Abstract
Bone metastases often create serious clinical problems: they lead to poor performance status due to pathologic fractures, spinal cord compression and intractable pain, commonly referred to as skeletal-related events. The receptor activator of nuclear factor-κB (RANK), the RANK ligand (RANKL), and osteoprotegerin, a decoy receptor for RANK, regulate osteoclastogenesis and may play a key role in bone metastasis. Denosumab (XGEVA; Amgen, Thousand Oaks, CA), a fully human monoclonal antibody that binds to and neutralizes RANKL, inhibits osteoclast function, prevents generalized bone resorption and local bone destruction, and has become a therapeutic option for preventing or delaying first on-study skeletal-related events in various malignancies. In the context of urological cancer, three main Phase III clinical studies have been published in prostate cancer. This article provides a brief overview of the characteristics of bone metastasis in urological cancers, reviews the mechanisms of bone metastasis, including the RANK/RANKL/osteoprotegerin axis, the current standard of care, zoledronic acid, and describes the efficacy of the novel bone-targeted agent denosumab in bone metastasis. Denosumab is emerging as a key therapeutic option in the treatment of bone metastases from urological cancers.
Introduction
Bone is a major metastatic site for many solid tumors. Indeed, after lung and liver, bone is the most common metastatic site for up to 70% of advanced breast and prostate cancer and for approximately 15% to 30% of lung, colon, gastric, bladder, uterus, rectal, thyroid cancer, or renal cell cancer (RCC).Citation1–Citation3 Bone seems to provide an ideal microenvironment in which metastatic cancer cells can thrive. When luciferase-labeled cancer cells are introduced into animals by intracardiac injection, they initially appear as diffuse photon accumulations throughout the body, become completely undetectable after 6 hours, and subsequently form bone metastases (). Bone metastases often create serious clinical problems; they lead to poor performance status due to pathologic fractures, spinal cord compression, and intractable pain, commonly referred to as skeletal-related events (SREs).Citation2,Citation4 The third-generation bisphosphonate, zoledronic acid (ZOL, Zometa®; Novartis Pharma AG, Basel, Switzerland), an inhibitor of bone resorption, is the current standard of care for preventing SREs associated with bone metastases and is the only agent that has demonstrated statistically significant reductions of SREs due to metastatic bone lesions in various cancers.Citation5–Citation8
Figure 1 Bone as an ideal site for metastatic cancer cells. After injection into the left ventricle, luciferase-labeled cancer cells initially appeared as diffuse photon accumulations throughout the body, were completely undetectable after 6 hours, and subsequently developed bone metastases (A). Schematic representation of the interplay between metastatic cancer cells, osteoblasts and osteoclasts in bone, and of the function of the RANK/RANKL/OPG axis. various growth factors are released when osteoclasts absorb bone that provides fertile ground for cancer cells to grow. Cancer cells activate osteoblasts to increase the production of RANKL. RANKL then interacts with RANK and promotes differentiation into mature osteoclasts. OPG acts as an inhibitor of osteoclastogenesis by serving as a decoy receptor for RANKL (B). RANK: receptor activator of nuclear factor κB.
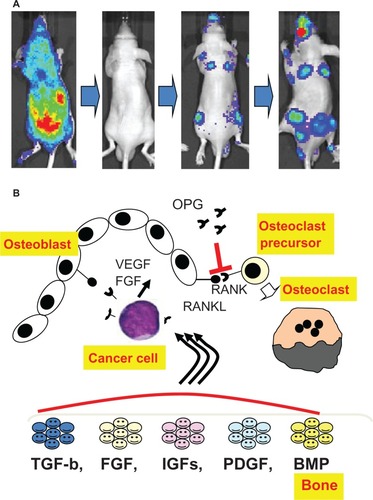
The receptor activator of nuclear factor-κB (RANK, also called tumor necrosis factor receptor superfamily member 11A; TNFRSF11A), the RANK ligand (RANKL, also called the tumor necrosis factor ligand superfamily member 11; TNFSF11), and osteoprotegerin (OPG, also called TNFRSF11B) are the major regulators of bone metabolism.Citation9,Citation10 The RANK/RANKL/OPG axis regulates osteoclastogenesis and may play a key role in bone metastasis. The function of the RANK/RANKL/OPG axis and the interplay between metastatic cells, osteoblasts, and osteoclasts in bone are summarized in .
Denosumab (XGEVA; Amgen, Thousand Oaks, CA), a novel agent targeting bone resorption, is a fully human monoclonal antibody that binds to and neutralizes RANKL, thereby inhibiting osteoclast function and preventing generalized bone resorption and local bone destruction.Citation11 In Phase III clinical trials, denosumab was demonstrated to be noninferior (trending to superior) to zoledronic acid in preventing or delaying first on-study SREs in patients with bone dissemination or myeloma.Citation11,Citation12 Therefore, denosumab is emerging as a novel anti-resorptive clinical agent for use in bone metastasis. This article provides a brief overview of the characteristics of bone metastasis in urological cancers, including renal cell, urothelial, and prostate cancer, summarizes mechanisms of dissemination to bone, and presents the mechanism of action and efficacy of denosumab in the clinical management of urological cancer bone metastasis.
