Abstract
Purpose
Aberrant activation of the Janus-associated kinase (JAK)/signal transducer and activator of transcription (STAT) pathway is associated with increased malignant cell proliferation and survival. This Phase Ib study evaluated ruxolitinib, a potent JAK1/2 inhibitor, in combination with gemcitabine with or without nab-paclitaxel in patients with advanced solid tumors.
Patients and methods
Patients received ruxolitinib + gemcitabine (regimen A) or ruxolitinib + gemcitabine + nab-paclitaxel (regimen B). The objective of the dose-finding phase was to identify the maximum tolerated doses (MTDs) of ruxolitinib plus gemcitabine with or without nab-paclitaxel.
Results
Among 42 patients enrolled, the median age was 62.5 years, 81.0% had pancreatic cancer, and almost 62% had received prior systemic therapy. Regimen A was tolerated with standard doses of gemcitabine; regimen B was tolerated with reduced doses of gemcitabine/nab-paclitaxel or concomitant granulocyte colony-stimulating factor. The sponsor decided to terminate the study early due to the interim analysis results of the Phase III JANUS 1 study. Discontinuations were mainly due to radiologic or clinical disease progression (81.0% of patients). Median treatment durations were 55.5 days (cohort A0) and 150.5 days (pooled B cohorts). Four patients (pooled B cohorts) had dose-limiting toxicities: grade 3 pneumonia (n=1), grade 4 neutropenia (n=1), and grade 4 thrombocytopenia (n=2). The most common grade 3/4 hematologic adverse events (AEs) were anemia, thrombocytopenia, and neutropenia. Serious AEs occurring in ≥2 patients in cohort A0 or pooled B cohorts were abdominal pain, sepsis (cohort A0), dehydration, anemia, and asthenia (pooled B cohorts). Overall response rates (ORRs) were 12.5% in cohort A0 and 38.5% in pooled B cohorts. Among patients with pancreatic cancer, ORR was 23.5% (14.0% cohort A0 30.0% pooled B cohorts).
Conclusion
The study was terminated early prior to reaching MTDs per sponsor decision; although ruxolitinib plus gemcitabine with or without nab-paclitaxel was generally safe and well tolerated in patients with advanced solid tumors, this combination will not be pursued further.
Keywords:
Introduction
The Janus-associated kinase (JAK) family comprises 4 non-receptor protein tyrosine kinases (JAK1–3 and tyrosine kinase 2) that transduce cytokine-mediated signaling via the JAK/signal transducer and activator of transcription (STAT) pathway.Citation1 Aberrant activation of this pathway is associated with increased malignant cell proliferation and survivalCitation1,Citation2 and has been observed in various tumor types.Citation3–Citation5 Furthermore, JAK kinases are key mediators of downstream signaling for various cytokine and/or growth factor receptors that play a role in systemic inflammation, leading to cancer cachexia that increases cancer-associated morbidity and mortality.Citation1,Citation6–Citation8
Ruxolitinib, an orally bioavailable, potent, and selective inhibitor of JAK1 and 2 enzymes, has been approved by the US Food and Drug Administration and European Medicines Agency for the treatment of intermediate- to high-risk primary or secondary myelofibrosis.Citation9,Citation10 By selectively inhibiting JAK2 V617F, STAT5, and ERK1/2 phosphorylation, ruxolitinib reduces cellular proliferation and induces apoptosis of JAK2 V617F Ba/F3 cells.Citation11 Ruxolitinib has also been shown to possess activity in solid tumors. In a previous Phase II study of Ruxolitinib in Pancreatic Cancer Patients (RECAP), early evidence of ruxolitinib in combination with capecitabine suggested an association with improved survival compared with placebo and capecitabine in a subset of patients with metastatic pancreatic cancer and systemic inflammation, evidenced by elevated C-reactive protein levels.Citation12
In addition to approvals in other solid tumor settings, gemcitabine is indicated as a single agent for pancreatic cancer and in combination with nab-paclitaxel as a first-line treatment for metastatic adenocarcinoma of the pancreas;Citation13,Citation14 however, myelosuppression is a common and sometimes dose-limiting adverse event (AE) associated with both gemcitabine and nab-paclitaxel.Citation13,Citation14 Ruxolitinib has demonstrated the ability to reduce levels of pro-inflammatory cytokines (thought to be associated with the development of cachexia) in patients with myelofibrosis.Citation15–Citation17 Ruxolitinib is generally known to be well tolerated and may augment the activity of gemcitabine in patients with pancreatic cancer. Indeed, in a murine model of pancreatic cancer, the combination of gemcitabine plus a JAK2 inhibitor (fedratinib) substantially reduced the rate of tumor growth and significantly improved overall survival compared with either agent alone.Citation18 Overlapping hematologic toxicities associated with gemcitabine and ruxolitinib may be a concern clinically.
