epithelium.Citation48 Consequently, topically administered ocular drugs show extremely low intravitreal bioavailability, typically of the order of <0.001%.Citation49
Likewise, periocular administration using the trans-scleral absorption pathway (subconjunctival, sub-Tenon’s, or retrobulbar injection) encounters multiple anatomic barriers (episclera, sclera, choroid, Bruch’s membrane, and retinal pigment epithelium) to drug delivery to the posterior eye. Moreover, trans-scleral clearance mechanisms (subconjunctival/episcleral lymphatics and blood flow, and choroidal blood flow) and outward-directed clearance flow from the vitreous humor (the posterior transretinal elimination pathway) further restrict drug penetration into target tissues of the posterior segment.Citation50 Collectively, these factors result in low intravitreal bioavailability (typically 0.01%–0.1%) for drugs administered via the periocular route.Citation48
Intravitreal drug injection through the pars plana has the advantage of bypassing the BRB and achieving maximal intravitreal bioavailability.Citation48 However, as a directly invasive technique, intravitreal injection carries risk of procedure-related complications (notably IOP elevation, endophthalmitis, and retinal hemorrhage, tear, or detachment). Rates of endophthalmitis and retinal detachment are estimated at 0.2% and 0.05%, respectively, per intravitreal injection.Citation51 Moreover, the duration of action of intravitreally administered drugs is limited by the presence of drug clearance mechanisms, namely the posterior transretinal and anterior aqueous humor elimination pathways and the efflux transporters on the retinal pigment epithelium.Citation48 For the commonly used ocular corticosteroids (dexamethasone, triamcinolone acetonide, and fluocinolone acetonide), the intravitreal half-life of the solubilized drug fraction is 2–3 hours in monkey and rabbit eyes.Citation34,Citation52 Accordingly, for treatment of retinal disorders, frequent intravitreal injections of soluble corticosteroids would be required, placing considerable treatment burden on the patient, and also increasing the likelihood of procedure-related complications.
In order to prolong drug retention in the vitreous humor, several sustained-release systems have been developed, including injectable drug suspensions and biodegradable and non-biodegradable intravitreal implants. Biodegradable nanocarrier systems (liposomes, nanoparticles, nanocrystals, and nanoemulsions) are currently under development, and may have future application in the treatment of posterior eye disease.Citation53 In addition to Ozurdex® (Allergan, Inc.; dexamethasone biodegradable implant), other sustained-release corticosteroid systems that are used intravitreally include Kenalog® (Bristol-Myers Squibb, Princeton, NJ, USA; triamcinolone acetonide suspension), Trivaris® (Allergan, Inc.; triamcinolone acetonide suspension), Triesence® (Alcon, Fort Worth, TX, USA; triamcinolone acetonide suspension), Retisert® (Bausch & Lomb Inc., Rochester, NY, USA; fluocinolone acetonide non-biodegradable implant), and Iluvien® (Alimera Sciences, Inc., Alpharetta, GA, USA; fluocinolone acetonide non-biodegradable implant). Of these sustained-release corticosteroid systems, Ozurdex® and Iluvien® are currently approved for treatment of DME (). Factors that can influence drug release include the physicochemical characteristics of the implant (eg, drug–polymer interactions), the solubility of the drug in the vitreous humor, and the proximity of the implant to the primary elimination pathway.Citation54 Posterior vitreous implant placement optimizes drug delivery to the retina and reduces drug exposure in the lens and trabecular meshwork, which are tissues associated with adverse ocular effects of corticosteroids (subcapsular cataract formation and IOP elevation).Citation34
Table 2 Comparative efficacy and safety of dexamethasone and fluocinolone acetonide intravitreal implants in diabetic macular edema
Dexamethasone intravitreal drug delivery system
Dexamethasone intravitreal implant, containing micronized preservative-free dexamethasone 0.7 mg in a biodegradable copolymer of polylactic-co-glycolic acid (which eventually breaks down into carbon dioxide and water), is designed to deliver drug to the retina over a period of up to 6 months after intravitreal injection. By avoiding the peak vitreous drug concentrations produced by intermittent bolus corticosteroid injections and the need for frequent repeat injections, the implant may potentially reduce the risk of unwanted steroid-associated ocular effects (cataract formation, IOP elevation, and glaucoma) and injection-related complications (lens injury, retinal detachment, and infectious endophthalmitis). The insertion procedure, which is performed in the office under local anesthesia, involves placement of the rod-shaped implant (6 mm in length and 0.46 mm in diameter) in the vitreous cavity via pars plana injection with a single-use applicator and 22-gauge needle. To avoid vitreal reflux through the scleral puncture, a tunneled injection technique is used to create an angled intrascleral injection tract. Despite the relatively large diameter of the injector needle, the level of pain associated with the insertion procedure is not appreciably different from that produced by intravitreal anti-VEGF treatment, as administered with a 28- to 30-gauge needle.Citation55 Since the implant is biodegradable, subsequent implant(s) can be inserted without the need for surgical removal of the existing implant.
