Abstract
Purpose
Traumatic brachial plexus injury (TBPI) causes severe disabilities to the patients, affecting not only upper limb function but also the psychosocial and economic aspects. Free functional muscle transfer (FFMT) is one of the reconstruction modalities for the management of TBPI. The aim of this study is to evaluate the functional outcomes and their correlation to patient factors.
Patients and Methods
This is a retrospective study of 131 patients who suffered from complete TBPI (C5-T1) and were treated with the FFMT procedure to restore elbow flexion and wrist extension from 2010 to 2018 in our institution. We evaluated the active range of motion (AROM), muscle power with MRC (Medical Research Council) scale, DASH score, and complications, with a minimum of 12-month follow-up.
Results
Following FFMT surgery, elbow flexion was significantly and successfully restored (MRC ≥ 3) in 75.5% of patients with an average AROM of 88.17 ± 41.29°. The wrist extension was restored in 42% of the patients with an average AROM of 20.69 ± 18.72°. There was no correlation between age, side of injury, and time to surgery with the functional outcomes. There was a weak correlation between education level, rehabilitation compliance, and elbow functional outcomes.
Conclusion
FFMT is a reliable surgical option to restore elbow flexion in TBPI with a high satisfactory result. Our findings suggested that the FFMT indication is potentially expanded regardless of the patient factors.
Introduction
Traumatic brachial plexus injury (TBPI) is a severe peripheral nerve injury of the upper limb, which causes tremendous disabilities due to pain, motor, and sensory deficits.Citation1,Citation2 This disability affects the patient’s psychological, social and economic aspects which result in decreased quality of life. The treatment to completely restore in TBPI patients is still challenging, therefore partial recovery of any function of the upper limb in TBPI patients means a lot. Treatment for TBPI patients compromises surgical nerve and muscle/tendon procedures. Nerve procedures such as external neurolysis, nerve repair, nerve grafting, and nerve transfer are preferable for patients with early TBPI presentations (≤6 months).Citation1 However, conditions in which nerve procedures are failed to restore elbow function or in delayed cases where neuromuscular junction already degenerated, muscle/tendon procedures are indicated.Citation1,Citation3,Citation4 In our hospital, 67% of TBPI patients were performed surgical nerve procedures, while the other 33% were performed surgical muscle/tendon procedures.
Free functional muscle transfer (FFMT) is a muscle procedure to reconstruct defective muscle function by grafting free muscles including blood vessels and nerves. This procedure primarily aims to restore the elbow function, which may be followed by partial shoulder and hand restoration depending on its site of attachment.Citation3 The consideration of restoring wrist extension as a secondary outcome in our study is to accommodate further finger flexion restoration procedure while preserving the wrist extension movement that is needed during motorcycle riding (which is of importance in most of our study population).Citation5
Although there is still debate about which time is the best for TBPI patients to be operated on, it has been found in a systematic review study that in the stretch and blunt injury of the brachial plexus, the ideal operative timeframe appears to be less than six months after injury. Nevertheless, a 3-month delay is generally acceptable.Citation6 This study focuses on FFMT to restore elbow flexion and wrist extension for complete TBPI in our center. In this study, we hypothesized that: (1) Patients who underwent FFMT will have a post-operative improvement compared to the pre-operative conditions; (2) Patients’ factors have no correlation with FFMT outcomes.
Materials and Methods
This is a retrospective study of TBPI patients who underwent FFMT surgery from 2010 to 2018 in our center. Our inclusion criteria were: (1) TBPI complete type (C5-T1) patients; (2) Underwent FFMT procedures using gracilis muscle as a donor for elbow flexion and wrist extension (including those who underwent FFMT as their primary procedures and those who were converted to FFMT after a failed primary procedure); (3) completed preoperative rehabilitation sessions (stimulation of the motor endplate and the muscle, and pROM exercise to prevent stiffness); (4) minimum 1-year follow-up. Whereas, our exclusion criteria were: (1) TBPI patient who underwent other surgical modalities (nerve transfer, nerve repair, nerve grafting, neurolysis, and tendon transfer) and never received FFMT procedure for elbow flexion; (2) Underwent double FFMT; (3) Incomplete data/loss to follow-up; (4) Joint contractures at the upper extremity; (5) Respiratory problems prior to surgery.