The current Phase Ib, dose-finding study was conducted to evaluate the safety and tolerability of ruxolitinib in combination with gemcitabine with or without nab-paclitaxel in patients with advanced pancreatic cancer and other advanced solid tumors. Our study was terminated early by the sponsor after an interim analysis from a Phase III trial of ruxolitinib plus capecitabine (JANUS 1) showed no additional benefit over capecitabine alone in patients with advanced pancreatic cancer and high systemic inflammation as measured by the modified Glasgow prognostic score.Citation19
Patients and methods
Patients
Eligible patients were aged ≥18 years, had radiographically measurable advanced or metastatic pancreatic adenocarcinoma or another advanced solid tumor, and an Eastern Cooperative Oncology Group (ECOG) performance status of ≤1.
The study was conducted in accordance with the study protocol, Declaration of Helsinki, Good Clinical Practices as defined in the Code of Federal Regulations Title 21, International Conference of Harmonisation – Good Clinical Practice consolidated guidelines, and applicable regulatory requirements. All patients provided written informed consent before study participation. The study protocol and its amendments and patients’ informed consent were reviewed and approved by institutional review boards or independent ethics committees (IntegReview Ethical Review Board, Austin, TX, USA; Western Institutional Review Board, Puyallup, WA, USA; Western Institutional Review Board, Olympia, WA, USA; and Duke University Health System Institutional Review Board, Durham, NC, USA).
Study design
The Phase Ib open-label study (NCT1822756) was designed to be conducted in 2 parts. Part 1 comprised a dose-finding phase to identify the maximum tolerated dose (MTD) of ruxolitinib when administered with gemcitabine with or without nab-paclitaxel to patients with advanced or metastatic pancreatic cancer and other advanced solid tumors; safety, tolerability, and pharmacokinetics would be assessed in part 1. Part 2 was to explore the safety, tolerability, pharmacokinetics, pharmacodynamics, and preliminary clinical activity of ruxolitinib, at the dose identified in part 1, in combination with gemcitabine with or without nab-paclitaxel. Part 2 of the study was not conducted following a sponsor decision not to pursue the combinations of ruxolitinib + gemcitabine or ruxolitinib + gemcitabine/nab-paclitaxel, and therefore, to stop further enrollment during part 1 before the MTD was reached.
Part 1 was a 3 + 3 dose-finding design in which patients were assigned to 1 of 2 treatment regimens, regimen A or B, based on prior chemotherapy exposure (). Patients who had received no more than 1 prior chemotherapy regimen for advanced or metastatic disease (excluding neoadjuvant or adjuvant disease) were eligible to receive ruxolitinib + gemcitabine (regimen A). Patients who had not received prior chemotherapy for advanced or metastatic disease (excluding neoadjuvant or adjuvant disease) were eligible to receive ruxolitinib + gemcitabine + nab-paclitaxel (regimen B).
Figure 1 Study design.a
Abbreviations: BID, twice daily; GCSF, granulocyte colony-stimulating factor; IV, intravenous; PO, orally; Q28D, every 28 days.