High-speed, real-time photography of the injection procedure reveals that the impact velocity of the dexamethasone intravitreal implant, delivered using the applicator, is insufficient to cause retinal damage.Citation56 Reported complications associated with the injection procedure include isolated cases of accidental lens injectionCitation57–Citation59 and splitting or fracture of the implant either during or immediately after intravitreal injection.Citation60–Citation63 Inadvertent lens injection is an extremely rare event, but if it occurs, it can be managed successfully with prompt surgical extraction of the lens to avoid possible IOP elevation, and implantation of an intraocular lens.Citation57–Citation59 Implant fracture can result from misalignment of the implant within the applicator.Citation61 Although the fragmented implant does not appear to cause more intraocular complications than the intact implant, monitoring for unexpected complications is recommended in such cases.Citation60
Complications that have been reported with the implant in situ include isolated cases of migration into the anterior chamber,Citation64–Citation69 potentially leading to development of corneal edema.Citation65,Citation66 Aphakia and pseudophakia in association with imperfect zonular/posterior capsular integrity are risk factors for anterior chamber migration.Citation65,Citation69 Accordingly, use of dexamethasone intravitreal implant should be avoided in eyes with aphakia, an anterior chamber intraocular lens, or rupture of the posterior lens capsule.
Pharmacokinetic profile of dexamethasone intravitreal implant
Pharmacokinetic studies in nonhuman primate (monkey) and rabbit eyes indicate that intraocular dexamethasone concentrations peak at 2–6 weeks after injection of the dexamethasone intravitreal implant, and that higher levels are achieved in the retina than in the vitreous.Citation70,Citation71 In the monkey eye, dexamethasone intravitreal implant 0.7 mg shows a biphasic release pattern, with vitreal and retinal dexamethasone concentrations displaying a high plateau (vitreous, ~100–1,000 µg/mL; retinal, ~100–1,000 µg/g) during the first 2 months after implant insertion, declining sharply during the third month, and leveling off at a considerably lower plateau (vitreous, ~0.1–1 ng/mL; retinal, ~0.1–1 ng/g) for the next 3–4 months, reaching nondetectable levels after 7–8 months.Citation70 Assuming that the steady-state concentrations of dexamethasone achieved in the monkey eye approximate to those in the human eye, these findings would suggest that dexamethasone intravitreal implant achieves higher and more steady vitreal drug concentrations during the initial release phase than subconjunctival,Citation72 periocular,Citation73 topical,Citation74 or oralCitation75 dexamethasone administration in human eyes.
Vitrectomy is known to accelerate the intraocular clearance of many drugs, including triamcinolone acetonide,Citation76 and differences in drug disposition between nonvitrectomized and vitrectomized eyes may potentially influence the effectiveness of treatment. In contrast, a pharmacokinetic study in rabbit eyes indicated that vitreous and retinal dexamethasone concentration-vs-time profiles following injection of dexamethasone intravitreal implant 0.7 mg were similar in nonvitrectomized and vitrectomized eyes.Citation71
Systemic drug exposure from the dexamethasone intravitreal implant (0.35 mg or 0.7 mg) appears to be negligible in humans, and plasma dexamethasone concentrations are generally below the lower limit of quantification (50 pg/mL). Accordingly, the potential for systemic corticosteroid-related adverse effects with dexamethasone intravitreal implant is minimal.
Efficacy of dexamethasone intravitreal implant in DME
Several Phase II and Phase III studies have demonstrated the efficacy of dexamethasone intravitreal implant (0.7 mg or 0.35 mg) in improving visual and retinal anatomic outcomes in patients with DME (). A randomized, single-masked, 6-month, Phase II study involving incisional vitreous placement of the dexamethasone implant in patients with persistent DME (n=171) provided evidence of a possible dose–response relationship, with more patients achieving a ≥10-letter or ≥15-letter gain in best-corrected visual acuity (BCVA) with dexamethasone implant 0.7 mg than with dexamethasone implant 0.35 mg at 2 months, 3 months, and 6 months; however, the differences between the active treatment groups were not statistically significant.Citation77 Significant improvements in macular thickness and retinal capillary leakage were noted at 6 months in the dexamethasone implant-treated patients compared with nontreated controls; as with the visual acuity findings, these anatomic responses tended to be more pronounced with the 0.7 mg than with the 0.35 mg dose. In a subsequent analysis of data from this study, dexamethasone intravitreal implant was found to display similar efficacy in focal, cystoid, and diffuse DME.Citation78
Table 3 Summary of Phase II and Phase III clinical trials of dexamethasone intravitreal implant in diabetic macular edema
Evidence of accelerated clearance of corticosteroids from vitrectomized compared with nonvitrectomized eyesCitation76,Citation79 might suggest that the clinical benefits of dexamethasone intravitreal implant would be reduced by vitrectomy. The CHAMPLAIN study, a multicenter, open-label, noncomparative, 6-month, Phase II investigation of the efficacy and safety of dexamethasone intravitreal implant 0.7 mg in patients with treatment-resistant DME and prior pars plana vitrectomy (n=55) reported sustained improvements in visual and anatomic outcomes in this difficult-to-treat patient group.Citation80 Improvements from baseline in BCVA and central subfield retinal thickness peaked at 2–3 months postinjection and persisted, albeit at a diminished level, until the end of the study.Citation80
A randomized, double-masked, sham-controlled, 12-month, Phase II study of dexamethasone implant 0.7 mg in combination with laser therapy in patients with diffuse DME (n=253) found that dexamethasone implant plus laser therapy produced greater improvements in BCVA, macular thickness, and capillary leakage than laser therapy alone, although in most cases the treatment advantage was not sustained for the full 12 months.Citation81 Patients received dexamethasone implant at baseline and laser therapy at month 1, and could receive up to three additional laser treatments and one additional dexamethasone implant treatment as needed. Significantly more patients showed a ≥10-letter gain in BCVA with dexamethasone implant 0.7 mg plus laser therapy than with laser therapy alone at 9 months (31.7% vs 17.3%) but not at 12 months (27.8% vs 23.6%). Analysis of the change from baseline in BCVA over the 12-month study period indicated significantly greater improvement with dexamethasone implant plus laser than with laser alone. Central subfield retinal thickness was reduced to a significantly greater extent in the dexamethasone implant plus laser group than in the laser-alone group during the first 4 months, while vascular leakage showed a significantly larger reduction in the dexamethasone implant plus laser group than in the laser-alone group over the full 12 months.