Surgical Technique
All surgeries were performed by a senior author in a single institution. Brachial plexus was explored with supra- and infraclavicular approach. The phrenic nerve was identified and checked for its viability using a nerve stimulator. If there was no contraction of the diaphragm muscle, the procedure continued to find the spinal accessory nerve, and its viability was also checked. If the potential nerve donor diameter seemed too thin, the intercostal nerves were used for neurotization. We used two ICNs (III and IV) because in all cases the gracilis nerve only had two big motor fascicles. The infraclavicular approach was performed to find the thoracoacromial artery and cephalic vein. The medial distal humerus and dorsal forearm approaches were performed to prepare the recipient site of muscle transfer. The phrenic nerve was used in 61 cases (46.5%), the accessory nerve in 44 cases (33.5%), and the intercostal nerve in 26 cases (20%).
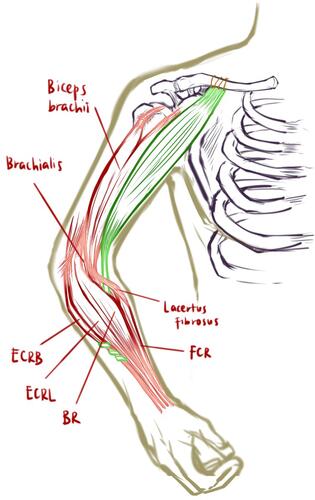
Gracilis muscle was harvested distally at its insertion and proximally at its origin along with its artery, vein, motor branch nerve, and sometimes with skin paddle. Gracilis muscle was then transferred with its afferent and efferent blood vessels and nerves to the affected arm. Hereafter, we performed a modified technique developed by our senior author as follows: The origin of the transferred gracilis muscle was implanted to the middle-third clavicle, the tendon was placed underneath the lacertus fibrosus and mobile wad compartment, and then attached to the middle-third of the Extensor Carpi Radialis Brevis (ECRB) tendon (distal to musculo-tendineous junction) to provide enough space within the tendon mass that allows sufficient tendon weaves which may lead to a strong fixation ().
Figure 1 Free functional muscle transfer (FFMT) surgical technique illustration. The origin of the transferred gracilis muscle was implanted directly to the periosteum middle-third clavicle with continuous suture through proximal tendon part of gracilis muscle. The distal tendon was placed underneath the lacertus fibrosus and mobile wad compartment, and then attached to the proximal side of the Extensor Carpi Radialis Brevis (ECRB) tendon. Green coloured: Gracilis muscle.
Revascularization was performed with end-to-end anastomosis of the afferent artery to the thoracoacromial artery and the veins to the cephalic vein. We performed reinnervation by connecting the motor branch of the gracilis muscle to the phrenic nerve as the first choice; or when inapplicable (injured or non-viable), we used the accessory or intercostal nerve on the affected side. Prior to surgery, the donor nerve candidates were checked for their potential (clinically according to their respective muscle function, chest radiograph, and EMG); whereas, they were rechecked with a nerve stimulator during surgery. If the patient came within the time frame for the nerve procedure, we also tried to find another donor for an additional nerve transfer or grafting to restore shoulder abduction.
After the surgery, the patient’s arm was immobilized in a 90° of elbow flexion position until six weeks to ensure the healing of the vascular, nerve anastomoses, and stitches of the origin and insertion. We gradually reduced the elbow flexion by 10–20 degrees every week until a full extension was achieved. Then, the active range of movement (AROM) exercise commenced by activating the nerve source in the fourth to sixth months. The FFMT procedure was defined as successful if the elbow flexion muscle power reached Medical Research Council’s scale (MRC)Citation7 3 or more.
Data Collection and Statistical Analysis
Data were collected by the research team. Patient factors such as age, gender, side of injury, education level, the timing of surgery, follow-up duration, and compliance following the medical rehabilitation program were collected. On the last follow-up, we collected the primary outcomes (AROM and MRC for elbow flexion) and secondary outcomes: Shoulder forward flexion, wrist extension, and Disabilities of the Arm, Shoulder, and Hand (DASH)Citation8 score. The DASH score questionnaire was filled out by the patients under the assistance of the research team due to the language problem since the Indonesian translated version of DASH questionnaire has not been validated yet. The frequency of patient visits to the medical rehabilitation clinic within one year after surgery was recorded. Patients with more than 30 visits of occupational therapy were classified as compliant, while less than 30 visits were classified as non-compliant.