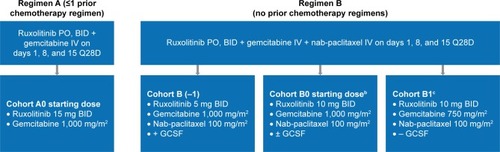
The first patients enrolled to regimen A were assigned to the starting dose cohort A0, consisting of ruxolitinib 15 mg twice daily (BID) and gemcitabine 1,000 mg/m2 on days 1, 8, and 15 every 28 days (Q28D). The first patients enrolled to regimen B were assigned to the starting dose cohort B0, consisting of ruxolitinib 10 mg BID, gemcitabine 1,000 mg/m2, and nab-paclitaxel 100 mg/m2 on days 1, 8, and 15 Q28D. Cohort B0 administered with prophylactic granulocyte colony-stimulating factor (GCSF) support could be repeated in patients with pancreatic cancer if any of the dose-limiting toxicities (DLTs) observed were due to myelosuppression. If a DLT was observed in 1 patient, then that cohort was expanded to at least 6 patients. If no additional DLTs were observed in those 3 additional patients, then dose finding could proceed or result in cohort expansion. If a DLT occurred in 2 patients or more of the total cohort, then the MTD was deemed to be exceeded, and the lower dose level was to be expanded to at least 6 patients to evaluate safety. If the regimen in cohort B0 was not tolerated, then an additional cohort (B1) was added to test a reduced dose of gemcitabine at 750 mg/m2, without the addition of prophylactic GCSF support. In addition, ruxolitinib 5 mg BID, gemcitabine 1,000 mg/m2, and nab-paclitaxel 100 mg/m2 on days 1, 8, and 15 Q28D were tested in cohort B (−1) to evaluate the effects of GCSF with the expectation of re-escalating doses.
Treatment for all patients in regimens A and B consisted of repeating 28-day cycles, with treatment cycles continuing for as long as the regimen was tolerated and the patient did not meet discontinuation criteria. The expected duration was ~4–6 months.
End points
The primary end points were the determination of the MTD of ruxolitinib in combination with gemcitabine with or without nab-paclitaxel, and the safety and tolerability of the treatment regimens. Secondary end points were pharmacokinetics and pharmacodynamics. Because of the early termination of the study, samples for pharmacokinetics and pharmacodynamics, and computed tomography for tumor burden were collected but not analyzed. The exploratory end point was antitumor effects assessed as overall response rate (ORR).
Assessments and statistical methods
Safety and tolerability were assessed by monitoring AEs, measuring vital signs and 12-lead electrocardiograms, and evaluating physical examinations and clinical laboratory blood tests. The severity of AEs was graded using the National Cancer Institute Common Terminology Criteria for AEs v4.03. Safety data were compared over time to assess change from baseline, during treatment, and follow-up. The safety population, including all enrolled patients who received at least 1 dose of ruxolitinib (treatment group defined according to actual treatment received regardless of assigned study drug treatment), was used for all safety analyses. Response was determined by radiographic disease assessments per Response Evaluation Criteria in Solid Tumors version 1.1Citation20 by investigator assessment and was exploratory in nature with descriptive statistics (eg, mean, standard deviation, and range) provided. The intent-to-treat (ITT) population, including all patients who received at least 1 dose of ruxolitinib (treatment group defined according to assigned treatment regardless of actual study drug received), was used for all efficacy analyses.
Results
Patients
A total of 42 patients with advanced solid tumors (predominantly pancreatic cancer; 81.0%) were enrolled in part 1 of the study (ITT and safety population; ). The median age at the time of enrollment was 62.5 years, and all patients had an ECOG performance status of either 0 (57.1%) or 1 (42.9%) at baseline. Almost 62% of patients had received prior systemic therapy for their primary cancer; ~19% had received prior gemcitabine; and ~40% had received prior radiation therapy. Of the 16 patients who had received prior radiation therapy, 8 received radiation therapy at the same time as chemotherapy as an add-on, 3 received neoadjuvant radiation therapy, and 5 received adjuvant radiation therapy.
Table 1 Patient demographics and baseline characteristics
Exposure, safety, and efficacy
MTD and exposure
Ruxolitinib + gemcitabine (regimen A) was tolerated with standard doses of gemcitabine (1,000 mg/m2). Ruxolitinib + gemcitabine/nab-paclitaxel (regimen B) was tolerated with reduced doses of gemcitabine (750 mg/m2)/nab-paclitaxel (100 mg/m2) or with concomitant GCSF. MTDs were not defined, as the study was terminated after cohort B1 when the sponsor decided not to pursue these combinations further based on the interim results from another Phase III trial.
A total of 40 patients (95.2%) discontinued treatment, primarily due to radiologic or clinical disease progression (n=34 [81.0%]; ). Other reasons included AE (7.1%), death (4.8%), and patient decision (2.4%). Overall, the median duration of ruxolitinib exposure was 97.5 days (55.5 days in cohort A0; 150.5 days in the pooled B cohorts); a median of 8.5 (range, 1–46) intravenous gemcitabine treatments were administered.
