Abstract
Purpose
Cranial nerve (CN) palsy is the main symptom in patients with locally advanced nasopharyngeal carcinoma (NPC). This study aimed to evaluate the therapeutic outcome of NPC with CN palsy and to analyze the prognostic factors.
Patients and methods
A total of 104 NPC patients with CN palsy curatively treated by conventional (n=44) or conformal (n=60) radiotherapy (RT) were enrolled. Upper CN palsy was present in 81 patients, lower CN palsy in four patients, and both upper and lower CN palsy in 19 patients. Forty-one patients had CN palsy for >2 months before diagnosis.
Results
Complete recovery of CN palsy was observed in 74 patients. The actuarial 5-year locoregional control (LRC), distant metastasis-free survival (DMFS), and overall survival (OS) rates were 58.2%, 62.2%, and 38.4%, respectively. No significant difference was observed in CN recovery, LRC, DMFS, or OS for patients treated by conventional versus conformal technique. However, significant reduction of grade 3 or greater toxicities was found in those treated by the conformal technique (odds ratio =0.28).
Conclusion
Patients with CN palsy presenting >2 months before diagnosis were hard to recover from palsy. The LRC, OS, and recovery from CN palsy did not significantly change with the treatment evolution. Patients with complete recovery from CN palsy had longer OS.
Introduction
Cranial nerve (CN) palsy is a common symptom presented in patients with locally advanced nasopharyngeal carcinoma (NPC). The tumor can extend from the nasopharynx into several foramens at the skull base and further upward to invade the cavernous sinus, therefore compressing CN II–VI and leading to diplopia, ophthalmoplegia, blindness, and trigeminal neuralgia (upper CN palsy). In addition, the tumor may invade CN IX–XI by extension into the jugular foramen or compress CN XII via the hypoglossal canal, leading to dysphagia, vocal cord palsy, sternocleidomastoid/trapezius muscle weakness, and hemiglossal paralysis (lower CN palsy). CN palsy has been recognized as a detrimental prognosticator and classified as a T4 primary tumor in the American Joint Committee on Cancer (AJCC) staging system.
Concurrent chemoradiotherapy (CCRT) is the treatment of choice for these patients, and radiotherapy (RT) plays the main role in locoregional therapy. In the past decades, the technique of RT has evolved from conventional two-dimensional RT (2DRT) into conformal RT, such as three-dimensional conformal RT (3D-CRT) and intensity-modulated RT (IMRT). The techniques of conformal RT provide better identification and delineation of the gross tumor, clinical target, or organ at risk via a computed tomography-based planning system; in addition, a more conformal distribution of dose via computer-based forward dose calculation or inverse planning algorithm can be delivered.
To determine whether the technical and dosimetric improvement of conformal therapy can directly translate into clinical benefits, such as recovery of CN palsy, reduced toxicity, increased local control, and longer survival, we retrospectively studied the therapeutic outcome of NPC patients with CN palsy treated by conventional or conformal RT and analyzed the prognostic factors.
Patients and methods
Patients
This retrospective study was approved by the Chang Gung Medical Foundation Institutional Review Board (100–0203B). The need for informed consent from patients was waived by the Chang Gung Medical Foundation Institutional Review Board because this study was non-invasive and was based only on medical records.
Between 2000 and 2007, patients with a new diagnosis of NPC with CN palsy curatively treated by conventional or conformal RT were enrolled. All patients were biopsy-proved, and three patients without pathological diagnosis of typical epidermoid carcinoma in nasopharynx were excluded. Other inclusion criteria were no previous or synchronous malignancies and age not >80 years. Two patients were excluded because they did not complete the treatment and the total RT dose was <64 Gy. There were 104 patients recruited; upper CN (II–VI) palsy was presented in 81 (77.9%) patients, lower CN (VII–XII) palsy in four (3.8%) patients, and both upper and lower in 19 (18.3%) patients. Forty-one (39.4%) patients had had CN palsy for >2 months before diagnosis. The pretreatment evaluation included a complete history and physical examination and comprehensive imaging studies, including nasopharyngoscopy, chest X-ray, magnetic resonance imaging of the head and neck, a bone scan, and an abdominal sonogram. The clinical characteristics of the patients are listed in .
