Abstract
Introduction
There is increasing evidence that systemic inflammation influences the prognosis in patients with malignant tumors. The aim of this research was to investigate the prognostic value of neutrophil/lymphocyte ratio (NLR) in patients with primary small-cell carcinoma of the esophagus.
Methods
This study retrospectively analyzed 129 patients with primary small-cell carcinoma of the esophagus who underwent esophagectomy in The Fourth Hospital of Hebei Medical University between January 2008 and December 2010. NLRs were calculated by using the following formula: peripheral neutrophil count/lymphocyte count (109/L). Correlations of NLR with other clinicopathologic data and prognosis were analyzed. The survival rate was calculated by Kaplan–Meier analysis. The differences between groups were compared by using the log-rank test. Cox regression was used to analyze the factors that may affect the survival of the patients.
Results
The survival rate was found to be related to tumor stage, tumor location, nodal metastasis, TNM stage, histology, adjuvant therapy, and NLR (all P<0.05). High-NLR group had significantly poorer survival than low-NLR group (1-, 3-, and 5-year survival rates: 46.6% vs 57.1%, 21.9% vs 50.0%, and 5.5% vs 23.2%, respectively, P=0.002). NLR was identified as an independent prognostic factor for patients with primary small-cell carcinoma of the esophagus.
Conclusion
NLR is a valuable clinical marker in preoperative estimation as well as prognosis prediction for patients with primary small-cell carcinoma of the esophagus.
Introduction
Primary small-cell carcinoma of the esophagus (SCCE) is an extremely rare disease, representing only 0.005%–4% of esophageal cancers (ECs) and 0.004%–4.6% of all gastrointestinal neuroendocrine neoplasms.Citation1,Citation2 On account of its rarity, a standard treatment has not yet been established.Citation2 Patients with SCCE have been treated with surgery, chemotherapy, and radiotherapy, alone or in combination.Citation1 However, the outcome for SCCE remains grim due to a poor therapeutic response and a high rate of disease recurrence.Citation3
Recently, there is increasing evidence that systemic inflammatory response plays an important role in postoperative survival in patients with gastrointestinal cancers.Citation4–Citation6 Previous studies have shown that pretreatment neutrophil/lymphocyte ratio (NLR), as an index of systemic inflammation, influenced the prognosis in patients with various cancers, including esophageal squamous cell carcinoma.Citation7–Citation9 The present study investigated the prognostic value of NLR in patients with SCCE.
Methods
Patients
From January 2008 to December 2010, a total of 4,141 patients received esophagectomy for EC at the Department of Thoracic Surgery, Tumor Hospital of Hebei (Shijiazhuang, China). The inclusion criteria were as follows: 1) SCCE confirmed by histopathology, 2) surgery with curative esophagectomy, 3) surgery not preceded by neoadjuvant therapy, and 4) preoperative NLRs obtained before esophagectomy within 1 week. The exclusion criteria were as follows: 1) non-SCCE, 2) previous or coexisting cancers other than SCCE, 3) previous chemotherapy and/or radiotherapy, 4) active concomitant infection within 1 week, and 5) distant metastasis. Finally, 129 patients were found to be eligible for this study. The following data of all the patients were collected: age, gender, laboratory examination, tumor stage and location, nodal metastasis, histology, and other miscellaneous characteristics on the basis of the medical records. Ethical approval from the ethical committee of the Tumor Hospital of Hebei, Shijiazhuang, China, was obtained. Informed consent was obtained from all individual participants included in the study.
Follow-up
All patients received a standardized 3-month interval follow-up for the first year after operation, 6-month interval follow-up in the next 2 years, and yearly follow-up thereafter. Medical history, physical examination, and computed tomography of the chest were recorded during the follow-up. The last follow-up date was December 31, 2015.
Statistical analysis
All statistical calculations were performed by using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA). The relationship between NLR and other clinicopathologic factors was analyzed by Pearson’s chi-squared test. Survival rate was analyzed by Kaplan–Meier analysis with log-rank test. A multivariate Cox proportional hazards regression model with the enter method was constructed to identify independent prognostic factors. A 95% confidence interval (CI) was used to quantify the relationship between survival time and each independent factor. All P-values were two-sided in the tests. P<0.05 was considered statistically significant. The Akaike information criterion (AIC) was used to identify the statistical model.Citation10 AIC was defined as AIC = −2 log(maximum likelihood) + 2 × (number of parameters in the model). A smaller AIC value indicates a more desirable model for predicting outcomes.