Characteristics of urological cancer bone metastasis
Renal cell cancer
Bone is a common metastatic site in RCC, second only to lung, with estimates of frequency ranging from 24% to 51%.Citation13–Citation15 RCC bone metastasis often has a pseudo-negative appearance on a bone scan, is mostly osteolytic and generally aggressive, and results in rapid bone destruction.Citation16 Upon diagnosis of RCC bone metastasis, since the current standard technique for diagnosing bone metastasis is radionuclide 99 m-technetium pyrophosphate scintigraphy, which identifies sites of active bone formation, RCC bone lesions often have a pseudo-negative appearance ().Citation15,Citation16 In a study of patients with RCC bone metastasis, Zekri et al reported that the frequency of lesions with osteolytic, osteoblastic, and mixed radiographic appearance was approximately 71%, 18%, and 11%, respectively.Citation17 Aggressive osteolysis also often causes significant morbidity from the resulting SREs, and radiotherapy for bone pain, hypercalcemia, and pathological fractures create serious problems for patients and often lead to poor performance status.Citation15–Citation17 Zekri et al also reported the SREs experienced by 84 patients with bone metastases with a skeletal morbidity rate (number of SREs/ patient/year) between 2.5 and 4.0 during the first year.Citation17 In their report, 29% developed hypercalcemia,Citation17 attributable to tumor production of cytokines and ectopic polypeptides including parathyroid hormone-related peptide. presents a summary of the incidence of SREs and efficacy of zoledronic acid in patients with prostate, breast, or renal cell cancers based on Phase III clinical trials.Citation5,Citation7,Citation8 Although the study period was different for each trial, the morbidity of RCC bone metastasis was comparable to that of prostate and breast cancer bone metastasis, yet the morbidity of RCC bone metastasis receives considerably less attention than that of breast and prostate cancer bone metastasis. Despite a higher incidence of bone lesions, a longer survival is observed after diagnosis of dissemination to bone.Citation5,Citation7,Citation8
Figure 2 Characteristics of urological cancer skeletal lesions. Characteristics of bone metastasis from renal cell cancer. The bulky bone metastatic lesion, which was demonstrated by abdominal CT-scan, has a negative appearance by bone scan. Typical bone metastatic lesions from urothelial cancer, which have a positive appearance by bone scan, are shown on the right side (A). Schematic representation of the interplay between prostate cancer, bone and testosterone (B).
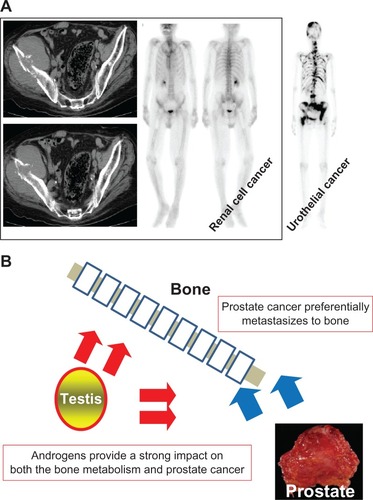
Table 1 Comparison of skeletal-related events in various cancers in zoledronic acid Phase III clinical studies
The distribution of RCC skeletal metastasis was predominantly to the axial skeleton, affecting the pelvis in 48%, the spine in 34%, and the ribs in 48% of cases.Citation17 These results are consistent with our recent report in which involvement of the pelvis, spine, and ribs was observed in 27%, 48%, and 48% of cases, respectively.Citation15 In our study, lower extremities were also frequently involved (37%).Citation15 To avoid pathologic fracture and/or intense pain, we often recommend surgical treatment and/or radiation therapy for metastatic lesions, including those of the pelvis, spine, and extremities.Citation15
Although it would appear to predispose toward poor prognosis, the prognosis of RCC bone metastasis is controversial.Citation18–Citation21 Neither of two large retrospective studies identified bone metastasis as an independent prognostic factor.Citation18,Citation21 Recently, we reported treatment outcomes in RCC patients with bone metastasis at our institution.Citation15 Among 214 RCC patients with metastasis, 71 patients (33%) were found to have bone metastases at the time of the initial diagnosis of metastasis.Citation15 The estimated median overall survival from the time of diagnosis of bone metastasis was 27.7 months and the probabilities of patients surviving 1 year, 2 years, and 5 years were 63.7%, 52.2%, and 19.3%, respectively.Citation15 These observations are comparable to other metastatic sites in RCC.