All data were first tested using the Kolmogorov–Smirnov normality test. Our data were not normally distributed. Thus, Wilcoxon signed rank sum test for paired samples was used. The correlation between patient factors and postoperative clinical outcome analysis was performed using the Spearman test. The significance level was set at p < 0.05.
Results
Patient Characteristics
From 2010 to 2018, as much as 172 TBPI patients were treated with FFMT. Among them, 11 had double FFMT, 8 had FFMT for elbow extension (lower plexus injury), 10 had incomplete data, 11 were lost to follow-up, 1 patient had staged procedure due to elbow contracture. There were 131 patients included in this study. Most of the patients were males (83.2%) with an average age of 27.71 ± 10.63 years. The patients tend to have a late presentation, consequently, as much as 45% of patients were operated on 12 months after the injury, with the longest time to surgery being 30 years after the injury. The median time from onset to surgery was 11 months (6–24 months). All of the patients had a minimum of 1-year follow-up with a median of 57 months (39–78 months). Further details about patient factors such as gender, BMI, side of injury, education level, time to surgery, rehabilitation compliance, donor nerve used for muscle graft, and follow-up time are shown in .
Table 1 Traumatic Brachial Plexus Injury Patient Characteristics
Clinical Outcomes
AROM for elbow flexion, shoulder flexion, and wrist extension before surgery was 0 degrees in all patients (). Successful restoration of elbow flexion (MRC ≥ 3) was observed in 75.5% of patients with average postoperative AROM of the elbow at 88.17 ± 41.29°. The average postoperative shoulder flexion AROM was 58.74 ± 38.48° with 58.1% of patients reaching MRC ≥ 3. The average postoperative wrist extension AROM was 20.69 ± 18.72° with 42% of patients reaching MRC ≥ 3. The average preoperative DASH score of patients was 88.46 ± 6.49 (range, 73.33–96.67) and the average postoperative DASH score of patients was 28.26 ± 23.34 (range, 7.5–96.67).
Table 2 Clinical Outcomes
Statistical Analysis
We found a statistically significant difference between pre- and postoperative measurements of all clinical outcomes using Wilcoxon test (). As for the correlation analysis (), we found a weak correlation between gender and wrist ROM (r = 0.181), gender and wrist MRC (r = 0.194), BMI and post-op DASH (r = 0.201), education level and elbow ROM (r = −0.202), education level and elbow MRC (r = −0.178), compliance to rehabilitation and elbow ROM (r = −0.167), and educational level to rehabilitation compliance (r = 0.378). There was no significant difference of clinical outcomes between the patients who were operated earlier and the patients who presented late ().
Table 3 Correlation Between Patient Factors with Post-Operative Clinical Outcomes
Table 4 Clinical Outcome Related to Time to Surgery
Complications
Postoperative complications include surgical site infection in the recipient and donor area (four patients, 3% and two patients, 1.5%) which all healed completely after adequate antibiotic treatment; numbness in the thigh was observed in two patients (1.5%), which resolved after four months; seven patients (5.3%) have vascular anastomosis problem which led to graft necrosis; and five patients (3.8%) have a failed re-innervation problem which led to FFMT failure.
Discussion
Elbow flexion is undoubtedly the priority in TBPI reconstruction, followed by shoulder, wrist, and hand function.Citation2 Many studies have reported that elbow flexion restoration improves the quality of life and increases the chance of the patient to return to work and make a living.Citation2,Citation3 FFMT is one treatment modality to restore elbow flexion in brachial plexus injury. A systematic review by Lee et al revealed that most FFMT literature only involved small numbers of patients, ranging from 2 to 42 patients.Citation3 We present 131 TBPI patients who underwent FFMT procedures, making this study one of the largest series in the literature.