Results
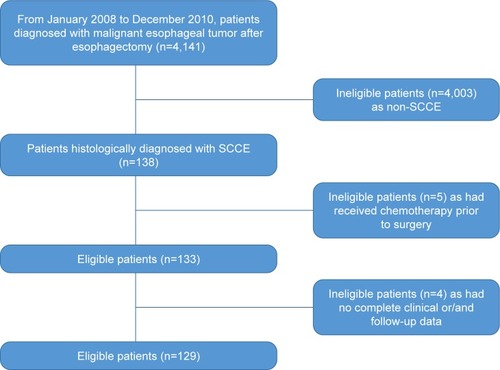
More than 4,000 patients with pathologically confirmed malignant tumors of the esophagus after surgery were recruited. Among these patients, 138 patients were confirmed with SCCE, 133 patients had received no neoadjuvant therapy prior to esophagectomy, and 129 patients had complete clinical data including age, gender, histology, tumor location and stage, nodal metastasis, complete blood count, and treatment. Finally, 129 patients were included in the study. The study flowchart is shown in . The median age for the patients was 60 years (range: 39–78 years). Eighty-five (65.9%) of the patients were men. Forty-eight (37.2%) patients had stage I, 54 (41.9%) had stage II, and 27 (20.9%) had stage III SCCE. At the end of this study (December 31, 2015), 113 (87.6%) patients died. The median follow-up duration for those who were still alive at the final follow-up was 67.5 months (range: 60–81 months).
All the eligible patients underwent radical esophagectomy. One hundred and eighteen patients underwent one incision via left thoracic approach. Three patients were treated by thoracotomy on the right side and intrathoracic gastric reconstruction. Lesions of the upper third were treated by cervical anastomosis. Along with esophagectomy, lymphadenectomy was performed, including the subcarinal, paraesophageal, pulmonary ligament, diaphragmatic, and the origin of the left gastric artery. The cervical lymph node dissection was performed only if abnormality was confirmed by preoperative evaluation. All of the patients were restaged according to the seventh edition of the American Joint Committee on Cancer (AJCC) Cancer Staging Manual.Citation11 All patients received adjuvant chemotherapy. Forty-nine (38.0%) patients received adjuvant chemoradiotherapy. Among these patients, 19 (38.8%) patients received conventional radiotherapy, 16 (32.7%) patients received three-dimensional conformal radiotherapy, and the remaining 14 (28.5%) patients received an intensity-modulated radiation therapy.
Receiver operating characteristic (ROC) curves for overall survival (OS) prediction were plotted to verify the optimum cutoff point for NLR. The area under the ROC curve was 0.704 (95% CI: 0.589–0.818) and, according to the ROC curve, the best cutoff value of NLR was 2.97, with a sensitivity of 61.1% and a specificity of 62.5%. The patients were then divided into two groups according to NLR: 56 (43.4%) patients with NLR <2.97 and 73 (56.6%) patients with NLR ≥2.97.
The relationship between NLR and the clinicopathologic characteristics of the 129 patients with SCCE is shown in . This study showed that NLR was not associated with any clinicopathologic characteristic in list.
Table 1 General characteristics of patients according to NLR groups
The median OS was 12 months (95% CI: 10.9–13.1). The 1-, 3-, and 5-year survival rates were 51.2%, 34.1%, and 13.2%, respectively. Our univariate analysis showed that seven clinicopathologic variables, namely histology, tumor location and stage, nodal metastasis, TNM stage, adjuvant therapy, and NLR, were significantly associated with OS (, ). All of the confounding factors were then included in the multivariate Cox proportional hazards model (enter procedure) to adjust for the effects of covariates, which demonstrated that NLR was a valuable clinical marker in prognosis prediction for patients with primary SCCE (NLR <2.97 vs ≥2.97, P=0.004, ). The predictive effect of NLR on OS rate was further assessed after stratification by nodal metastasis staging. NLR was associated with clinical outcome only in patients with pN0 disease (). pN0 patients with an NLR ≥2.97 had significantly worse OS (hazard ratio (HR) =2.314; 95% CI: 1.401–3.822; P<0.001) (). No differences were observed in patients with other pN stages.
