Abstract
To investigate which of two tunnel incision forms (frown versus straight) in sutureless manual small incision cataract surgery creates more corneal astigmatism. Sixty eyes of 60 patients who had consented to undergo cataract surgery and to partake in this study were followed from baseline through >12-week postoperative period. Values of preoperative and postoperative corneal astigmatism for the 60 eyes, measured with a Bausch and Lomb keratometer, were extracted from the patients’ cataract surgery records. Residual astigmatism was computed as the difference between preoperative and postoperative keratometry readings. Visual acuity was assessed during the preoperative period and at each postoperative visit with a Snellen chart at 6 m. Fifty eyes of 50 patients were successfully followed-up on. Overall, the mean residual astigmatism was 0.75±0.12 diopters. The differences in mean residual astigmatism between the two different incision groups were statistically significant (t [48]=6.33, P<0.05); frown incision group recorded 1.00±0.12 diopters, whereas the straight incision group recorded 0.50±0.12 diopters. No significant difference was observed between male and female groups (t [48]=0.24, P>0.05). Residual corneal astigmatism in the frown incision group was significantly higher than in the straight incision group. Fisher’s exact test did not reveal a significant association between incision forms and visual acuity during the entire postoperative period (P>0.05).
Introduction
Cataract is an eye condition in which the human crystalline lens becomes opaque and invariably affects vision.Citation1–Citation4 It mostly affects the aged, but young people may suffer from congenital forms of the condition.Citation1,Citation5,Citation6 The causes and risk factors for cataract are many and varied. Some of them include genetics, sex, race, metabolic diseases, trauma to the eyes, radiation, use of certain drugs, and lifestyle.Citation7,Citation8
It is common for ophthalmic clinicians to attempt to improve the vision of persons with early cataracts – either by the use of spectacle prescription and/or antiglare devices.Citation9 Sometimes, clinicians may also prescribe antioxidant-rich supplements and diets that are believed to retard the lens clouding process.Citation10,Citation11 In spite of these approaches, vision is often improved when cataract is ultimately removed by surgery and patients undergo subsequent visual rehabilitation.Citation3,Citation12,Citation13
Surgical techniques for cataract extraction have undergone major advancement – from intracapsular extraction to the present day phacoemulsification. Phacoemulsification offers desirable anatomical and functional results following cataract surgery. The technique is however not widely used in some parts of the developing world for reasons such as higher cost and expertise. The most widely used surgical technique for cataract extraction in third world countries is the sutureless manual small incision cataract surgery (MSICS). MSICS is reportedly able to offer good anatomical and functional results following cataract surgery. Presently, it remains the most cost-effective method for cataract extraction in developing countries.
However, visual outcome after MSICS and other forms of cataract surgery may rarely not be desirable. The reasons for a poor visual outcome after cataract surgery are indefinite. Some studies have implicated surgeon’s experience, existing ocular and systemic comorbidities of the patient, aging, and some refractive complications.Citation14–Citation16
Significant and oftentimes unwanted residual corneal astigmatism (RCA) could affect visual outcome following cataract surgery. It has been identified as an inevitable contributory factor to the sometimes poor visual outcome after cataract surgery.Citation17 Some studies have stated that RCA can be significantly blinding as the in situ cataractous lens and can severely affect visual function.Citation18,Citation19 RCA has been an influence in the evolution of cataract surgical techniques and incision types – in attempts to improve visual outcome by minimizing or preventing RCA.Citation20,Citation21 The type, size, and location of incisions, general surgical “insults” to corneal architecture, a surgeon’s experience, and other factors are said to also influence RCA.Citation17,Citation22
Herein, we attempted to compare the amounts of RCA between two groups of patients who underwent frown and straight incision forms of MSICS at a local hospital. We also studied visual acuity (VA) differences and changes between these two groups during the entire study period.