Table 2 Patient disposition
Safety
There were no DLTs experienced in cohort A0. Four patients in the B0 cohorts experienced DLTs; 2 patients from cohort B0 without GCSF, including 1 case of grade 4 neutropenia, 1 case of grade 4 thrombocytopenia, and 2 patients from cohort B0 with GCSF, including a serious event of grade 3 pneumonia (which resolved with treatment 6 days after onset) and 1 case of grade 4 thrombocytopenia.
All patients experienced at least 1 treatment-emergent AE (TEAE), with the most common nonhematologic TEAEs of any grade (occurring in ≥50% of patients in cohort A or pooled B cohorts) being fatigue, nausea, alopecia, and peripheral edema (). A lower percentage of infections and infestations occurred in patients who did not receive GCSF compared with patients who did receive GCSF (28.6% vs 57.1%). Grade 3/4 TEAEs were reported in >80% of patients in both cohort A0 and pooled B cohorts. The most common grade 3/4 nonhematologic AEs (occurring in ≥10% of patients in cohort A or pooled B cohorts) were abdominal pain, fatigue, sepsis, and hypokalemia (); the most common grade 3/4 hematologic AEs (new/worsening laboratory abnormalities occurring in ≥10% of patients in cohort A or pooled B cohorts) were anemia, thrombocytopenia, and neutropenia ().
Table 3 Most common treatment-emergent nonhematologic adverse events
Table 4 Worsening of hematologic toxicity
Treatment-emergent serious AEs (SAEs) were experienced in 62.5% of patients in cohort A and 34.6% of patients in pooled B cohorts. Treatment-emergent SAEs occurring in ≥2 patients in either cohort A or pooled B cohorts were abdominal pain (25% cohort A0), sepsis (12.5% cohort A0), dehydration, anemia, and asthenia (7.7% each, pooled B cohorts). One death occurred in cohort A0 due to sepsis (without neutropenia), which was not considered related to ruxolitinib; no deaths occurred in pooled B cohorts.
Efficacy
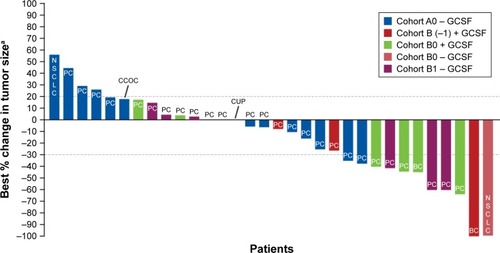
ORRs were 12.5% (2/16) in cohort A0 and 38.5% (10/26) in the pooled B cohorts (). Among the patients with pancreatic cancer, ORR was 23.5% (14.0% in cohort A0 and 30.0% in pooled B cohorts). A complete response (CR) occurred in 1 patient (2.4%) overall with non-small cell lung cancer in cohort B0 without GCSF, and a partial response (PR) occurred in 11 patients overall (26.2%). Among patients who achieved a PR, the median duration of response ranged from 33.0 days in cohort B (−1) to 225.0 days in cohort B1. The majority of PRs (82.0%) occurred in patients treated with ruxolitinib for a median of >140 days. Clinical benefit rate (ORR + stable disease for ≥7 weeks) was 37.5% (6/16) in cohort A0 and 73.0% (19/26) for the pooled B cohorts. The largest percentage reduction of target lesions occurred in a patient with PR in cohort B (−1) and in a patient with CR in cohort B0 ().
Table 5 Tumor response
Figure 2 Waterfall plot of best percent change in sum of target lesions (ITT population).
Abbreviations: BC, breast cancer; CCOC, clear cell odontogenic cancer; CUP, cancer of unknown primary (likely gallbladder); GCSF, granulocyte colony-stimulating factor; ITT, intent-to-treat; NSCLC, non-small cell lung cancer; PC, pancreatic cancer.