Urothelial cancer
Bladder cancer is the most common urothelial cancer, followed by renal, pelvic, and ureteral cancer, and is the fourth most common solid malignancy in males in the United States.Citation22 It is estimated that in 2012, there will be 73,510 new cases and 14,880 deaths from bladder cancer in the United States.Citation22 Although 70% of bladder cancers are superficial at presentation and can be managed by transurethral resection, 60% to 70% of superficial tumors recur and 20% to 30% of recurrent disease progresses to a higher stage or grade.Citation23,Citation24 Radical cystectomy is the standard and most effective treatment for operable invasive bladder cancer;Citation24,Citation25 however, at initial diagnosis, one fifth of bladder cancer patients exhibit visceral metastasis and up to half of the remaining patients eventually develop invasive cancer and distant metastases.Citation24,Citation26 Chemotherapy with a combination of methotrexate, vinblastine, doxorubicin, and cisplatin or gemcitabine and cisplatin is the common therapeutic option for distant metastases.Citation23,Citation25,Citation26 Bone is the most common visceral metastatic site for bladder cancer, followed by lung and liver.Citation27 Although bladder cancer is chemosensitive, most deaths from bladder cancer are caused by invasion and subsequent metastases that are resistant to conventional chemotherapy.Citation26,Citation28 We and others pointed out that visceral metastases, including bone metastases, were predictors of poor prognosis.Citation29,Citation30 Novel therapeutic options are needed to improve outcome in advanced bladder cancer.
Prostate cancer
Prostate cancer has a very high proclivity for metastasizing to bone. Even at the initial diagnosis of prostate cancer, 24% of patients have metastases as determined by a bone scan.Citation31,Citation32 According to the Prostate Cancer Clinical Trials Working Group 2, approximately 90% of patients with castration-resistant prostate cancer develop bone metastasis.Citation33 The presence or absence of bone metastases is one of the most important factors influencing the selection of therapy in prostate cancer.
In 2004, two landmark trials, TAX 327 and SWOG 99-16, showed for the first time that docetaxel, a microtubule-targeted tubulin-polymerizing agent, improved survival in metastatic castration-resistant prostate cancer.Citation34,Citation35 Zoledronic acid is a highly potent nitrogen-containing bisphosphonate shown to reduce skeletal complications in patients with bone metastases arising from various solid cancers, including prostate cancer.Citation36 Accumulated evidence has revealed that zoledronic acid and taxoids act synergistically or additively in inhibiting the growth of various malignancies, including leukemia, lung cancer, bladder cancer, breast cancer, and prostate cancer.Citation36–Citation40 Thus, the combination of docetaxel, prednisolone, and zoledronic acid is the current mainstay of treatment for castration-resistant prostate cancer and bone metastasis.
In addition to the high prevalence of bone metastasis, treatment-induced bone loss is typically seen in patients undergoing androgen-deprivation therapy (ADT).Citation41–Citation43 ADT has been the standard treatment for metastatic prostate cancer since Huggins and Hodges first reported it in 1941.Citation44 Currently, ADT is also frequently employed in the nonmetastatic setting, either for aging men with local disease or for biochemical failure after prostatectomy or radiation therapy.Citation45,Citation46
ADT is associated with anemia, weight gain, insulin resistance, ischemic heart disease, hypogonadism, and increasing bone resorption.Citation31,Citation47 Of these ADT complications, increasing bone resorption is of particular concern because it may lead to osteoporosis and bone fractures.Citation41,Citation48 A number of studies have shown that ADT-treated patients suffer from bone loss and skeletal-related adverse events,Citation49–Citation52 and a recent clinical report disclosed a negative correlation between skeletal fractures and overall survival in ADT-treated patients.Citation53 These observations have led to the suggestion that clinicians should be alert to the impact of ADT on bone mineral density and should strive to prevent bone loss. The survival of patients with prostate cancer and bone metastasis is commonly longer than that of patients with other malignant tumors. Therefore, management of bone metastasis and bone metabolism plays important roles in prostate cancer therapy. A schematic representation of the interplay between prostate cancer, bone, and testosterone is shown in .
Mechanism of bone metastasis
More than 100 years ago, Stephen Paget described the “seed and soil” hypothesis in which seeds of metastatic cancer cells preferentially settle in the soil of the bone matrix.Citation44 Bone is an abundant repository for immobilized growth factors, including transforming growth factor β, fibroblast growth factor, insulin-like growth factors I and II, platelet-derived growth factor, and bone morphogenetic proteins ().Citation1,Citation16,Citation36 When osteoclasts absorb bone by secreting protons and proteases, growth factors are released that provide fertile ground for cancer cells to grow. As described earlier, bone provides an ideal microenvironment in which metastatic cancer cells can thrive ().
Bone-metastasizing cancer cells do not directly activate osteoclasts. They activate stromal cells/osteoblasts through parathyroid hormone receptors to increase the production of RANKL, which plays a central role in osteoclast differentiation and activation.Citation1–Citation3 RANKL then interacts with RANK expressed in hematopoietic osteoclast precursors and promotes differentiation into mature osteoclasts.Citation9–Citation11 The interaction between RANK and its ligand RANKL plays an important role in osteoclastogenesis. RANKL is a cytokine produced by osteoblasts that stimulates osteoclast activity and inhibits osteoclast apoptosis by binding to its receptor RANK, which is expressed on osteoclasts and their precursors.Citation1,Citation9–Citation11 In contrast, OPG, which is expressed by many tissues and cells including osteoblasts, acts as an inhibitor of osteoclastogenesis by serving as a decoy receptor for RANKL.Citation1,Citation9 Consequently, the RANK/RANKL/OPG axis regulates osteoclastogenesis and may perform a key role in bone metastasis. The function of the RANK/RANKL/OPG axis and the interplay between metastatic cells, osteoblasts, and osteoclasts in bone are summarized in .