Table 1 Patient characteristics (n=104)
Treatments
Among the 104 patients enrolled in this study, 44 patients were treated by conventional RT (2DRT: 4; 2DRT plus 3D-CRT: 39; 2DRT plus IMRT: 1) and 60 patients (3D-CRT: 27; 3D-CRT plus IMRT: 4; IMRT: 29) by conformal RT. The technical details of RT in our institution have been described previously.Citation1–Citation3 Briefly, the delineation of clinical target volume was mainly according to magnetic resonance imaging if available in conformal RT. The margin around clinical target volume to develop planning target volume was 3 mm three-dimensionally. The timing of adaptive re-planning was ~45–50.4 Gy in 1.8 Gy per fraction and escalated the total dose to 72 Gy or more to gross tumor and nodes. The IMRT used sequential reduced-field boost but not simultaneous integrated boost. The median dose of RT was 73.9 Gy (range 64.8–86.4 Gy). Concomitant chemotherapy was given to 78 (75%) patients. The regimen was 80–100 mg/m2 cisplatin intravenous bolus on day 1 and 800–1,000 mg/m2/24 h continuous intravenous infusion of fluorouracil without Ca folinate on days 1–4 of each cycle. Fifty-five patients (71.8%) received at least three cycles of chemotherapy before, during, and/or after the RT course. Patients did not receive concurrent chemotherapy if they had major comorbidities, poor performance status, or refusal to undergo chemotherapy.
Follow-up
Patients were regularly followed up after RT until death or last follow-up. They came back to visit the clinics at 3 months in the first 2 years and at 4–6 months in the third to fifth years. The mean follow-up duration was 46 months. Physical and nasopharyngoscopic examinations were routinely performed on each visit. Head and neck computed tomography or magnetic resonance imaging scans were performed within 2 months after RT or when clinic indications dictated. Locoregional failure was determined by pathologic diagnosis or progressive deterioration shown on consecutive image studies. Patients were examined by chest X-ray annually and by abdominal sonogram or bone scintigraphy whenever indicated to identify distant metastasis. RT toxicities such as dysphagia, aspiration pneumonia, hearing impairment, neck fibrosis, and temporal lobe necrosis were recorded.
Statistical analysis
This study uses the Kaplan–Meier method to calculate the actuarial 5-year locoregional control (LRC), distant metastasis-free survival (DMFS), and overall survival (OS) rates. LRC is defined as the date of diagnosis to tumor locoregional failure, and DMFS is defined as the date of diagnosis to distant tumor failure. OS is calculated from the date of disease diagnosis, and the censored data refer to the patients still alive at the last follow-up. The log-rank test analyzed the prognostic factors in the univariate analysis. Multivariate analysis tested all the prognostic factors of LRC, DMFS, and OS with the Cox regression model by using the forward stepwise procedure. The results of survival analyses are presented as median time or hazard ratio (HR) with 95% confidence interval (CI). The factors associated with complete recovery of CN palsy and grade 3 or greater toxicities were evaluated by the binary logistic regression models. A P-value <0.05 was considered to be statistically significant. The statistics program was SPSS 17.0 (SPSS Inc., Chicago, IL, USA).
Results
Tumor control and survival outcomes
The actuarial 5-year LRC, DMFS, and OS rates of NPC with CN palsy were 58.2%, 62.2%, and 38.4%, respectively. As for prognostic factors, we performed univariate analysis () and found that patients with a higher RT dose (≥72.0 Gy) had better LRC; in contrast, patients with age ≥60 years, histology of World Health Organization (WHO) Type I, and who did not undergo chemotherapy had poorer OS. We also found that patients with histology of WHO Type I had worse DMFS. Furthermore, all possible prognosticators were checked in the multivariate analysis, and we got the same significant prognostic factors of LRC, DMFS, and OS as for the univariate analysis (). Comparing the results of conventional versus conformal technique, we did not find any significant difference in LRC, DMFS, or OS ().
Figure 1 OS between conventional RT and conformal RT groups.