Discussion
In patients with chemotherapy-naive metastatic pancreatic adenocarcinoma, the combination of gemcitabine and nab-paclitaxel has previously demonstrated improved survival and tumor response compared with gemcitabine alone; however, this combination was also found to increase the rates of peripheral neuropathy and myelosuppression observed.Citation21,Citation22 In the Phase II RECAP study in patients with metastatic pancreatic cancer who had failed prior gemcitabine therapy, the combination of ruxolitinib and capecitabine demonstrated clinical activity, especially in patients with systemic inflammation, evidenced by elevated C-reactive protein levels.Citation12 These results suggest that the modulation of inflammatory cytokine signaling may be important in these patients and highlight a potential role for JAK inhibition as a therapeutic target.Citation12
The combination of ruxolitinib and gemcitabine, with and without nab-paclitaxel, in patients with advanced solid tumors, 81% of whom had pancreatic cancer, at the doses investigated were generally safe and well tolerated. The combination of ruxolitinib and gemcitabine was tolerated with standard doses of gemcitabine; however, the combination of ruxolitinib, gemcitabine, and nab-paclitaxel was tolerated with reduced doses of gemcitabine/nab-paclitaxel or with concomitant GCSF. Dose reductions of gemcitabine and/or nab-paclitaxel were required in up to 47% of patients in the pivotal study of gemcitabine versus gemcitabine plus nab-paclitaxel in patients with metastatic pancreatic cancer, and 15%–26% of patients received growth factor support.Citation22 Although the overall number of patients treated was relatively small and any results from a comparison between groups must be interpreted with caution, the addition of GCSF to the ruxolitinib combination suggested no apparent clinical advantage, as a higher percentage of patients in cohorts receiving GCSF reported more infections than cohorts who did not receive GCSF. The most frequently reported TEAE was fatigue, which occurred in at least 50% of patients across all cohorts, and the most frequently reported grade ≥3 TEAEs were anemia, thrombocytopenia, and neutropenia, consistent with the prescribing information for ruxolitinib.Citation9,Citation10 In 2 randomized double-blind Phase III trials, JANUS 1 and JANUS 2, ruxolitinib, when combined with capecitabine, also had a reasonably well-tolerated safety profile in patients with refractory advanced/metastatic pancreatic cancer. However, the addition of ruxolitinib to capecitabine did not improve clinical or quality of life outcomes, and the studies were terminated early based on efficacy findings of the planned interim analysis of JANUS 1.Citation19
In our study, objective responses were noted in 23.5% of 34 patients with pancreatic cancer. These results correlate well with response rates determined from recent studies in patients with advanced/metastatic pancreatic cancer (7%–35%) depending on the treatment regimen used.Citation22–Citation27
Conclusion
In this Phase I study of ruxolitinib in combination with gemcitabine with or without nab-paclitaxel in patients with advanced solid tumors, assessment of the safety data revealed that no new safety concerns were identified, and the doses investigated were generally well tolerated. The study was terminated early prior to reaching the MTDs per sponsor decision. The combinations of ruxolitinib and gemcitabine or ruxolitinib, gemcitabine, and nab-paclitaxel will not be pursued further.
Acknowledgments
This study was supported by Incyte Corporation. Medical writing assistance was provided by Jordana Campbell, part of Evidence Scientific Solutions, Inc, Philadelphia, PA, USA, and was funded by Incyte Corporation. AF-T has received research funding from Incyte (Inst) and Celgene (Inst). TJG Jr is a consultant for Merck and Bayer. AA has received research funding and royalties from Incyte. HH has received research funding from Incyte (Inst).
Disclosure
Both AA and YD are employees of Incyte Corporation and have stock ownership. The authors report no other conflicts of interest in this work.