Two large, multicenter, randomized, Phase III clinical trials to evaluate the long-term safety and efficacy of dexamethasone implant have recently been completed in patients with DME.Citation82 Patients with a BCVA of 34–68 letters (20/200–20/50 Snellen equivalent) and central subfield retinal thickness ≥300 µm were randomized to treatment with dexamethasone implant 0.7 mg or 0.35 mg, or sham procedure and followed for 3 years. As the trials were of identical design, the results were pooled for analysis (total of 1,048 patients).Citation82 Dexamethasone implant 0.7 mg and 0.35 mg, administered at ≥6-month intervals over 3 years, provided robust long-term improvement in visual acuity and macular edema, with significantly more patients showing a ≥15-letter gain in BCVA at the end of the study with dexamethasone implant 0.7 mg and 0.35 mg than with sham injection (22.2% and 18.4% vs 12.0%; P≤0.018). Although the changes in visual acuity were confounded by development and/or progression of cataract in a substantial proportion of phakic eyes after the first year, significant overall improvement in BCVA over the 3-year treatment period was obtained with dexamethasone implant.
Anatomical assessments, using optical coherence tomography, fundus photography, and fluorescein angiography, indicated that dexamethasone implant 0.7 mg and 0.35 mg produced rapid and sustained reductions in measures of macular edema over the 3-year treatment period, and slowed retinopathy progression.Citation83 On completion of 3 years of treatment with dexamethasone implant 0.7 mg and 0.35 mg, significant reductions (vs sham procedure) were noted in central subfield retinal thickness (mean, −111.6 µm and −107.9 µm vs −41.9 µm), macular volume (mean, −1.06 mm3 and −1.14 mm3 vs −0.31 mm3), and area of central retinal thickening (mean, −2.75 and −2.93 vs −1.49 disk areas). Patients treated with dexamethasone implant 0.7 mg and 0.35 mg were significantly more likely to show an improvement in clinically significant macular edema after 3 years than sham-treated controls (20.4% and 22.4% vs 12.4%). In addition, treatment with dexamethasone implant 0.7 mg slowed the progression of diabetic retinopathy, delaying by approximately 12 months the onset of two-step progression in Diabetic Retinopathy Disease Severity Score.Citation84
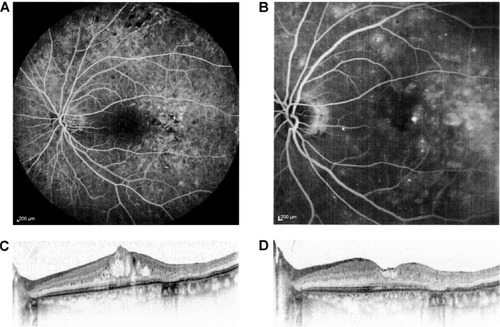
Small-scale, short-term exploratory studies and retrospective case studies suggest that dexamethasone intravitreal implant 0.7 mg is of potential benefit in persistent, treatment-refractory DME, including cystoid macular edema ( and ). A prospective study in 15 patients (16 eyes) with chronic DME nonresponsive to bevacizumab (as indicated by the absence of clinically significant reduction in CRT after at least three monthly bevacizumab injections) reported significant improvements in BCVA and central subfield retinal thickness for up to 3 months after insertion of dexamethasone intravitreal implant.Citation85 A retrospective study assessing the effects of dexamethasone intravitreal implant 0.7 mg in 33 patients (37 eyes) with prolonged, treatment-refractory cystoid macular edema of various etiologies reported significant improvements in BCVA (mean 2–3 Early Treatment Diabetic Retinopathy Study lines from baseline) and central macular thickness (46% decrease) during approximately 6 months of follow-up in the subset of patients (14 eyes) with DME.Citation86 In a retrospective review of medical records of 58 patients with chronic DME that was refractory to laser and intravitreal anti-VEGF and/or intravitreal steroid therapy, dexamethasone intravitreal implant produced significant improvement in BCVA and foveal thickness for up to 6 months post-insertion.Citation87 Favorable results have also been reported with dexamethasone intravitreal implant in small cohorts of patients with persistent DME.Citation88,Citation89
Figure 1 A 64-year-old male diagnosed with diabetic macular edema in the right eye.