Methods
Participants
The participants were 60 persons with cataracts who had consented to undergo cataract surgery at a local hospital. All the individuals included in this study had operable cataracts with no obvious corneal abnormality and had also consented to participate in this study. They comprised 27 males and 33 females. Cataract patients at this local hospital are routinely assigned to either the frown or straight MSICS incision form by the surgeon in a simple random fashion. After explaining the research to the participants, informed consent was sought from them to have information relevant to this study extracted from their cataract surgery records at each visit, for data analysis. This mainly comprised VA and keratometry (k-) readings. Patients could withdraw from the study at their own will. Ethical approval was not sought as per the Kwame Nkrumah University of Science and Technology Institutional policy. All procedures conformed to the tenets of the Declaration of Helsinki.
Procedures
K-readings were obtained for each individual using a Bausch and Lomb one position variable doubling keratometer (model number K-6003). The k-readings at each visit were repeated thrice and the average recorded. Uncorrected vision (distance) for each participant was determined using a Snellen chart with backlight luminance of 160 cd/m2, at 6 m. All of these procedures were done during the preoperative period (before surgery) and then at each postoperative visit at intervals of the first to third week, the fourth to eleventh week, the 12th week and beyond – all following the day of cataract surgery.
Preoperative corneal astigmatism (PCA) was determined as the initial difference between k-reading values for the two principal corneal meridians of each participant’s eye before surgery. RCA was obtained in the same way; as the difference between the PCA and the corneal astigmatism at specific postoperative visits. Values of both the PCA and RCA were kept in units of diopters (D). All k-readings obtained were approximated to the nearest measurable D value.
Data were analyzed using SPSS version 20 (IBM Corporation, Armonk, NY, USA). Differences in mean PCA and RCA between groups were studied using bivariate independent Student’s t-test statistics. Fisher’s exact test was used to test for associations between comparable categorical groups. Microsoft Excel (2007) was used to plot graphs. A P-value <0.05 was considered significant.
Results
Participants’ demographics
Fifty eyes of 50 out of the 60 patients were successfully followed-up on for the period under study. The other ten were lost to follow-up. The mean age of these study participants was 64.34±15.64 years. is a cross tabulation of the sex and the incision groups of the 50 study participants.
Table 1 Cross tabulation of participants’ sex per incision group
Pattern of corneal astigmatism
The study showed that there was no statically significant difference in PCA between the incision groups (P=0.321) as well as between the sex groups (P>0.05). All participants had an overall mean PCA of 1.00±0.12 D; mean PCA value for the frown incision group was 1.00±0.12 D whereas mean PCA for the straight incision group was 1.25±0.12 D
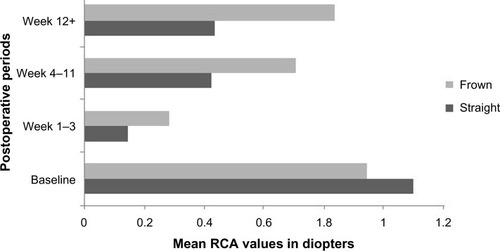
However, PCA levels dropped to values of ~0.25 D within the first 3 weeks following surgery. Levels of corneal astigmatism began to rise from the fourth week through the eleventh week and then remained steady at the 12th week and beyond ().
The differences in mean RCA for the incision groups, as studied using independent Student’s t-test, were observed to be statistically significant during the entire postoperative period (P<0.05). At all the set intervals of the postoperative visits, the recorded mean RCA values for the frown incision were higher than that recorded for the straight incision (P<0.05). The frown incision group showed RCA values that were approximately twice as high as that recorded for the straight incision group; RCA at the 12th week and beyond was 1.00±0.12 D for the frown incision group, whereas that for the straight incision group was 0.50±0.12 D ().
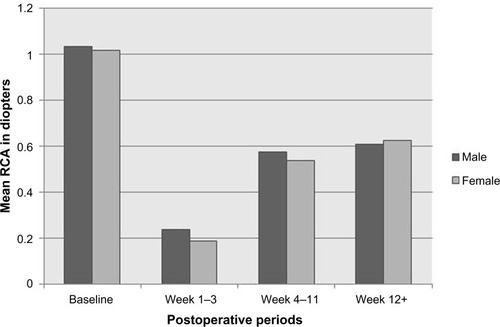
In studying the trend in corneal astigmatism between male and female groups, we detected that there was no significant difference in their mean RCA (P>0.05). This observation remained the same during the entire postoperative period. The mean RCA recorded at the end of the study for both male and female groups was ~0.75±0.12 D ().