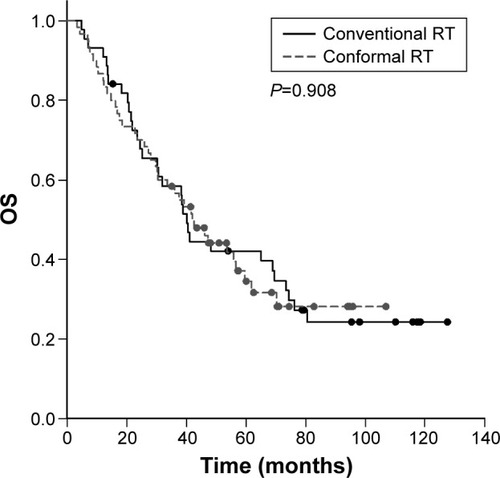
Table 2 The actuarial 5-year LRC, DMFS, and OS rates
Table 3 The prognosticators of treatment outcomes in the multivariate analysis
CN palsy
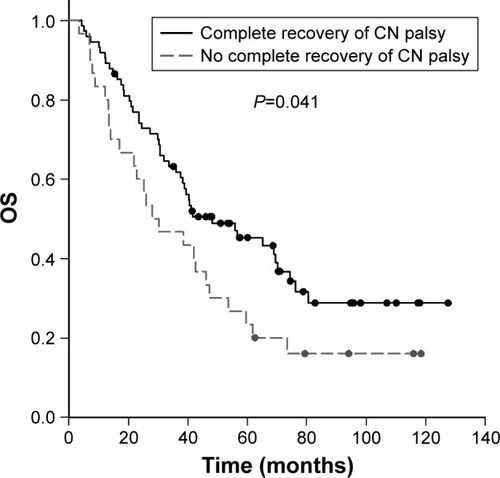
Complete recovery of CN palsy was observed in 74 patients (71.2%), and there were 49 patients (66.2%) with complete recovery before the end of the RT course. Of all the possible factors, an interval of CN palsy >2 months before diagnosis was the only independent adverse prognosticator for the complete recovery of CN palsy following treatment (43.9% versus 88.9%, P<0.001), which was confirmed in the multivariate analysis (odds ratio =0.10, 95% CI =0.04–0.27, P<0.001). We did not observe a significant difference in the complete recovery of CN palsy for patients treated by the conventional versus conformal technique (77.3% versus 66.7%, P=0.238). If patients could completely recover from CN palsy, they would have a better 5-year OS rate (45.2% versus 23.3%, P=0.041) ().
Late toxicities
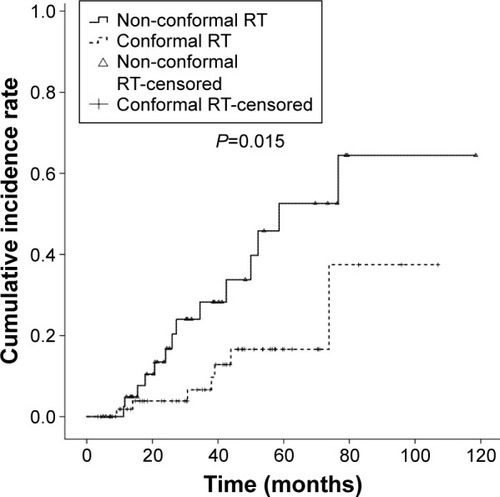
Twenty-one patients (20.2%) suffered from severe (grade 3 or greater) late toxicities, retrospectively graded according to the Common Terminology Criteria for Adverse Events version 4.0. Of these patients with severe toxicities, 14 patients underwent conventional RT and seven patients received the conformal technique. Six patients had suffered from dysphagia requiring tube feeding, and the respective distribution for the conventional RT group compared with the conformal RT group was four versus two. There were four patients with aspiration pneumonia, and the distribution for the conventional RT group compared with the conformal RT group was one versus three. Eight patients had hearing impairment requiring hearing aids, and six of them were in the conventional RT group while two were in the conformal RT group. There were six patients with severe neck fibrosis requiring rehabilitation (four in the conventional RT group versus two in the conformal RT group) and nine patients with temporal lobe necrosis (seven in the conventional RT group versus two in the conformal RT group).
The cumulative incidence rate of toxicity in the conventional group was significantly higher than that of patients in the conformal group (). In the multivariate analysis of all possible prognosticators, we found that the conformal RT technique could significantly reduce the occurrence of severe toxicities (odds ratio =0.28, 95% CI =0.10–0.78, P=0.014).
Discussion
Several studies have reported the therapeutic outcomes of NPC with CN palsy in English literature. However, some of these studies were small population reports,Citation4,Citation5 and some were published in the conventional 2DRT era.Citation6–Citation10 Some studies were published in the last decade but comprised patients mainly treated by conventional 2DRT.Citation11–Citation14 To our knowledge, this study is the first clinical report to date to evaluate the difference between the therapeutic outcomes of NPC with CN palsy treated by conformal RT (57.7%) and conventional RT (42.3%).