Figure 2 Kaplan–Meier analysis of NLR for OS in patents with SCCE.
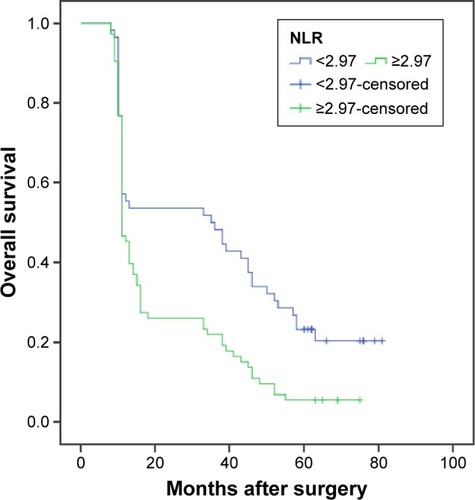
Figure 3 Kaplan–Meier analysis of NLR for OS in patents with pN0 SCCE.
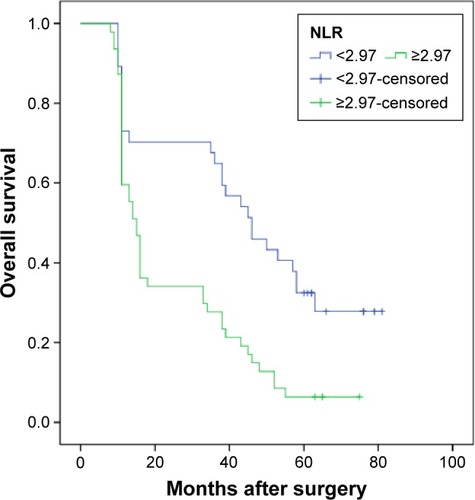
Table 2 Univariate analysis of prognostic factors of overall survival
Table 3 Multivariate survival analysis for various potential prognostic factors of overall survival
Table 4 Univariate analysis of NLR stratified by nodal metastasis
We then prepared multivariate models 1 (histology, tumor stage, TNM stage, and adjuvant therapy) and 2 (histology, tumor stage, TNM stage, adjuvant therapy, and NLR). AIC was calculated for OS in these models to document the prognostic role (). The results from the AIC analysis suggest that model 2 gives a better prediction of survival in patients with SCCE.
Table 5 AIC results of the two multivariate models
Discussion
Inflammation plays an important role in the development and progression of various solid tumors.Citation7,Citation8,Citation12,Citation13 Inflammatory cells within the tumor microenvironment can enhance angiogenesis, invasion, motility, and viability.Citation10,Citation14,Citation15 Cancer cells may also produce myeloid growth factors, such as granulocyte colony-stimulating factor, interleukin (IL)-1, IL-6, and tumor necrosis factor-α. These growth factors contribute to the tumor-related leukocytosis and neutrophilia.Citation16,Citation17 Research has confirmed a link between the systemic inflammatory responses and the tumor inflammatory microenvironment.Citation18,Citation19 Therefore, measurements of systemic inflammation, including NLR, may reflect the degree of host inflammatory cell activity that promotes tumor growth and progression. Several research studies have reported that NLR and other similar measures have been associated with clinical outcomes after surgery for gastroesophageal cancer.Citation20–Citation24
To the best of our knowledge, this is the first study to show NLR as an independent prognostic factor in patients with SCCE. There was a study investigating the prognostic importance of NLR in 43 patients with SCCE.Citation24 The area under the curve was 0.650 while that of the present study was 0.702. Feng et alCitation24 showed that NLR did not correlate with the prognostic factor in patients with SCCE and reported that survival rate did not differ according to NLR categories (≥3.5 and <3.5). However, this study enrolled 129 consecutive patients to evaluate the role of NLR with other clinicopathologic features in the clinical outcome of patients with surgically resected SCCE and showed that a high preoperative NLR (≥2.97 vs <2.97, P=0.004) was an indicator of poorer OS in patients with SCCE, independent of cancer stage, adjuvant therapy, and SCCE histologically with or without squamous cell carcinoma. These differences might due to a relatively larger sample in the study or a different cutoff value for NLR.