The RANK/RANKL/OPG axis
We and others demonstrated the potential therapeutic modulation of the RANK/RANKL/OPG axis.Citation54–Citation56 In RCC, Mikami et al demonstrated a positive correlation between RANKL expression level, primary tumor stage, and presence of distant metastasis, and elevated RANKL and RANK and low OPG expression was a significant and independent predictor of recurrence, bone metastasis and poor prognosis.Citation54 In addition, recombinant RANKL protein could stimulate the migration of the clear cell RCC cell line Caki-1 in vitro, and this enhanced migration could be inhibited by recombinant OPG protein.Citation54 They concluded that the RANK/RANKL/OPG axis was not only involved in RCC bone metastasis but was also involved in metastasis to other organs through the stimulation of cancer cell migration.Citation54
In prostate cancer, the expression of RANKL, RANK, and OPG was found to be low in normal cells and markedly elevated in prostate cancer cell lines.Citation55 The frequency of expression of RANKL, RANK, and OPG was significantly higher in metastatic prostate cancer than in organ-confined cancer. In addition, the observed increased expression of RANKL, RANK, and OPG correlated with Gleason score, TNM stage, androgen status and serum prostate-specific antigen levels in patients.Citation55 The authors concluded that the expression of RANKL, RANK, and OPG correlated with more aggressive, advanced, metastatic prostate carcinoma, suggesting their potential utility in the diagnosis, prognosis, and therapy of prostate cancer.Citation55
We evaluated the significance of OPG gene polymorphisms in prostate cancer progression.Citation56 The presence of the variant C allele of the OPG 950 T/C polymorphism in the promoter region of OPG may have a considerable protective effect against bone metastasis or disease progression.Citation56 In addition, the analysis of metastatic prostate cancer patients (stage D) revealed that the T allele of the OPG 950 T/C polymorphism was an independent risk factor, predicting short survival compared to the C allele, according to Cox proportional hazard regression analysis (P = 0.031).Citation56 The C allele of the 950 T/C polymorphism was associated with high bone marrow density, suggesting that OPG can function effectively to prevent the RANK/RANKL osteolytic signal.Citation56 Therefore, the RANK/RANKL/OPG axis may regulate the development of prostate cancer metastasis by modulating bone metabolism.
Zoledronic acid, a novel bisphosphonate, in urological cancer bone metastasis
Zoledronic acid (Zometa®; Novartis Pharma AG), a third-generation bisphosphonate, has the strongest inhibitory activity against bone resorption and is the only bisphosphonate with demonstrated statistically significant reduction of SREs due to metastatic bone lesions in various cancers.Citation16,Citation36,Citation57 Zoledronic acid had been the only treatment option for preventing SREs in patients with bone metastasis.Citation16,Citation36,Citation57 Bisphosphonates exhibit a high affinity for calcified matrices, such as hydroxyapatite, in bone,Citation16,Citation34,Citation55 and they decrease the recruitment, proliferation, and differentiation of pre-osteoclasts, their adhesion to the mineralized matrix, and the resorptive activity of mature osteoclasts.Citation16,Citation36,Citation57 Bisphosphonates, both nonamino-bisphosphonates and amino-bisphosphonates, also promote the induction of apoptosis in osteoclasts.Citation16,Citation36,Citation57 In a randomized, placebo-controlled trial of zoledronic acid in hormone-refractory metastatic prostate cancer, a greater proportion of patients who received placebo had SREs compared to those who received zoledronic acid at 4 mg (44.2% vs 33.2%; P = 0.021).Citation5 The median time to first SRE was 321 days in patients who received placebo but SRE was not reached in patients who received zoledronic acid at 4 mg (P = 0.011).Citation5 The pain and analgesic scores were higher in patients who received placebo than in patients who received zoledronic acid.Citation5 Although there were no differences in disease progression, performance status, or quality-of-life scores between the groups, zoledronic acid has been adopted as a standard option in hormone-refractory prostate cancer with bone metastasis.Citation5
RCC will likely be one of the most sensitive cancers to bone resorption inhibition therapy. In a retrospective subset analysis of 74 patients with RCC enrolled in a multicenter, randomized, placebo-controlled study, zoledronic acid was found to significantly reduce the proportion of patients with an SRE (37% vs 74% for placebo; P = 0.015).Citation7 Similarly, zoledronic acid significantly reduced the mean skeletal morbidity rate (2.68 vs 3.38 for placebo; P = 0.014) and extended the time to the first event (median not reached vs 72 days for placebo; P = 0.006).Citation7 The median time to progression of bone lesions was significantly longer for patients treated with zoledronic acid (P = 0.014 vs placebo).Citation7 Although there was no statistical significance compared to placebo, the median overall survival showed a trend toward favoring zoledronic acid (295 days for the 4 mg zoledronic acid group vs 216 days for the placebo group; P = 0.179).Citation7 These results suggest that zoledronic acid not only decreases SREs, but also improves survival in patients with bone metastatic RCC.