Abbreviation: BCVA, best-corrected visual acuity.
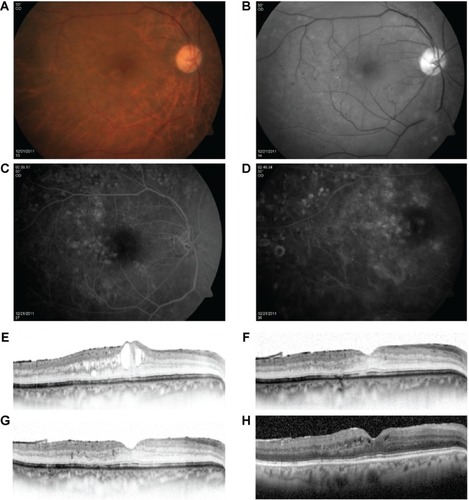
Figure 2 A 62-year-old patient with cystoid macular edema in the left eye previously treated with three monthly injections of intravitreal bevacizumab.
Abbreviation: BCVA, best-corrected visual acuity.
Tolerability of dexamethasone intravitreal implant
Common complications of ocular corticosteroid therapy are IOP elevation and cataract formation/progression. In the Phase III registration studies of dexamethasone intravitreal implant 0.7 mg and 0.35 mg in the treatment of DME,Citation82 29.7% of patients treated with dexamethasone implant (compared with 4.3% of sham-treated patients) showed clinically significant IOP elevation (IOP ≥25 mmHg). In most cases, this was managed with ocular hypotensive medication or observation, and only seven patients (1.0%) required glaucoma incisional surgery (three patients, 0.4%) or IOP-lowering laser therapy (four patients, 0.6%). The increase in IOP was generally transient, reaching a peak at approximately 6 weeks after each dexamethasone implant injection, with IOP returning to baseline levels within 6 months postinjection. The incidence and extent of IOP elevation after each dexa methasone implant injection did not change appreciably over the 3-year treatment period. Among phakic patients, 66.0% experienced a cataract-related adverse effect (cataract, cataract cortical, cataract nuclear, cataract subcapsular, or lenticular opacities) during treatment with dexamethasone implant (compared with 20.4% of sham-treated patients), and 55.8% of dexamethasone implant-treated patients required cataract surgery during the study (compared with 7.2% of sham-treated patients). The incidence of cataract-related adverse effects increased during the second and third years of treatment with dexamethasone implant, and most cataract surgery procedures occurred during this period.
In addition to elevated IOP and cataract, the most frequent adverse events reported with dexamethasone intravitreal implant in the Phase III studies in DME included conjunctival hemorrhage (23.5%), vitreous hemorrhage (10.0%), macular fibrosis (8.3%), conjunctival hyperemia (7.2%), eye pain (6.1%), vitreous detachment (5.8%), and dry eye (5.8%)Citation82 (). Injection-related adverse effects, such as retinal tear, retinal detachment, vitreous loss, and endophthalmitis, occurred in <2% of patients.
Table 4 Most frequently reported adverse events in Phase III studies of dexamethasone intravitreal implant in the treatment of diabetic macular edema
Place of dexamethasone intravitreal implant in management of DME
In comparison to the other sustained-release corticosteroid delivery systems, dexamethasone implant has the advantage of ease of administration, and the implant injection can be performed in the outpatient setting, while the biodegradable polymer matrix allows re-treatment without the need for surgical removal of the existing implant. The major challenge with intravitreal corticosteroid implants is their high rate of intraocular complications, notably IOP elevation and cataract. Dexamethasone is less lipophilic than fluocino-lone acetonide and triamcinolone acetonide and shows less sequestration in the lens and trabecular meshwork,Citation90 and hence has potentially lower risk of causing IOP elevation and cataract; however, this has yet to be confirmed in head-to-head comparisons of dexamethasone with other intravitreal corticosteroid implants.
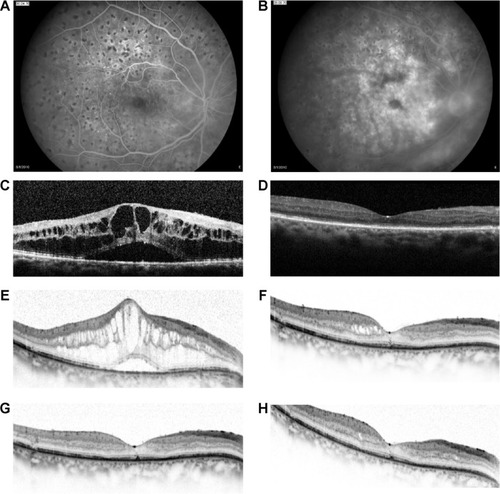
Dexamethasone intravitreal implant has a shorter duration of action than fluocinolone acetonide implant, with macular edema typically reverting to pretreatment levels approximately 5–6 months, and in some cases, as early as 3 months, after injection (). Despite the temporary morphological effect, macular edema usually responds to re-treatment. Repeat injections performed at approximately 6-month intervals produce consistent reductions in macular thickness, with no apparent attenuation of response over time ().
Figure 3 A 72-year-old patient with diabetic macular edema in the right eye previously treated with three monthly injections of intravitreal bevacizumab.