We followed the patients for a minimum of 12 months as no significant outcome improvement will come after 12 months after surgery. Yang et al'sCitation2 study suggests that after one year of normalized rehabilitation, patients can recover gracilis muscle power. Furthermore, patients who had poor function recovery showed no improvement after two years or more rehabilitation in their study.Citation2
In this study, we achieved elbow flexion restoration with a success rate of 75.5% (≥M3), with an average elbow flexion AROM of 88.17 ± 41.29°. These findings are consistent with previous literatures that reported the average postoperative elbow AROM varied from 68° to 107°.Citation2,Citation9–Citation11 The success rate (MRC ≥3 for elbow flexion) in our finding is also comparable to the systematic reviews which reported the success rates of FFMT for elbow flexion are about 46% to 88%.Citation3,Citation10,Citation12,Citation13
Other than achieving elbow flexion alone, FFMT has also been developed to provide some distal functions other than the useful shoulder and elbow movement. However, controversies exist for the distal attachments of the tendon. Some believe that the elbow flexion strength in a more distal muscle attachment can be lower than a more proximal attachment on the biceps tendon.Citation12 Barrie et al'sCitation12 study of 29 FFMT cases showed that distal attachment to biceps alone achieves a greater success rate of elbow flexion strength than double FFMT with distal attachment at ECRB and FDP & FPL (79% vs 63%).Citation12
In our study, we attached the gracilis tendon to the ECRB tendon. This configuration would produce forearm pronation, wrist extension, and shoulder forward flexion simultaneously during elbow flexion movement.Citation12 We achieved a comparable successful rate as in other study and this finding is consistent with Maldonado et al'sCitation14 study which showed that elbow flexion strength is clinically and biomechanically superior in FFMT group with the more distal attachment. Furthermore, the re-creation of pulley (ie, the lacertus fibrosus, sling under wrist extensors) can prevent bowstringing and increase the effectiveness of the muscle pull.
Moreover, the majority of the patients in our study drive two-wheelers. The wrist extension motion is highly needed in our population to perform this activity other than elbow flexion and shoulder stabilization. Thus, we performed the FFMT for elbow flexion and wrist extension as our main priority. Further FFMT for finger flexions is planned for the next procedure. In addition to the elbow function improvement, we also achieved a significant wrist and shoulder function improvement. In fact, the wrist extension in our study was slightly higher than reported in Yang et alCitation2 (average ROM 17° with 21.43% MRC ≥3) and Oliver et alCitation13 (52.9% reach MRC ≥3) study.
The elbow flexion, shoulder forward flexion, and wrist extension improvement could also increase the overall function of the upper limb as reflected in an improvement of the DASH score. DASH questionnaire is a standardized measure that evaluates impairments and activity limitations of the upper extremity based on patients’ own perspective.Citation8 Though not specified to evaluate FFMT, the DASH score could represent how FFMT improves patients’ quality of life. In our study, the average DASH score after the FFMT procedure was 28.26 ±23.34 which was slightly better than other studies by Estrella et alCitation10 and Maldonado et alCitation15 43.09±14.9 and 36.5±19, respectively. Each patient experienced a DASH score average decrease of 49.1±7.3 points (from 86.1±7.2 to 36.9±7.3), which is better than the previously reported study (from 66±14 to 36±15).Citation16
There were only a few studies that correlate patient factors to functional outcomes in FFMT. In a study on FFMT for facial palsy reconstruction, excursion and satisfaction scores were significantly worse in the older age group.Citation17 In our study, there was mostly no correlation and some weak correlation between patient factors and outcomes as shown in . In fact, those statistically weak correlations had no clinical correlation which means that FFMT outcomes do not depend on these factors. Our findings are consistent with Yi et alCitation2 and Sabthai et alCitation11 studies which showed that patient factors such as age, sides, the interval between primary injury and treatment, follow-up time, level of injury, and accompanying procedures did not have any significant impact on the primary outcome: elbow flexion and wrist extension muscle power or ROM.