In the context of urothelial cancer, a prospective, randomized, placebo-controlled trial in patients with bladder cancer metastatic to bone was recently reported.Citation58 Compared to patients receiving placebo, those receiving zoledronic acid had a lower mean incidence of SREs (2.1 vs 0.95, respectively), and zoledronic acid prolonged the median time to first SRE compared to placebo (16 vs 8 weeks, respectively).Citation58 Multiple event analysis of SREs revealed that zoledronic acid decreased the risk of SRE development by 59% (hazard ratio [HR], 0.413). Zoledronic acid also increased the 1-year survival rate compared to placebo (36.3% vs 0%, respectively).Citation58 The investigators concluded that zoledronic acid therapy decreased the incidence of SREs and improved the 1-year survival rate of patients with bone metastases from bladder cancer, potentially through its anticancer activity.Citation58
In addition to clinical trials using zoledronic acid, we previously used a mouse model to demonstrate the possibility to target osteoclasts to treat RCC and urothelial cancers.Citation59–Citation61 The first study showed that minodronic acid (also known as YM529), another third-generation bisphosphonate, had anticancer activity and synergistically augmented interferon-induced growth inhibition in vitro and in vivo.Citation59 The second and third studies established luciferase-labeled human RCC and urothelial cancer cell models to investigate the inhibition of osteoclasts and of bone metastasis by minodronic acid in vivo.Citation60 Minodronic acid administered systemically successfully showed significant anticancer efficacy in luciferase-labeled urothelial cancer cell bone metastases monitored using an in vivo imaging system.Citation60 In addition, we demonstrated that prevention of osteoclast activity and/or maturation could lead inhibition of the growth of luciferase-labeled human RCC cells in a bone metastatic mouse model.Citation61 Therefore, prevention of osteoclast genesis and function is an attractive therapeutic strategy in RCC and urothelial cancer bone metastasis.
In vitro and in vivo preclinical anticancer activity of denosumab
Denosumab inhibits the maturation of osteoclasts by binding to and inhibiting RANKL. As with zoledronic acid, the anti-SRE effect of denosumab is considered indirect via the inhibition of osteoclast function; however, some in vitro and in vivo studies have demonstrated a possible direct anticancer effect.
As discussed above, RANKL is a critical osteoclast differentiation factor that is highly expressed in the bone marrow environment. Besides indirect activity via prevention of osteoclast function, denosumab was demonstrated to act directly on RANK-expressing cancer cells, including breast, prostate and melanoma cells.Citation62 Jones et al demonstrated that RANKL plays an important role in the cell migration and tissue-specific metastatic behavior of cancer cells. They found expression of the receptor RANK on various cancer cells that preferentially metastasize to bone.Citation62 In addition, RANKL triggers cytoskeletal changes and migration in several RANK-expressing cancer cells. Moreover, the authors demonstrated that the inhibition of the RANKL/ RANK signal by OPG in vivo markedly and selectively reduces bone metastasis.Citation62
Gonzalez-Suarez et al demonstrated that RANK and RANKL are expressed in normal, premalignant, and neoplastic mammary epithelium. In addition, in complementary gain-of-function studies in mouse mammary tumor virus (MMTV)-RANK transgenic mice, accelerated preneoplasia and increased mammary tumor formation was observed after multiparity or treatment with carcinogen and hormone (progesterone).Citation63 In loss-of-function approaches, selective pharmacological inhibition of RANKL attenuated mammary tumor development, not only in hormone- and carcinogen-treated MMTV-RANK and wild-type mice, but also in the MMTV-neu transgenic spontaneous tumor model.Citation63 The authors concluded that the RANK/RANKL pathway directly contributes to mammary carcinogenesis.Citation63 These preclinical studies suggest a possible direct anticancer effect of denosumab.
In addition, Miller et al showed the potential clinical utility of denosumab with docetaxel in castration-resistant prostate cancer.Citation64 They demonstrated that the RANKL inhibitor OPG-Fc alone reduced bone resorption (P < 0.001 vs PBS), inhibited progression of established osteolytic lesions, and reduced tumor area (P < 0.0001 vs PBS).Citation64 In addition, combination of the RANKL inhibitor OPG-Fc and docetaxel markedly suppressed skeletal tumor burden (P = 0.0005) and increased median survival time by 16.7% (P = 0.0385) compared to docetaxel alone in a murine model of prostate cancer bone metastasis.Citation64
Denosumab, a new option in the treatment of urological cancer bone metastasis
Three main Phase III clinical studies have been published in prostate cancer. The first study was conducted to evaluate the effect of denosumab on BMD and fractures in men receiving ADT.Citation65 The second study compared denosumab to zoledronic acid for the prevention of SREs in men with bone metastases from castration-resistant prostate cancer.Citation66 The third study assessed denosumab for prevention of bone metastasis or death in nonmetastatic castration-resistant prostate cancer.Citation67 The purpose and results of these studies are summarized in .