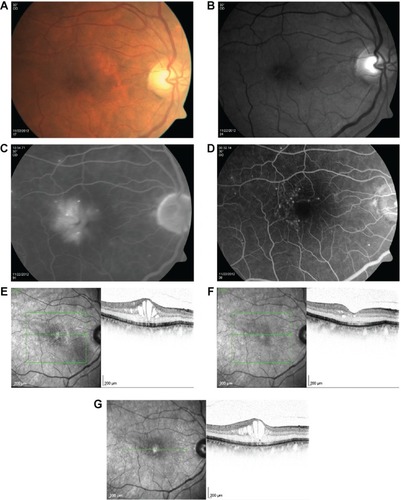
Figure 4 A 65-year-old female with regressed proliferative diabetic retinopathy in the right eye previously treated with three monthly injections of intravitreal bevacizumab.
Abbreviation: BCVA, best-corrected visual acuity.
In comparison to intravitreal anti-VEGF agents, dexamethasone intravitreal implant requires less frequent repeat injection, which might be anticipated to result in fewer injection-related complications, lower treatment costs, and improved patient compliance. Although prospective head-to-head comparisons have yet to be conducted with anti-VEGF agents, dexamethasone intravitreal implant (in common with other injectable corticosteroid implants) is unlikely to replace anti-VEGF agents as first-line therapy for DME because of the risk of steroid-related intraocular complications (notably cataract, IOP elevation, and glaucoma). However, because of its favorable pharmacokinetic properties, dexamethasone intravitreal implant may potentially be an appropriate first-line therapy for DME with foveal involvement in vitrectomized eyes. In addition, it appears to be a suitable treatment option for persistent DME and DME that is unresponsive to anti-VEGF or laser therapy.
Use of dexamethasone intravitreal implant is contraindicated in the following cases: patients with active or suspected ocular or periocular infections, including most viral diseases of the cornea and conjunctiva (eg, dendritic keratitis, vaccinia, and varicella), mycobacterial infections, and fungal diseases; glaucoma patients with a cup-to-disk ratio >0.8; patients with a torn or ruptured posterior lens capsule; and patients with known hypersensitivity to any component of the implant.Citation91 In addition, use of dexamethasone intravitreal implant (in common with other corticosteroids) is not recommended in patients with a history of ocular herpes simplex because of the risk of viral reactivation.Citation91 Similarly, it should be borne in mind that the use of dexamethasone intravitreal implant may increase the risk of secondary ocular infections.
Further insight into the role of dexamethasone intravitreal implant in the treatment of DME, and its optimal schedule of administration, is expected from ongoing/planned clinical trials that are variously exploring its adjunctive use with anti-VEGF agents (ClinicalTrials.gov identifier: NCT01309451), in the post-vitrectomy setting (ClinicalTrials.gov identifiers: NCT01788475 and NCT01613716), and in anti-VEGF-refractory disease (ClinicalTrials.gov identifiers: NCT01571232, NCT01790685, and NCT 01951066), as well as the effects of a shortened (5-month) re-treatment interval in DME (NCT01492400).
Acknowledgments
Writing and editorial assistance in preparation of this manuscript was provided to the authors by Andrew Fitton, PhD, of Evidence Scientific Solutions, and was funded by Allergan, Inc.
Disclosure
PUD reports the following: consultancy fees and research grants – Allergan. FB reports the following: consultancy fees/honoraria and lecture/speakers’ bureaux fees – Allergan, Novartis, Farmilia-Thea, Bayer, Pfizer, Alcon, Bausch and Lomb, Genentech, Alimera Sciences, Sanofi-Aventis, ThromboGenics, Hoffmann-La Roche, and Novagali Pharma. AL reports the following: consultancy fees – Allergan, Alcon, Bayer, Notal Vision, Novartis, and Teva.