FFMTs had proven a good outcome for cases with late presentation or in the absence of nerve recovery after neurological procedures.Citation19 Basically, the healthy nerves are used to innervate a healthy muscle that is transferred to restore upper-limb function in FFMT procedure for TBPI patients. Thus, the time frame is not limited, unlike the nerve reconstruction procedure where timing is a critical consideration for the nerve regeneration.Citation18 In our study, there was no correlation between time to surgery and clinical outcome, as further shown in result that there was no significant difference of clinical outcome among time to surgery group.
The rehabilitation for brachial plexus surgery starts even before the surgery to maintain the stimulation of the motor endplate, the muscle, and prevent stiffness. Whereas, the postoperative rehabilitation program focuses on re-education of the nerve or muscle to train the brain for sending information along a new nerve pathway or grafted muscle with the biofeedback method. Although it has not been proven yet, we believe that this learning process correlates with patient motivation and knowledge about the disease and therapy. This rehabilitation program with good compliance is expected to optimize the overall success of the FFMT surgery. However, in our study, the correlation between these factors to the outcome was weak. Further studies are needed and the clinicians should focus on this rehabilitation and continuing patient education to make sure regardless of the patient basic knowledge, we as the clinician can aid the patient to achieve maximum benefit of the therapy.Citation20
The reported complications of FFMT in previous publications included wound infections, delayed healing, unsightly scarring, donor site numbness, bowstringing, thrombosis, and failed re-innervation. Donor site numbness and bowstringing were the most common short- and long-term complications.Citation2 Literature reporting complication rate after FFMT procedure was varied from 4% to 35%.Citation3 In this study, the complication rate of FFMT is 15.2%. The infection cases in our study were all healed completely after adequate antibiotic treatment. The infections were all superficial and may be caused by long surgical duration. No cases needed surgical debridement to control the source of infection. The numbness over the thigh region was observed in two patients, which recovered spontaneously by the 4th month after surgery. Numbness was probably caused by skin sensory nerve damage and its recovery was achieved by cross re-innervation from surroundings. The vascular anastomosis problem in our study is probably due to the caliber mismatch between donor and recipient vessels. Further investigation about complication rates of FFMT is needed since it is only reported by a few literatures with small samples.
Conclusion
This is the largest series about FFMT for TBPI in a single center and one of a few studies that correlate patient factors to FFMT. We found that FFMT is a reliable surgical option to restore elbow flexion in TBPI with a high satisfactory result. The indication of FFMT for traumatic TBPI could be expanded regardless of the patient factors. Limitations of this study were its retrospective nature and varied time in the postoperative data collection. Future research should consider the patient’s education and rehabilitation point of view, comparing other patient factors such as nerve source for muscle graft, and further evaluation of donor site morbidities.
Ethical Approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Dr. Soetomo General Academic Hospital, Surabaya, Indonesia with protocol approval number: 1399/KEPK/VIII/2019. The privacy and information regarding personal identity of each participant were protected. The written informed consent was obtained from all participants.
Disclosure
The authors declare no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Funding
References
- Bhandari PS, Bhatoe HS, Mukherjee MK, Deb P. Management strategy in post traumatic brachial plexus injuries. Indian J Neurotrauma. 2012;9(1):19–29. doi:10.1016/j.ijnt.2012.04.010
- Yang Y, Yang JT, Fu G, et al. Functioning free gracilis transfer to reconstruct elbow flexion and quality of life in global brachial plexus injured patients. Sci Rep. 2016;6(February):1–10. doi:10.1038/srep22479