Table 2 Summary of denosumab Phase III clinical trials in prostate cancer
In the first study, which was double-blind and multi-center, patients receiving ADT for nonmetastatic prostate cancer were randomly assigned to receive denosumab at a dose of 60 mg subcutaneously every 6 months or placebo (734 patients in each group).Citation65 Denosumab therapy was associated with significant increases in BMD at the lumbar spine, total hip, femoral neck, and distal third of the radius at all time points.Citation66 Moreover, patients who received denosumab had a decreased incidence of new vertebral fractures at 36 months (1.5% vs 3.9% with placebo) (relative risk, 0.38; P = 0.006).Citation65
In the second study, men with castration-resistant prostate cancer and no previous exposure to intravenous bisphosphonate were enrolled at 342 centers in 39 countries; 1904 patients were randomly assigned to 120 mg subcutaneous denosumab (n = 950) or 4 mg intravenous zoledronic acid (n = 951).Citation66 The median time to first on-study SRE was 20.7 months with denosumab compared to 17.1 months with zoledronic acid (HR, 0.82, P = 0.0002 for noninferiority; P = 0.008 for superiority).Citation66 Although more events of hypocalcaemia occurred in the denosumab group (13%) than in the zoledronic acid group (6%; P < 0.0001), denosumab seemed to not be worse than zoledronic acid for preventing SREs and potentially represents a novel treatment option in men with bone metastases from castration-resistant prostate cancer.Citation66
In the third study, which was double-blind, randomized, and placebo-controlled, men with nonmetastatic castration-resistant prostate cancer at high risk of bone metastasis were enrolled at 319 centers in 30 countries; 1432 patients were randomly assigned to treatment groups (716 denosumab, 716 placebo).Citation67 Denosumab significantly increased bone metastasis-free survival by a median of 4.2 months compared to placebo (median 29.5 vs 25.2 months; HR, 0.85; P = 0.028).Citation67 Denosumab also significantly delayed the time to first bone metastasis (33.2 vs 29.5 months; HR, 0.84; P = 0.032); however, the overall survival did not differ between the groups (denosumab, 43.9 vs placebo, 44.8 months; HR, 1.01; P = 0.91).Citation67 Although the rates of adverse events and serious adverse events were similar in both groups, 33 (5%) patients on denosumab developed osteonecrosis of the jaw (none on placebo) and 12 (2%) patients on denosumab developed hypocalcemia (< 1% on placebo).Citation67
There is currently no clinical report describing the efficacy of denosumab in RCC or urothelial cancer; however, the anti-bone resorption agent zoledronic acid demonstrated good clinical and preclinical efficacy in these diseases.Citation5,Citation8,Citation58–Citation64 Decreased SREs were associated with a potential survival benefit in patients with metastatic RCC and bladder cancer in bone metastatic RCC and bladder cancer. Zoledronic acid has the potential to induce renal impairment, and therefore requires that renal function be monitored and sometimes doses adjusted or withheld, particularly in patients with RCC or upper urinary tract urothelial cancer who often have a single functional kidney. In contrast, denosumab has no renal toxicity and is emerging as a key therapeutic option for the treatment of bone metastases from urological cancers.
Conclusions and future directions
Accumulated evidence suggests that the inhibition of bone resorption is a promising anticancer therapy without severe adverse effects. Until now, zoledronic acid was the only approved agent inhibiting bone resorption. Denosumab is a novel and attractive option for the treatment of bone metastases from urological cancers. In prostate cancer, the addition of the novel hormonal agents abiraterone acetate, MDV-3100, and TAK700 to the therapeutic armamentarium will lead to greater reliance on ADT, suggesting that the adverse events associated with ADT may become a greater clinical problem in the future. As a result, a more careful assessment and monitoring of SRE and more anti-bone resorption therapeutic options will be needed. Currently, the optimum therapy for metastatic bone disease as well as anti-bone resorption remains uncertain. In order to clarify this issue, accumulated clinical practice will be necessary.
Acknowledgements
The work was partly supported by the Smoking Research Foundation, the Takeda Science Foundation, and Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Disclosure
The authors report no conflict of interest in this work.