References
- KleinRKleinBEMossSEDavisMDDeMetsDLThe Wisconsin epidemiologic study of diabetic retinopathy. IV. Diabetic macular edemaOphthalmology19849112146414746521986
- AntcliffRJMarshallJThe pathogenesis of edema in diabetic maculopathySemin Ophthalmol199914422323210758223
- BhagatNGrigorianRATutelaAZarbinMADiabetic macular edema: pathogenesis and treatmentSurv Ophthalmol200954113219171208
- YauJWRogersSLKawasakiRMeta-Analysis for Eye Disease (META-EYE) Study GroupGlobal prevalence and major risk factors of diabetic retinopathyDiabetes Care201235355656422301125
- FordJALoisNRoylePClarCShyangdanDWaughNCurrent treatments in diabetic macular oedema: systematic review and meta-analysisBMJ Open201333e002269
- ZhangWLiuHAl-ShabraweyMCaldwellRWCaldwellRBInflammation and diabetic retinal microvascular complicationsJ Cardiovasc Dis Res2011229610321814413
- EhrlichRHarrisACiullaTAKheradiyaNWinstonDMWirostkoBDiabetic macular oedema: physical, physiological and molecular factors contribute to this pathological processActa Ophthalmol201088327929120222885
- The Diabetes Control and Complications Trial Research GroupThe effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitusN Engl J Med1993329149779868366922
- UK Prospective Diabetes Study (UKPDS) GroupIntensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33)Lancet199835291318378539742976
- AntonettiDABarberAJBronsonSKJDRF Diabetic Retinopathy Center GroupDiabetic retinopathy: seeing beyond glucose-induced microvascular diseaseDiabetes20065592401241116936187
- SchollSAugustinALoewensteinARizzoSKuppermanBGeneral pathophysiology of macular edemaEur J Ophthalmol201121suppl 6S10S1923264324
- StewartMWCorticosteroid use for diabetic macular edema: old fad or new trend?Curr Diab Rep201212436437522581206
- ZhangWLiuHRojasMCaldwellRWCaldwellRBAnti-inflammatory therapy for diabetic retinopathyImmunotherapy20113560962821554091
- FunatsuHNomaHMimuraTEguchiSHoriSAssociation of vitreous inflammatory factors with diabetic macular edemaOphthalmology20091161737919118698
- YoshimuraTSonodaKHSugaharaMComprehensive analysis of inflammatory immune mediators in vitreoretinal diseasesPLoS One2009412e815819997642
- El-AsrarAMNawazMIKangaveDHigh-mobility group box-1 and biomarkers of inflammation in the vitreous from patients with proliferative diabetic retinopathyMol Vis2011171829183821850157
- Adamiec-MroczekJOficjalska-MlyńczakJMisiuk-HojłoMRoles of endothelin-1 and selected proinflammatory cytokines in the pathogenesis of proliferative diabetic retinopathy: analysis of vitreous samplesCytokine201049326927420015663
- MaierRWegerMHaller-SchoberEMMultiplex bead analysis of vitreous and serum concentrations of inflammatory and proangiogenic factors in diabetic patientsMol Vis20081463764318385799
- LeeWJKangMHSeongMChoHYComparison of aqueous concentrations of angiogenic and inflammatory cytokines in diabetic macular oedema and macular oedema due to branch retinal vein occlusionBr J Ophthalmol201296111426143022930681
- MiyamotoKOguraYPathogenetic potential of leukocytes in diabetic retinopathySemin Ophthalmol199914423323910758224
- GardnerTWAntonettiDABarberAJLaNoueKFLevisonSWDiabetic retinopathy: more than meets the eyeSurv Ophthalmol200247suppl 2S253S26212507627
- JoussenAMPoulakiVLeMLA central role for inflammation in the pathogenesis of diabetic retinopathyFASEB J200418121450145215231732
- TangJKernTSInflammation in diabetic retinopathyProg Retin Eye Res201130534335821635964
- BrucklacherRMPatelKMVanGuilderHDWhole genome assessment of the retinal response to diabetes reveals a progressive neurovascular inflammatory responseBMC Med Genomics200812618554398
- JoussenAMPoulakiVMitsiadesNSuppression of Fas-FasL-induced endothelial cell apoptosis prevents diabetic blood-retinal barrier breakdown in a model of streptozotocin-induced diabetesFASEB J2003171767812475915
- RojasMZhangWXuZRequirement of NOX2 expression in both retina and bone marrow for diabetes-induced retinal vascular injuryPLoS One2013812e8435724358357
- DeisslerHLDeisslerHLangGKLangGEVEGF but not PlGF disturbs the barrier of retinal endothelial cellsExp Eye Res201311516217123891860
- AveleiraCALinCMAbcouwerSFAmbrosioAFAntonettiDATNF-alpha signals through PKCzeta/NF-kappaB to alter the tight junction complex and increase retinal endothelial cell permeabilityDiabetes201059112872288220693346
- LealECManivannanAHosoyaKInducible nitric oxide synthase isoform is a key mediator of leukostasis and blood-retinal barrier breakdown in diabetic retinopathyInvest Ophthalmol Vis Sci200748115257526517962481
- AntonettiDALiethEBarberAJGardnerTWMolecular mechanisms of vascular permeability in diabetic retinopathySemin Ophthalmol199914424024810758225
- BarberAJAntonettiDAMapping the blood vessels with paracellular permeability in the retinas of diabetic ratsInvest Ophthalmol Vis Sci200344125410541614638745
- BoltonSJAnthonyDCPerryVHLoss of the tight junction proteins occludin and zonula occludens-1 from cerebral vascular endothelium during neutrophil-induced blood–brain barrier breakdown in vivoNeuroscience1998864124512579697130