It was interesting to observe that intra-group variations in mean RCA, that is for male versus female groups and frown versus straight incision groups, were not uniform within the first and third week of the postoperative period. The variations at this period as observed for the intra-incisions group () was statistically significant (t [39.85]=2.10, P=0.042) but was the opposite for the intra-sex group () (t [41.84]=0.82, P=0.42).
VA changes
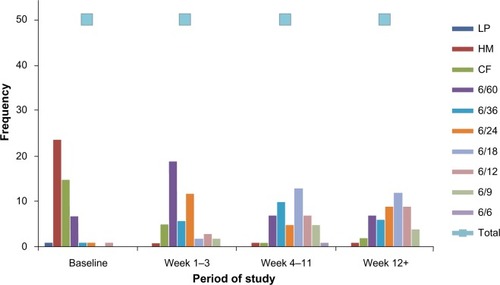
There was a general improvement in VA after extraction of the cataract. At baseline, 48% of the participants presented with a VA of hand-movement and 30% of them presented with an unaided VA of counting fingers. At the end of the study, 24% of them had an uncorrected VA of 6/18, whereas 18% had unaided VA of 6/12 with a few reading 6/9 on the Snellen chart.
is a summary of the pattern and distribution of VA among the study participants. Fisher’s exact test showed that there was no statistically significant association between VA and type of incision; for the frown and straight incision forms, P>0.05 at all stages of the study.
Discussion
Several studies have shown alterations in the power of preoperative astigmatism following cataract surgery.Citation16,Citation20,Citation21,Citation23–Citation25 Our study participants had a recorded mean age of 64.34±15.64 years. This agrees with what is reported in many literature sources that cataract remains a common condition among people in their fifth decades of life and beyond. The aged are frequently at risk of metabolic diseases that have an influence on the development of cataract.Citation1,Citation7,Citation10 There could be younger persons with cataracts as found among the few outliers in this study who may suffer cataracts congenitally or in their formative years form trauma, radiation, drugs, and other causes.Citation1,Citation5,Citation26,Citation27
All of the 50 participants were recorded to have the same amount of RCA. This was however not the situation in one study where only 75% of the study subjects were recorded to have RCA.Citation28 Whether or not a patient will suffer significant RCA following cataract surgery has been linked to factors such as the patient’s physiological characteristics, surgeon’s experience, disease, and several others.Citation22,Citation29
The overall mean RCA (1.00±0.12 D) recorded in our study falls between what other studies have reported. One study reported a value (1.85 D) higher than what was found in our study, whereas another study recorded an RCA value (0.525±0.804) lower than what is reported in our study.Citation16,Citation30 The overall mean RCA value of our study is however closer to what (1.30 D) another study reported.Citation23 The level of RCA has been found, in other studies, to be associated with preoperative corneal astigmatism present in a person’s eye prior to surgery. Others have linked the levels of RCA to the sites of the tunnel incision, corneal biomechanical properties, types and size of incision. Corneal hysteresis and other physiological differences of individual patients may have their own possible influences on RCA.Citation31,Citation32
While certain limitations of our study did not allow for further probing into the variations of RCA observed, the observed intra-group variations in the levels of RCA could be linked to corneal rigidity and thickness. General “surgical insults” to the cornea, corneal viscoelasticity, and ocular hypotony resulting from aqueous escape during cataract surgery could also influence the variations in RCA.Citation33–Citation35
Even though our study reports a statistically significant difference in the mean RCA values between the frown and straight incision groups (P<0.05), another study recorded a statistically insignificant difference (P=0.062) between the frown and straight incision groups. That other study also reported that the frown and straight incision forms caused more RCA compared to a (V-shape) chevron incision form.Citation25
Thus, it may be of interest for optometrists, particularly those in parts of the developing world where MSICS exists, to know what incision form a cataract patient is assigned in order to adequately assess the postoperative cataract patient for the presence of significantly reduced astigmatism. This will inform them about the best refractive correction to prescribe for such patients to ensure these patients have optimal VA following surgery.