References
- RoodmanGDMechanisms of bone metastasisN Engl J Med2004350161655166415084698
- OnishiTHayashiNTheriaultRLHortobagyiGNUenoNTFuture directions of bone-targeted therapy for metastatic breast cancerNat Rev Clin Oncol201071164165120808302
- MorganSCParkerCCLocal treatment of metastatic cancer – killing the seed or disturbing the soil?Nat Rev Clin Oncol20118850450621647193
- ColemanREBisphosphonates: clinical experienceOncologist20049Suppl 4142715459426
- SaadFGleasonDMMurrayRTZoledronic Acid Prostate Cancer Study GroupA randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinomaJ Natl Cancer Inst200294191458146812359855
- RosenLSGordonDTchekmedyianSZoledronic acid versus placebo in the treatment of skeletal metastases in patients with lung cancer and other solid tumors: a phase III, double-blind, randomized trial – the Zoledronic Acid Lung Cancer and Other Solid Tumors Study GroupJ Clin Oncol200321163150315712915606
- LiptonAColombo-BerraABukowskiRMRosenLZhengMUrbanowitzGSkeletal complications in patients with bone metastases from renal cell carcinoma and therapeutic benefits of zoledronic acidClin Cancer Res20041018 Pt 26397S6403S15448038
- KohnoNAogiKMinamiHZoledronic acid significantly reduces skeletal complications compared with placebo in Japanese women with bone metastases from breast cancer: a randomized, placebo-controlled trialJ Clin Oncol200523153314332115738536
- WittrantYThéoleyreSChipoyCRANKL/RANK/OPG: new therapeutic targets in bone tumours and associated osteolysisBiochim Biophys Acta200417042495715363860
- HofbauerLCSchoppetMClinical implications of the osteoprotegerin/ RANKL/RANK system for bone and vascular diseasesJAMA2004292449049515280347
- BodyJJFaconTColemanREA study of the biological receptor activator of nuclear factor-kappaB ligand inhibitor, denosumab, in patients with multiple myeloma or bone metastases from breast cancerClin Cancer Res20061241221122816489077
- HenryDHCostaLGoldwasserFRandomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myelomaJ Clin Oncol20112991125113221343556
- SrinivasanRLinehanWMTreatment of advanced renal cell carcinomaKavoussiLRNovickACPartinAWPetersCAWeinAJCampbell-Walsh Urology10th edNew York, NYSaunders201114751491
- LjungbergBHanburyDCKuczykMAEuropean Association of Urology Guideline Group for renal cell carcinomaRenal cell carcinoma guidelineEur Urol20075161502151017408850
- YuasaTUrakamiSYamamotoSTreatment outcome and prognostic factors of the patients with renal cell cancer bone metastasisClin Exp Metastasis201128440541121365325
- LiptonAManagement of Bone Metastasis in patients with Renal Cell Carcinoma and Other Malignancies of the Genitourinary TractKantoffPSaadFSmithMRManagement of Skeletal Complications of Prostate Cancer and Other Genitourinary MalignanciesPhiladelphia, PAFA Davis Co2004207234
- ZekriJAhmedNColemanREHancockBWThe skeletal metastatic complications of renal cell carcinomaInt J Oncol200119237938211445855
- NaitoSYamamotoNTakayamaTPrognosis of Japanese metastatic renal cell carcinoma patients in the cytokine era: a cooperative group report of 1463 patientsEur Urol20105731732519136199
- KuczykMAAnastasiadisAGZimmermannRMerseburgerASCorvinSStenziACurrent aspects of the surgical management of organ-confined, metastatic, and recurrent renal cell cancerBJU Int2005965721727 quiz i–ii.16144527
- ToyodaYShinoharaNHarabayashiTSurvival and prognostic classification of patients with metastatic renal cell carcinoma of boneEur Urol200752116316817098353
- MotzerRJBacikJMurphyBARussoPMazumdarMInterferon-alfa as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinomaJ Clin Oncol200220128929611773181
- SiegelRNaishadhamDJemalACancer statistics, 2012CA Cancer J Clin2012621102922237781
- LernerSPSternbergCNManagement of metastatic and invasive bladder cancerKavoussiLRNovickACPartinAWPetersCAWeinAJCampbell-Walsh Urology10th edNew York, NYSaunders201123552374
- GeeJSabichiALGrossmanHBChemoprevention of superficial bladder cancerCrit Rev Oncol Hematol200243327728612270783
- StenzlACowanNCDe SantisMEuropean Association of Urology (EAU)Treatment of muscle-invasive and metastatic bladder cancer: update of the EAU guidelinesEur Urol20115961009101821454009
- DreicerRLocally advanced and metastatic bladder cancerCurr Treat Options Oncol20012543143612057106
- BabaianRJJohnsonDELlamasLAyalaAGMetastases from transitional cell carcinoma of urinary bladderUrology19801621421447404907
- HussainSAJamesNDThe systemic treatment of advanced and metastatic bladder cancerLancet Oncol20034848949712901963
- BellmuntJAlbanellJPaz-AresLSpanish Oncology Genitourinary GroupPretreatment prognostic factors for survival in patients with advanced urothelial tumors treated in a phase I/II trial with paclitaxel, cisplatin, and gemcitabineCancer200295475175712209718
- TsukamotoTYoneseJOhkuboYFukuiIPhase I/II study of a combined gemcitabine, etoposide, and cisplatin chemotherapy regimen for metastatic urothelial carcinomaCancer2006106112363236816649219