- RangasamySMcGuirePGDasADiabetic retinopathy and inflammation: novel therapeutic targetsMiddle East Afr J Ophthalmol2012191525922346115
- EdelmanJLDifferentiating intraocular glucocorticoidsOphthalmologica2010224suppl 1253020714178
- ClarkARBelvisiMGMaps and legends: the quest for dissociated ligands of the glucocorticoid receptorPharmacol Ther20121341546722212616
- BusilloJMCidlowskiJAThe five Rs of glucocorticoid action during inflammation: ready, reinforce, repress, resolve, and restoreTrends Endocrinol Metab201324310911923312823
- SolitoEMullaAMorrisJFChristianHCFlowerRJBuckinghamJCDexamethasone induces rapid serine-phosphorylation and membrane translocation of annexin 1 in a human folliculostellate cell line via a novel nongenomic mechanism involving the glucocorticoid receptor, protein kinase C, phosphatidylinositol 3-kinase, and mitogen-activated protein kinaseEndocrinology200314441164117412639897
- DalliJNorlingLVRenshawDCooperDLeungKYPerrettiMAnnexin 1 mediates the rapid anti-inflammatory effects of neutrophil-derived microparticlesBlood200811262512251918594025
- LogieJJAliSMarshallKMHeckMMWalkerBRHadokePWGlucocorticoid-mediated inhibition of angiogenic changes in human endothelial cells is not caused by reductions in cell proliferation or migrationPLoS One2010512e1447621217824
- GongYJinXWangQSThe involvement of high mobility group 1 cytokine and phospholipases A2 in diabetic retinopathyLipid Health Dis201413156
- LupoGMottaCGiurdanellaGRole of phospholipases A2 in diabetic retinopathy: in vitro and in vivo studiesBiochem Pharmacol201386111603161324076420
- PannickeTIandievIWurmADiabetes alters osmotic swelling characteristics and membrane conductance of glial cells in rat retinaDiabetes200655363363916505225
- TamuraHMiyamotoKKiryuJIntravitreal injection of corticosteroid attenuates leukostasis and vascular leakage in experimental diabetic retinaInvest Ophthalmol Vis Sci20054641440144415790913
- MiuraYRoiderJTriamcinolone acetonide prevents oxidative stress-induced tight junction disruption of retinal pigment epithelial cellsGraefes Arch Clin Exp Ophthalmol2009247564164919189116
- ReichenbachAWurmAPannickeTIandievIWiedemannPBringmannAMuller cells as players in retinal degeneration and edemaGraefes Arch Clinical Exp Ophthalmol2007245562763617219109
- ZhaoMBousquetEValamaneshFDifferential regulations of AQP4 and Kir4.1 by triamcinolone acetonide and dexamethasone in the healthy and inflamed retinaInvest Ophthalmol Vis Sci20115296340634721724913
- HughesPMOlejnikOChang-LinJEWilsonCGTopical and systemic drug delivery to the posterior segmentsAdv Drug Deliv Rev200557142010203216289435
- EdelhauserHFRowe-RendlemanCLRobinsonMROphthalmic drug delivery systems for the treatment of retinal diseases: basic research to clinical applicationsInvest Ophthalmol Vis Sci201051115403542020980702
- MauriceDMDrug delivery to the posterior segment from dropsSurv Ophthalmol200247suppl 1S41S5212204700
- KimSHLutzRJWangNSRobinsonMRTransport barriers in transscleral drug delivery for retinal diseasesOphthalmic Res200739524425417851264
- JagerRDAielloLPPatelSCCunninghamETJrRisks of intravitreous injection: a comprehensive reviewRetina200424567669815492621
- KwakHWD’AmicoDJEvaluation of the retinal toxicity and pharmacokinetics of dexamethasone after intravitreal injectionArch Ophthalmol199211022592661736876
- KaurIPKakkarSNanotherapy for posterior eye diseasesJ Control Release201419310011224862316
- YasukawaTOguraYTabataYKimuraHWiedemannPHondaYDrug delivery systems for vitreoretinal diseasesProg Retin Eye Res200423325328115177203
- MoisseievERegenbogenMRabinovitchTBarakALoewensteinAGoldsteinMEvaluation of pain during intravitreal Ozurdex injections vs intravitreal bevacizumab injectionsEye201428898098524924442
- MeyerCHKleinAAltenFRelease and velocity of micronized dexamethasone implants with an intravitreal drug delivery system: kinematic analysis with a high-speed cameraRetina201232102133214023060033
- BerarducciASianISLingRInadvertent dexamethasone implant injection into the lens body managementEur J Ophthalmol201424462062224519508
- Coca-RobinotJCasco-SilvaBArmada-MarescaFGarcia-MartinezJAccidental injections of dexamethasone intravitreal implant (Ozurdex) into the crystalline lensEur J Ophthalmol201424463363624519506
- FasceFBattaglia ParodiMKnutssonKAAccidental injection of dexamethasone intravitreal implant in the crystalline lensActa Ophthalmol2014924e330e33124373603
- AgrawalRFernandez-SanzGBalaSAddisonPKDesegmentation of Ozurdex implant in vitreous cavity: report of two casesBr J Ophthalmol201498796196324648417
- DonmezOParlakMYamanASaatciAOSplitting of a dexametha-sone implant (Ozurdex) following the injectionCase Rep Ophthalmol Med2013201324794923984139
- RoyRHegdeSSplit Ozurdex implant: a cautionCan J Ophthalmol2013481e15e1623419308
- RishiPMathurGRishiEFractured Ozurdex™ implant in the vitreous cavityInd J Ophthalmol2012604337338
- Wai Ch’ngSPadroniSBanerjeeSAnterior vitreous displacement of the intravitreal dexamethasone implant (Ozurdex)Eye201428223823924336298