shows there was a general improvement in VA during the entire postoperative period. Cataract surgery has been found, in most studies, as necessary for improvement in visual function and quality of life. This improved vision however, often gets better upon correction of the residual refractive errors – including RCA, with spectacles or contact lenses after the surgery.Citation13,Citation28,Citation36,Citation37,Citation38
As this study could posit, a slight improvement in VA following surgery is enough for some patients to default postoperative visits because such patients “see better than they did before surgery”. We lost 20% of the participants to follow-up; perhaps, the improvement in uncorrected VA, as they may have subjectively appreciated, could be a reason why some refused to show up for postoperative care and management. This is a common occurrence in most clinics across the developing world.
It is noteworthy to mention that cataract patients in some developing countries would have to wait until their vision becomes significantly impaired – often to an uncorrected VA of hand-movement before they are admitted for surgery. Most (>48%) of our patients presented with a VA of hand-movement or worse prior to surgery. A possible explanation may be the incommensurately low number of cataract surgeons compared to higher number of cataract patients in these parts of the world.Citation39
Conclusion
We found that mean RCA was higher in the frown incision group than straight incision group. The difference in mean RCA for the incision groups was statistically significant (P<0.05) but was not so for the sex groups (P>0.05). There was a general improvement in VA, but this observation did not have any statistically significant association with the incision forms during the entire study period (P>0.05), at all intervals of the postoperative period.
Recommendation
Future studies should consider including assessments of corneal biomechanical properties as these properties could provide useful insights into RCA findings.
Acknowledgments
The authors would like to extend their gratitude to the following personnel at the eye care facility for their help during data collection: Evelyn Sarpong (enrolled nurse), Afia Nkansah Asantewaa (OD), Akwasi Ahmed (MD), Sumaila Mohamadu (OD), Benjamin Brifa Bempong (OD), and Killian Asampana Asosega (statistician).
Disclosure
The authors have no conflicts of interest to disclose.
References
- KhuranaAKDiseases of the lens Comprehensive Ophthalmology4 edIndiaNew Age International®, Limited2007167200
- PascoliniDMariottiSPGlobal estimates of visual impairment: 2010Br J Ophthalmol201196561461822133988
- GyasiMAmoakuWAsamanyDBarriers to cataract surgical uptake in the upper east region of GhanaGhana Med J200741416717018464906
- GuzekJPAnyomiFKFiadoyorSNyonatorFPrevalence of blindness in people over 40 years in the Volta region of GhanaGhana Med J20063925562
- RobertsJEUltraviolet radiation as a risk factor for cataract and macular degenerationEye Contact Lens201137424624921617534
- CourtrightPBowmanRGilbertCLewallenSvan DijkKYorstonDChildhood cataract in AfricaVeenendaal, the NetherlandsDark and Light Blind Care2008
- ChangJRKooEAgrónERisk factors associated with incident cataracts and cataract surgery in the Age-related Eye Disease Study (AREDS): AREDS report number 32Ophthalmology2011118112113211921684602
- MohammadSKhanSUFCPSSUKFFactors responsible for Traumatic Cataract and its effects on visual acuityAn Official Journal of Peshawar Medical College201210182
- SharmaNGAravind Eye Care System—Compassion in Action2014 Available from: http://sdmimd.ac.in/SDMRCMS/cases/CIM2014/1.pdfAccessed February 27, 2016
- FletcherAEFree radicals, antioxidants and eye diseases: evidence from epidemiological studies on cataract and age-related macular degenerationOphthalmic Res201044319119820829643
- MvituMLongo-MbenzaBTulombaDNgeARegular, high, and moderate intake of vegetables rich in antioxidants may reduce cataract risk in Central African type 2 diabeticsInt J Gen Med2012548949322807635