Several studies have shown NLR to be predictive of outcomes in ECs.Citation25–Citation29 However, the cutoff values for elevated NLR varied in these studies. In these studies investigating NLR in EC, the cutoff value was mean/median valueCitation25,Citation26 or was determined with ROC analysisCitation27,Citation28 or accepted as the cutoff value as in previous studies.Citation29,Citation30 The patients were classified according to a cutoff value (3.5) accepted as in a previous study by Feng et al,Citation24 whereas in the present study, the cutoff value was determined by using the ROC analysis and it was calculated to be 2.97 by using a time-dependent ROC curve. With this cutoff value, nearly half of the patients were included in the high-NLR group. Therefore, this cutoff value is considered to be useful for predicting the prognosis after esophagectomy for patients with SCCE. We chose to dichotomize NLR as ≥2.97 or <2.97 in order to be consistent with prior studies that had used the same method to determine the cutoff valueCitation27,Citation28 and found that patients with higher NLRs (≥2.97) had greater risk of death than those with lower NLRs (<2.97; HR: 1.803; 95% CI: 1.203–2.702; P=0.004). However, it is unclear whether a different cutoff value would serve as an even better predictor for survival rate, or NLRs categorized as “high,” “intermediate,” and “low” or in quartiles instead of dichotomized would be better.
This study suggested that the prognostic value of NLR in the pN0 group was more useful than that in the pN1–pN3 groups for risk stratification of patients with an elevated NLR level, but it was not satisfactory, due to the small sample in patients with N2 and N3 diseases. The data also showed that the number of lymph nodes dissected, of which the median was 8 (6–16) in this study, was sufficient for adequate nodal staging because the seventh edition of the International Union for Cancer Control and The American Joint Committee on CancerCitation11 recommends that the number of lymph nodes resected be at least six for proper nodal classification, and at least seven lymph nodes must be removed to diagnose a patient as N3 (14 and 15, respectively, in this study).
AIC was calculated to document the importance of NLR in the multivariate models. Because AIC decreased with NLR in the multivariate model, it was assumed that NLR is a meaningful predictor of survival in patients with surgically treated primary esophageal small-cell carcinoma.
This study also has certain limitations. This was a retrospective study, and this study used data from a single institution. Therefore, prospective studies involving worldwide EC centers are recommended to confirm these results in a broader population.
In conclusion, preoperative NLR is significantly associated with clinical outcomes and could be used to stratify prognosis in patients with SCCE receiving surgical treatment. It can be easily obtained from a routine examination before surgery and does not require additional cost. Preoperative NLR may be taken into consideration for the prognosis of patients with SCCE.
Disclosure
The authors alone are responsible for the writing and content of this paper. The authors report no conflicts of interest in this work.
References
- WangHHZaorskyNGMengMBMultimodality therapy is recommended for limited-stage combined small cell esophageal carcinomaOnco Targets Ther2015843744425709477
- PurwarPJiwnaniSKarimundackalGPrameshCSManagement of esophageal small cell carcinomaAnn Thorac Surg20159941488
- ShenWDengWLiNWeiCLuoSPrognostic impact of different chemotherapy strategies on small cell esophageal carcinomaZhonghua Zhong Liu Za Zhi2015371078078326813600
- DuanHZhangXWangFXPrognostic role of neutrophil-lymphocyte ratio in operable esophageal squamous cell carcinomaWorld J Gastroenterol201521185591559725987784
- ZhangJZhuZLiuYDiagnostic value of multiple tumor markers for patients with esophageal carcinomaPLoS One2015102e011695125693076
- HanLHJiaYBSongQXWangJBWangNNChengYFPrognostic significance of preoperative lymphocyte-monocyte ratio in patients with resectable esophageal squamous cell carcinomaAsian Pac J Cancer Prev20151662245225025824745
- WeiXLWangFHZhangDSA novel inflammation-based prognostic score in esophageal squamous cell carcinoma: the C-reactive protein/albumin ratioBMC Cancer20151535025934640
- KosumiKBabaYIshimotoTNeutrophil/lymphocyte ratio predicts the prognosis in esophageal squamous cell carcinoma patientsSurg Today201646440541326036223