In our study, 77.9% of patients had upper CN palsy but not lower CN palsy at initial diagnosis. This phenomenon demonstrated the anatomically upward extension of the tumor into the pterygopalatine fossa and further invasion of the cavernous sinus. The prevalence of upper CN palsy in this study was compatible with the reports of other studies. Mo et alCitation14 reported upper CN palsy in 78.7% of patients in southern China, and Chang et alCitation11 reported the similar result of 81.2% of patients in northern Taiwan. Both Li et alCitation12 and Liu et alCitation13 pointed out that CN V and CN VI were the major lesion sites. On the other hand, our study found that few patients (3.8%) suffered from lower CN palsy, which was similar to other reports (<10% of patients) presented by Mo et alCitation14 and Chang et alCitation11 (). The low prevalence of lower CN palsy actually reflected the tumor location anatomically far away from the jugular foramen and hypoglossal canal.
Table 4 Therapeutic outcome analysis of NPC with CN palsy
The 5-year actuarial LRC and OS rates in this study were 58.2% and 38.4%, respectively, which were very similar to the results reported by Chang et al,Citation11 but worse than the results reported by Mo et al.Citation14 Therapeutic outcome seemed to have no improvement with the evolution of the RT technique from conventional RT to conformal RT, since conformal RT comprised 57.7% in our study versus 18.0% in the study reported by Mo et alCitation14 and 0% in the study reported by Chang et al.Citation11 Furthermore, there were no significant differences in LRC, DMFS, and OS between conventional and conformal RT. This phenomenon depicted the locally advanced nature of the primary tumor invasion despite the use of the newer RT technique. The similar LRC could be contributed to by the much larger treatment fields in conventional 2DRT than those in conformal RT. On the other hand, the non-inferiority result of LRC indicated that conformal RT with a lower volume of high RT dose to nearby tissue did not influence tumor control.
The evolution of RT technique did not directly translate into a better LRC in our study, but we found that patients with a higher RT dose had a better LRC. This result depicted the large volume of these locally advanced tumors requiring higher dose escalation. As for other prognosticators of primary tumor control, Chang et alCitation11 reported that imaging modality, CN palsy area, and complete recovery of CN palsy were significant factors for local control, and Mo et alCitation14 found that recovery duration was the only significant prognosticator for local relapse-free survival. Nevertheless, both complete recovery of CN palsy and recovery duration were post-treatment factors. The few pretreatment prognosticators correlated to primary tumor control in the studies were owing to a locally advanced entity in these clinical T4 tumors.
In this study, chemotherapy was one of the significant prognosticators for OS. The role of concurrent chemotherapy in locally advanced NPC had been established since a Phase III study published by Lin et alCitation15 in 2003, which demonstrated that patients with concurrent chemotherapy had better OS and progression-free survival but both regional control and distant control had no significant difference. Our study result also emphasized the importance of concurrent chemotherapy in these patients with CN palsy. Similarly, we considered that the survival benefit from chemotherapy might be due to the radio-enhancing effect since patients with chemotherapy did not have better DMFS but with longer LRC even though it is not significant. Concurrent chemotherapy with RT had been a gold standard treatment for these patients.
As for other prognosticators of OS, the poor OS in older patients might be owing to more comorbidities and worse general condition than younger patients. The histology of WHO Type I was rare in endemic Asians and less radio-responsive, which might lead to poor LRC.Citation16,Citation17 Our study also found that patients with histology of WHO Type I had poor OS.
Different studies reported different treatment outcomes of complete recovery of CN palsy. Chang et alCitation11 and Li et alCitation12 reported similar complete recovery rates of 51.8% and 58%, respectively. Mo et alCitation14 reported that most patients could have complete recovery. In this study, we found that 71.2% of patients had complete recovery of CN palsy, and a pretreatment duration of CN palsy (2 months) associated with complete recovery. We also demonstrated that patients with complete recovery from cranial palsy would have better OS. Some studiesCitation12,Citation14 also demonstrated the importance of pretreatment duration of CN palsy for complete recovery. In the study reported by Mo et al,Citation14 recovery duration within or beyond 6 months was a significant prognosticator not only for local relapse-free survival and disease-free survival but also for disease-specific survival and OS.