- KhuranaRNAppaSNMcCannelCADexamethasone implant anterior chamber migration: risk factors, complications, and management strategiesOphthalmology20141211677123890421
- KishoreSASchaalSManagement of anterior chamber dislocation of dexamethasone implantOcul Immunol Inflamm2013211909123323589
- VelaJICrespiJAndreuDRepositioning of dexamethasone intravitreal implant (Ozurdex) migrated into the anterior chamberIntl Ophthalmol2012326583584
- BansalRBansalPKulkarniPGuptaVSharmaAGuptaAWandering Ozurdex(®) implantJ Ophthalmic Inflamm Infect2012211521960148
- MalclèsAJanin-ManificatHYhuelYAnterior chamber migration of intravitreal dexamethasone implant (Ozurdex®) in pseudophakic eyes: report of three casesJ Franc Ophtalmol2013364362367 French
- Chang-LinJEAttarMAcheampongAAPharmacokinetics and pharmacodynamics of a sustained-release dexamethasone intravitreal implantInvest Ophthalmol Vis Sci2011521808620702826
- Chang-LinJEBurkeJAPengQPharmacokinetics of a sustained-release dexamethasone intravitreal implant in vitrectomized and nonvit-rectomized eyesInvest Ophthalmol Vis Sci20115274605460921421864
- WeijtensOFeronEJSchoemakerRCHigh concentration of dexamethasone in aqueous and vitreous after subconjunctival injectionAm J Ophthalmol1999128219219710458175
- WeijtensOvan der SluijsFASchoemakerRCPeribulbar corticosteroid injection: vitreal and serum concentrations after dexamethasone disodium phosphate injectionAm J Ophthalmol199712333583639063245
- WeijtensOSchoemakerRCRomijnFPCohenAFLentjesEGvan MeursJCIntraocular penetration and systemic absorption after topical application of dexamethasone disodium phosphateOphthalmology2002109101887189112359610
- WeijtensOSchoemakerRCCohenAFDexamethasone concentration in vitreous and serum after oral administrationAm J Ophthalmol199812556736799625551
- ChinHSParkTSMoonYSOhJHDifference in clearance of intra-vitreal triamcinolone acetonide between vitrectomized and nonvitrec-tomized eyesRetina200525555656016077349
- HallerJAKuppermannBDBlumenkranzMSDexamethasone DDS Phase II Study GroupRandomized controlled trial of an intrav-itreous dexamethasone drug delivery system in patients with diabetic macular edemaArch Ophthalmol2010128328929620212197
- KuppermannBDChouCWeinbergDVWhitcupSMHallerJABlumenkranzMSIntravitreous dexamethasone effects on different patterns of diabetic macular edemaArch Ophthalmol2010128564264320212194
- BeerPMBakriSJSinghRJLiuWPetersGB3rdMillerMIntraocu-lar concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injectionOphthalmology2003110468168612689886
- BoyerDSFaberDGuptaSOzurdex CHAMPLAIN Study GroupDexamethasone intravitreal implant for treatment of diabetic macular edema in vitrectomized patientsRetina201131591592321487341
- CallananDGGuptaSBoyerDSOzurdex PLACID Study GroupDexamethasone intravitreal implant in combination with laser photocoagulation for the treatment of diffuse diabetic macular edemaOphthalmology201312091843185123706947
- BoyerDSYoonYHBelfortRJrThree-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edemaOphthalmology2014121101904191424907062
- DanisRPSaddaSCuiHLiX-YHashadYWhitcupSMAnatomic outcomes with dexamethasone intravitreal implant in diabetic macular edema: a pooled analysis of two randomized Phase III trialsARVO 2014 Annual MeetingMay 4–8, 2014Orlando, FL
- SaddaSDanisRPLiX-YCuiHHashadYWhitcupSMAnatomic effects of dexamethasone intravitreal implant in diabetic macular edema: pooled analysis of findings from two randomized Phase 3 studies32nd Annual Meeting of the American Society of Retina SpecialistsAugust 9–13, 2014San Diego
- LazicRLukicMBorasITreatment of anti-vascular endothelial growth factor-resistant diabetic macular edema with dexamethasone intravitreal implantRetina201434471972423975006
- SorkinNLoewensteinAHabot-WilnerZGoldsteinMIntravitreal dexamethasone implant in patients with persistent macular edema of variable etiologiesOphthalmologica20142322839124942067
- Dutra MedeirosMPostorinoMNavarroRGarcia-ArumiJMateoCCorcosteguiBDexamethasone intravitreal implant for treatment of patients with persistent diabetic macular edemaOphthalmologica2014231314114624356099
- PacellaEVestriARMuscellaRPreliminary results of an intra-vitreal dexamethasone implant (Ozurdex®) in patients with persistent diabetic macular edemaClin Ophthalmol201371423142823901252
- ZucchiattiILattanzioRQuerquesGIntravitreal dexamethasone implant in patients with persistent diabetic macular edemaOphthalmologica2012228211712222310491
- ThakurAKadamRKompellaUBTrabecular meshwork and lens partitioning of corticosteroids: implications for elevated intraocular pressure and cataractsArch Ophthalmol2011129791492021402977
- AnonOzurdex Prescribing Information2014 Available from: http://www.allergan.com/assets/pdf/ozurdex_pi.pdfAccessed March 27, 2015
- CampochiaroPABrownDMPearsonAFAME Study GroupSustained delivery fluocinolone acetonide vitreous inserts provide benefit for at least 3 years in patients with diabetic macular edemaOphthalmology2012119102125213222727177