- HiraharaNMatsubaraTHayashiHTakaiKFujiiYTajimaYImpact of inflammation-based prognostic score on survival after curative thoracoscopic esophagectomy for esophageal cancerEur J Surg Oncol201541101308131526235238
- JungJParkSYParkSJParkJPrognostic value of the neutrophil-to-lymphocyte ratio for overall and disease-free survival in patients with surgically treated esophageal squamous cell carcinomaTumour Biol20163767149715426662960
- SobinLHGospodarowiczMKWittekindCTNM Classification of Malignant Tumors7th edOxfordWiley-Blackwell2010
- LiuJSHuangYYangXFengJFA nomogram to predict prognostic values of various inflammatory biomarkers in patients with esophageal squamous cell carcinomaAm J Cancer Res2015572180218926328248
- ArigamiTOkumuraHMatsumotoMAnalysis of the fibrinogen and neutrophil-lymphocyte ratio in esophageal squamous cell carcinoma: a promising blood marker of tumor progression and prognosisMedicine (Baltimore)20159442e170226496280
- ShaoYNingZChenJPrognostic nomogram integrated systemic inflammation score for patients with esophageal squamous cell carcinoma undergoing radical esophagectomySci Rep201551881126689680
- WangJJiaYWangNThe clinical significance of tumor-infiltrating neutrophils and neutrophil-to-CD8+ lymphocyte ratio in patients with resectable esophageal squamous cell carcinomaJ Transl Med201412724397835
- FengJFHuangYChenQXPreoperative platelet lymphocyte ratio (PLR) is superior to neutrophil lymphocyte ratio (NLR) as a predictive factor in patients with esophageal squamous cell carcinomaWorld J Surg Oncol2014125824641770
- KemalYYucelIEkizKElevated serum neutrophil to lymphocyte and platelet to lymphocyte ratios could be useful in lung cancer diagnosisAsian Pac J Cancer Prev20141562651265424761879
- YuanDZhuKLiKYanRJiaYDangCThe preoperative neutrophil-lymphocyte ratio predicts recurrence and survival among patients undergoing R0 resections of adenocarcinomas of the esophagogastric junctionJ Surg Oncol2014110333334024889121
- ChenHHeJPreoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after radical resection of esophageal squamous cell carcinomaZhonghua Zhong Liu Za Zhi201436429429724989917
- WangYWangQZhangNIdentification of microRNAs as novel biomarkers for detecting esophageal squamous cell carcinoma in Asians: a meta-analysisTumour Biol20143511115951160425135426
- FengJFHuangYChenQXThe combination of platelet count and neutrophil lymphocyte ratio is a predictive factor in patients with esophageal squamous cell carcinomaTransl Oncol20147563263725389458
- XieXLuoKJHuYWangJYChenJPrognostic value of preoperative platelet-lymphocyte and neutrophil-lymphocyte ratio in patients undergoing surgery for esophageal squamous cell cancerDis Esophagus2016291798525410116
- NobleFHopkinsJCurtisNThe role of systemic inflammatory and nutritional blood-borne markers in predicting response to neoadjuvant chemotherapy and survival in oesophagogastric cancerMed Oncol201330359623690267
- FengJFHuangYZhaoQChenQXClinical significance of preoperative neutrophil lymphocyte ratio versus platelet lymphocyte ratio in patients with small cell carcinoma of the esophagusScientificWorld-Journal2013201350436524089602
- FengJFHuangYLiuJSCombination of neutrophil lymphocyte ratio and platelet lymphocyte ratio is a useful predictor of postoperative survival in patients with esophageal squamous cell carcinomaOnco Targets Ther201361605161224403837
- SatoHTsubosaYKawanoTCorrelation between the pretherapeutic neutrophil to lymphocyte ratio and the pathologic response to neoadjuvant chemotherapy in patients with advanced esophageal cancerWorld J Surg201236361762222223293
- DuttaSCrumleyABFullartonGMHorganPGMcMillanDCComparison of the prognostic value of tumour- and patient-related factors in patients undergoing potentially curative resection of oesophageal cancerWorld J Surg20113581861186621538187
- SharaihaRZHalazunKJMirzaFElevated preoperative neutrophil: lymphocyte ratio as a predictor of postoperative disease recurrence in esophageal cancerAnn Surg Oncol201118123362336921547702
- HiraharaNMatsubaraTHayashiHTakaiKNakadaSTajimaYPrognostic importance of controlling nutritional status in patients undergoing curative thoracoscopic esophagectomy for esophageal cancerAm J Ther Epub201625
- RashidFWaraichNBhattiIA pre-operative elevated neutrophil: lymphocyte ratio does not predict survival from oesophageal cancer resectionWorld J Surg Oncol20108120053279