References
- ThomasSJSnowdenJAZeidlerMPDansonSJThe role of JAK/STAT signalling in the pathogenesis, prognosis and treatment of solid tumoursBr J Cancer2015113336537126151455
- Quintás-CardamaAKantarjianHCortesJVerstovsekSJanus kinase inhibitors for the treatment of myeloproliferative neoplasias and beyondNat Rev Drug Discov201110212714021283107
- CortasTEisenbergRFuPKernJPatrickLDowlatiAActivation state EGFR and STAT-3 as prognostic markers in resected non-small cell lung cancerLung Cancer200755334935517161498
- KomazakiTNagaiHEmiMHypermethylation-associated inactivation of the SOCS-1 gene, a JAK/STAT inhibitor, in human pancreatic cancersJpn J Clin Oncol200434419119415121754
- TamLMcGlynnLMTraynorPMukherjeeRBartlettJMEdwardsJExpression levels of the JAK/STAT pathway in the transition from hormone-sensitive to hormone-refractory prostate cancerBr J Cancer200797337838317595657
- CarsonJABaltgalvisKAInterleukin 6 as a key regulator of muscle mass during cachexiaExerc Sport Sci Rev201038416817620871233
- EvansWJMorleyJEArgilésJCachexia: a new definitionClin Nutr200827679379918718696
- MondelloPLacquanitiAMondelloSEmerging markers of cachexia predict survival in cancer patientsBMC Cancer20141482825400234
- JAKAFI® (ruxolitinib) [prescribing information]Wilmington, DE, USAIncyte Corporation2016
- JAKAVI® (ruxolitinib) [summary of product characteristics]Camberley, UKNovartis Europharm Limited2016
- Quintás-CardamaAVaddiKLiuPPreclinical characterization of the selective JAK1/2 inhibitor INCB018424: therapeutic implications for the treatment of myeloproliferative neoplasmsBlood2010115153109311720130243
- HurwitzHIUppalNWagnerSARandomized, double-blind, phase II study of ruxolitinib or placebo in combination with capecitabine in patients with metastatic pancreatic cancer for whom therapy with gemcitabine has failedJ Clin Oncol201533344039404726351344
- ABRAXANE® (nab-paclitaxel) [prescribing information]Summit, NJ, USACelgene Corporation2015
- GEMZAR® (gemcitabine) [prescribing information]Indianapolis, IN, USALilly USA2017
- HarrisonCKiladjianJJAl-AliHKJAK inhibition with ruxolitinib versus best available therapy for myelofibrosisN Engl J Med2012366978779822375970
- VerstovsekSKantarjianHMesaRASafety and efficacy of INCB018424, a JAK1 and JAK2 inhibitor, in myelofibrosisN Engl J Med2010363121117112720843246
- VerstovsekSMesaRAGotlibJA double-blind, placebo-controlled trial of ruxolitinib for myelofibrosisN Engl J Med2012366979980722375971
- WormannSMSongLAiJLoss of P53 function activates JAK2-STAT3 signaling to promote pancreatic tumor growth, stroma modification, and gemcitabine resistance in mice and is associated with patient survivalGastroenterology20161511180193.e1227003603
- HurwitzHVan CutsemEBendellJCTwo randomized, placebo-controlled phase 3 studies of ruxolitinib (Rux) + capecitabine (C) in patients (pts) with advanced/metastatic pancreatic cancer (mPC) after failure/intolerance of first-line chemotherapy: JANUS 1 (J1) and JANUS 2 (J2)J Clin Oncol2017354 Suppl34327918718
- EisenhauerEATherassePBogaertsJNew response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1)Eur J Cancer200945222824719097774
- GoldsteinDEl-MaraghiRHHammelPnab-Paclitaxel plus gemcitabine for metastatic pancreatic cancer: long-term survival from a phase III trialJ Natl Cancer Inst20151072dju41325638248
- Von HoffDDErvinTArenaFPIncreased survival in pancreatic cancer with nab-paclitaxel plus gemcitabineN Engl J Med2013369181691170324131140
- BendellJO’ReillyEMMiddletonMRPhase I study of olaparib plus gemcitabine in patients with advanced solid tumours and comparison with gemcitabine alone in patients with locally advanced/metastatic pancreatic cancerAnn Oncol201526480481125573533
- IkedaMSatoAMochizukiNPhase I trial of GBS-01 for advanced pancreatic cancer refractory to gemcitabineCancer Sci2016107121818182427685612
- SteinSMJamesESDengYFinal analysis of a phase II study of modified FOLFIRINOX in locally advanced and metastatic pancreatic cancerBr J Cancer2016114773774327022826
- WadaKSanoKAmanoHBiweekly gemcitabine plus S-1 for locally advanced and metastatic pancreatic cancer: a preliminary feasibility studyJ Hepatobiliary Pancreat Sci201522969269826136371
- YamaueHSatoiSKanbeTPhase II clinical study of alternate-day oral therapy with S-1 as first-line chemotherapy for locally advanced and metastatic pancreatic cancerCancer Chemother Pharmacol20147319710224146260