- Yi Lee TM, Sechachalam S, Satkunanantham M. Systematic review on outcome of free functioning muscle transfers for elbow flexion in brachial plexus injuries. J Hand Surg Eur Vol. 2019;44(6):620–627. doi:10.1177/1753193419825527
- Fischer JP, Elliott RM, Kozin SH, Levin LS. Free function muscle transfers for upper extremity reconstruction: a review of indications, techniques, and outcomes. J Hand Surg Am. 2013;38(12):2485–2490. doi:10.1016/j.jhsa.2013.03.041
- Suroto H, Antoni I, Siyo A, et al. Traumatic Brachial Plexus Injury in Indonesia: an experience from a developing country. J Reconstr Microsurg. 2021. doi:10.1055/s-0041-1735507
- Martin E, Senders JT, DiRisio AC, Smith TR, Broekman MLD. Timing of surgery in traumatic brachial plexus injury: a systematic review. J Neurosurg. 2019;130(4):1333–1345. doi:10.3171/2018.1.JNS172068
- Compston A. Aids to the investigation of peripheral nerve injuries. Medical Research Council: nerve Injuries Research Committee. His Majesty’s Stationery Office: 1942; pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By Michael O’Brien for the Guarantors of Brain. Brain. 2010;133(10):2838–2844. doi:10.1093/brain/awq270
- Jester A, Harth A, Wind G, Germann G, Sauerbier M. Disabilities of the Arm, Shoulder and Hand (Dash) questionnaire: determining functional activity profiles in patients with upper extremity disorders. J Hand Surg Br Eur Vol. 2005;30B(1):23–28. doi:10.1016/j.jhsb.2004.08.008
- Potter SM, Ferris SI. Reliability of functioning free muscle transfer and vascularized ulnar nerve grafting for elbow flexion in complete brachial plexus palsy. J Hand Surg Eur Vol. 2017;42(7):693–699. doi:10.1177/1753193417702029
- Estrella EP, Montales TD. Functioning free muscle transfer for the restoration of elbow flexion in brachial plexus injury patients. Injury. 2016;47(11):2525–2533. doi:10.1016/j.injury.2016.08.011
- Satbhai NG, Doi K, Hattori Y, Sakamoto S. Functional outcome and quality of life after traumatic total brachial plexus injury treated by nerve transfer or single/double free muscle transfers: a comparative study. Bone Jt J. 2016;98B(2):209–217. doi:10.1302/0301-620X.98B2.35101
- Barrie KA, Steinmann SP, Shin AY, Spinner RJ, Bishop AT. Gracilis free muscle transfer for restoration of function after complete brachial plexus avulsion. Neurosurg Focus. 2004;16(5):1–9. doi:10.3171/foc.2004.16.5.9
- Oliver JD, Beal C, Hu MS, Graham EM, Santosa KB. Functioning free muscle transfer for brachial plexus injury: a systematic review and pooled analysis comparing functional outcomes of intercostal nerve and spinal accessory nerve grafts. J Reconstr Microsurg. 2020;84132.
- Maldonado AA, Romero-Brufau S, Kircher MF, Spinner RJ, Bishop AT, Shin AY. Free functioning gracilis muscle transfer for elbow flexion reconstruction after traumatic adult brachial pan-plexus injury: where is the optimal distal tendon attachment for elbow flexion? Plast Reconstr Surg. 2017;139(1):128–136. doi:10.1097/PRS.0000000000002864
- Maldonado AA, Kircher MF, Spinner RJ, Bishop AT, Shin AY. Free functioning gracilis muscle transfer with and without simultaneous intercostal nerve transfer to musculocutaneous nerve for restoration of elbow flexion after traumatic adult brachial pan-plexus injury. J Hand Surg Am. 2017;1–7. doi:10.1016/j.jhsa.2017.01.014
- Dodakundi C, Doi K, Hattori Y, et al. Outcome of surgical reconstruction after traumatic total brachial plexus palsy. J Bone Jt Surg - Ser A. 2013;95(16):1505–1512. doi:10.2106/JBJS.K.01279
- Jcy L, Fang F, Lin JTK, Chang TNJ, Chuang DCC. Impact of increasing age on functioning free muscle transplantation for facial palsy reconstruction. Microsurgery. 2020;40(2):110–116. doi:10.1002/micr.30481
- Brenner MJ, Moradzadeh A, Myckatyn TM, et al. Role of timing in assessment of nerve regeneration. Microsurgery. 2008;28(4):265–272. doi:10.1002/micr.20483
- Martins-Filho FVF, Do Carmo Iwase F, Silva GB, et al. Do technical components of microanastomoses influence the functional outcome of free gracilis muscle transfer for elbow flexion in traumatic brachial plexus injury? Orthop Traumatol Surg Res. 2021;107(2):102827. doi:10.1016/j.otsr.2021.102827
- Arfianti L, Haryadi RD. The outcome of biofeedback muscle re-education after brachial plexus reconstruction: a case series. Surabaya Phy Med Rehabil J. 2020;35–41.