Toxicity from RT was a major concern because of the large treatment volumes covering these locally advanced tumors. There were no previous studies focusing on whether the evolution of the RT technique from conventional to conformal technique could reduce RT toxicity in these patients. This was the first study to demonstrate that conformal RT could significantly reduce severe late toxicities in NPC patients with CN palsy. This result was compatible with our previous studies about quality of life in general NPC patients.Citation1–Citation3,Citation18
Conclusion
This retrospective cohort study depicted that the recovery of CN palsy, LRC, and survival in NPC patients with CN palsy did not significantly change with treatment evolution from a conventional to conformal technique despite a greater reduction of toxicities. Our study also demonstrated an interval of CN palsy >2 months before diagnosis as a significant adverse prognosticator for complete recovery of CN palsy. Considering the limitation of a retrospective study, further prospective studies are needed to confirm our results.
Disclosure
The authors report no conflicts of interest in this work.
References
- FangFMTsaiWLChenHCIntensity-modulated or conformal radiotherapy improves the quality of life of patients with nasopharyngeal carcinoma: comparisons of four radiotherapy techniquesCancer2007109231332117154159
- FangFMChienCYTsaiWLQuality of life and survival outcome for patients with nasopharyngeal carcinoma receiving three-dimensional conformal radiotherapy vs. intensity-modulated radiotherapy-a longitudinal studyInt J Radiat Oncol Biol Phys200872235636418355980
- FangFMTsaiWLLeeTFLiaoKCChenHCHsuHCMultivariate analysis of quality of life outcome for nasopharyngeal carcinoma patients after treatmentRadiother Oncol201097226326920817290
- HuangHIChanKTShuCHHoCYT4-locally advanced nasopharyngeal carcinoma: prognostic influence of cranial nerve involvement in different radiotherapy techniquesScientificWorldJournal2013201343907324385882
- YapMLChooBAChanYHLuJJMun LeeKThamIWOutcomes following treatment for patients with cranial nerve involvement from nasopharyngeal cancerJ Med Imaging Radiat Oncol201256554855323043575
- StillwagonGBLeeDJMosesHKashimaHHarrisAJohnsMResponse of cranial nerve abnormalities in nasopharyngeal carcinoma to radiation therapyCancer19865712227222743008979
- ChenMSLinFJTangSGLeungWMLeungWClinical significance of cranial nerve deficit in the therapy of nasopharyngeal carcinomaBr J Radiol1989627407397432504432
- ShamJSCheungYKChoyDChanFLLeongLCranial nerve involvement and base of the skull erosion in nasopharyngeal carcinomaCancer19916824224262070338
- OzyarEAtahanILAkyolFHGurkaynakMZorluAFCranial nerve involvement in nasopharyngeal carcinoma: its prognostic role and response to radiotherapyRadiat Med199412265688079005
- TurgutMErturkOSaygiSOzcanOEImportance of cranial nerve involvement in nasopharyngeal carcinoma. A clinical study comprising 124 cases with special reference to clinical presentation and prognosisNeurosurg Rev199821424324810068184
- ChangJTLinCYChenTMNasopharyngeal carcinoma with cranial nerve palsy: the importance of MRI for radiotherapyInt J Radiat Oncol Biol Phys20056351354136016297716
- LiJCMayrNAYuhWTWangJZJiangGLCranial nerve involvement in nasopharyngeal carcinoma: response to radiotherapy and its clinical impactAnn Otol Rhinol Laryngol2006115534034516739664
- LiuLLiangSLiLPrognostic impact of magnetic resonance imaging-detected cranial nerve involvement in nasopharyngeal carcinomaCancer200911591995200319235251
- MoHYSunRSunJPrognostic value of pretreatment and recovery duration of cranial nerve palsy in nasopharyngeal carcinomaRadiat Oncol2012714922958729
- LinJCJanJSHsuCYLiangWMJiangRSWangWYPhase III study of concurrent chemoradiotherapy versus radiotherapy alone for advanced nasopharyngeal carcinoma: positive effect on overall and progression-free survivalJ Clin Oncol200321463163712586799
- ReddySPRaslanWFGooneratneSKathuriaSMarksJEPrognostic significance of keratinization in nasopharyngeal carcinomaAm J Otolaryngol19951621031087540805
- MarksJEPhillipsJLMenckHRThe National Cancer Data Base report on the relationship of race and national origin to the histology of nasopharyngeal carcinomaCancer19988335825889690553
- FangFMChiuHCKuoWRHealth-related quality of life for nasopharyngeal carcinoma patients with cancer-free survival after treatmentInt J Radiat Oncol Biol Phys200253495996812095563