- ArutaAMarencoMMarinozziSHistory of cataract surgeryMed Secoli200921140342820481376
- FongCSMitchellPRochtchinaETeberETHongTWangJJCorrection of visual impairment by cataract surgery and improved survival in older persons: the Blue Mountains Eye Study cohortOphthalmology201312091720172723664468
- ChakrabartiACataract Surgery in Diseased EyesJP Medical Ltd2014
- WongTYEffect of increasing age on cataract surgery outcomes in very elderly patientsBMJ200132272941104110611337443
- BehndigAMontanPSteneviUKugelbergMZetterströmCLundströmMAiming for emmetropia after cataract surgery: Swedish National Cataract Register studyJ Cataract Refract Surg20123871181118622727287
- RaiyawaSJenchitrWYenjitrBTapunyaMVisual acuity in patients having cataract surgery by different techniquesJ Med Assoc Thai200891Suppl 1S92S10118672600
- SmithJSEye diseases in hot climates4 edIndiaElsevierIndia Private Limited2003
- ReadSAVincentSJCollinsMJThe visual and functional impacts of astigmatism and its clinical managementOphthalmic Physiol Opt201434326729424635572
- YaoKTangXYePCorneal astigmatism, high order aberrations, and optical quality after cataract surgery: microincision versus small incisionJ Refract Surg2006229 SupplS1079S108217444097
- ElkadyBAlióJLOrtizDMontalbánRCorneal aberrations after microincision cataract surgeryJ Cataract Refract Surg2008341404518165079
- OdugboOPBabalolaOEMorganREInfluence of rank of surgeon on the outcome of cataract surgery in Plateau State NigeriaJos J Med201152212216
- AcharAKadriRHegdeSKudvaADevikaPJohnVSurgically induced astigmatism following cataract surgery: A comparative studyInt J A.J. Inst Med Sci20132144
- ChoYKKimMSPerioperative modulating factors on astigmatism in sutured cataract surgeryKorean J Ophthalmol200923424024820046682
- JauhariNChopraDChaurasiaRKAgarwalAComparison of surgically induced astigmatism in various incisions in manual small incision cataract surgeryInt J Ophthalmol2014761001100425540754
- ReadSACollinsMJCarneyLGA review of astigmatism and its possible genesisClin Exp Optom200790151917177660
- DobsonVMillerJMHarveyEMCorneal and refractive astigmatism in a sample of 3- to 5-year-old children with a high prevalence of astigmatismOptom Vis Sci1999761285586010612408
- AdioAOAruotoNInduced astigmatism after cataract surgery-a retrospective analysis of cases from the University of Port Harcourt Teaching Hospital, NigeriaAfr Vis Eye Health20117027580
- RobertsTVLawlessMBaliSJHodgeCSuttonGSurgical outcomes and safety of femtosecond laser cataract surgery: a prospective study of 1500 consecutive casesOphthalmology2013120222723323218822
- AruotuNUzoDikeEPrevalence of astigmatism in post operative cataract in University of Port Harcourt Teaching Hospital, NigeriaJ Med Med Sci201121632637
- MatsumotoYHaraTChibaKChikudaMOptimal incision sites to obtain an astigmatism-free cornea after cataract surgery with a 3.2 mm sutureless incisionJ Cataract Refract Surg200127101615161911687361
- DenoyerARicaudXVan WentCLabbéABaudouinCInfluence of corneal biomechanical properties on surgically induced astigmatism in cataract surgeryJ Cataract Refract Surg20133981204121023756347
- BerdahlJPCataract surgery to lower intraocular pressureMiddle East Afr J Ophthalmol200916311920142975
- HjortdalJØRegional elastic performance of the human corneaJ Biomech19962979319428809623
- ElsheikhAWangDBrownMRamaPCampanelliMPyeDAssessment of corneal biomechanical properties and their variation with ageCurr Eye Res2007321111917364730
- WangLDixitLWeikertMPJenkinsRBKochDDHealing changes in clear corneal cataract incisions evaluated using Fourier-domain optical coherence tomographyJ Cataract and Refract Surg201238466066522321355
- NaeserKAssessment of surgically induced astigmatism; call for an international standardJ Cataract and Refract Surg1997239127880
- SabesanRJeongTMCarvalhoLCoxIGWilliamsDRYoonGVision improvement by correcting higher-order aberrations with customized soft contact lenses in keratoconic eyesOpt Lett20073281000100217375181
- TabinGChenMEspandarLCataract surgery for the developing worldCurr Opin Ophthalmol2008191555918090899