- NelsonJBHormonal therapy of prostate cancerKavoussiLRNovickACPartinAWPetersCAWeinAJCampbell-Walsh Urology10th edNew York, NYSaunders201129342953
- JohanssonJEAndrénOAnderssonSONatural history of early, localized prostate cancerJAMA2004291222713271915187052
- ScherHIHalabiSTannockIProstate Cancer Clinical Trials Working GroupDesign and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working GroupJ Clin Oncol20082671148115918309951
- PetrylakDPTangenCMHussainMHDocetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancerN Engl J Med2004351151513152015470214
- TannockIFde WitRBerryWRTAX 327 InvestigatorsDocetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancerN Engl J Med2004351151502151215470213
- YuasaTKimuraSAshiharaEHabuchiTMaekawaTZoledronic acid – a multiplicity of anti-cancer actionCurr Med Chem200714202126213517691952
- KimuraSKurodaJSegawaHAntiproliferative efficacy of the third-generation bisphosphonate, zoledronic acid, combined with other anti-cancer drugs in leukemic cell linesInt J Hematol2004791374314979476
- MatsumotoSKimuraSSegawaSEfficacy of the third-generation bisphosphonate, zoledronic acid alone and combined with anti-cancer agents against small cell lung cancer cell linesLung Cancer200547313915603852
- Neville-WebbeHLEvansCAColemanREHolenIMechanisms of the synergistic interaction between the bisphosphonate zoledronic acid and the chemotherapy agent paclitaxel in breast cancer cells in vitroTumour Biol20062729210316582586
- JagdevSPColemanREShipmanCMRostami-HACroucherPIThe bisphosphonate, zoledronic acid, induces apoptosis of breast cancer cells: evidence for synergy with paclitaxelBr J Cancer20018481126113411308265
- SmithMROsteoporosis and obesity in men receiving hormone therapy for prostate cancerJ Urol20041725 Pt 2S52S5615535444
- WangWYuasaTTsuchiyaNBone mineral density in Japanese prostate cancer patients under androgen-deprivation therapyEndocr Relat Cancer200815494395218667685
- YuasaTMaitaSTsuchiyaNRelationship between bone mineral density and androgen-deprivation therapy in Japanese prostate cancer patientsUrology20107551131113720163839
- HugginsCHodgesVCStudies on prostate cancer: I. The effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostateCancer Res19411293297
- CooperbergMRGrossfeldGDLubeckDPCarrollPRNational practice patterns and time trends in androgen ablation for localized prostate cancerJ Natl Cancer Inst2003951398198912837834
- SharifiNGulleyJLDahutWLAndrogen deprivation therapy for prostate cancerJAMA2005294223824416014598
- HiganoCSSide effects of androgen deprivation therapy: monitoring and minimizing toxicityUrology2003612 Suppl 1323812667885
- ShahinianVBKuoYFFreemanJLGoodwinJSRisk of fracture after androgen deprivation for prostate cancerN Engl J Med2005352215416415647578
- GreenspanSLCoatesPSereikaSMNelsonJBTrumpDLResnickNMBone loss after initiation of androgen deprivation therapy in patients with prostate cancerJ Clin Endocrinol Metab200590126410641716189261
- BruderJMMaJZBaslerJWWelchMDPrevalence of osteopenia and osteoporosis by central and peripheral bone mineral density in men with prostate cancer during androgen-deprivation therapyUrology200667115215516413352
- MoroteJMorinJPOrsolaAPrevalence of osteoporosis during long-term androgen deprivation therapy in patients with prostate cancerUrology200769350050417382153
- MoroteJOrsolaAAbascalJMBone mineral density changes in patients with prostate cancer during the first 2 years of androgen suppressionJ Urol200717551679168316600728
- OefeleinMGRicchiutiVSConradPWClinical predictors of androgen-independent prostate cancer and survival in the prostate-specific antigen eraUrology200260112012412100936
- MikamiSKatsubeKOyaMIncreased RANKL expression is related to tumour migration and metastasis of renal cell carcinomasJ Pathol2009218453053919455604
- ChenGSircarKAprikianAPottiAGoltzmanDRabbaniSAExpression of RANKL/RANK/OPG in primary and metastatic human prostate cancer as markers of disease stage and functional regulationCancer2006107228929816752412
- NaritaNYuasaTTsuchiyaNA genetic polymorphism of the osteoprotegerin gene is associated with an increased risk of advanced prostate cancerBMC Cancer2008822418684318
- FleischHDevelopment of bisphosphonatesBreast Cancer Res200241303411879557
- ZaghloulMSBoutrusREl-HossienyHKaderYAEl-AttarINazmyMA prospective, randomized, placebo-controlled trial of zoledronic acid in bony metastatic bladder cancerInt J Clin Oncol201015438238920354750
- YuasaTNogawaMKimuraSA third-generation bisphosphonate, minodronic acid (YM529), augments the interferon αβ-mediated inhibition of renal cell cancer cell growth both in vitro and in vivoClin Cancer Res2005112 Pt 185385915701876
- SatoKYuasaTNogawaMA third-generation bisphosphonate, minodronic acid (YM529), successfully prevented the growth of bladder cancer in vitro and in vivoBr J Cancer200695101354136117043684
- MaitaSYuasaTTsuchiyaNAntitumor effect of sunitinib against skeletal metastatic renal cell carcinoma through inhibition of osteoclast functionInt J Cancer2012130367768421387300
- JonesDHNakashimaTSanchezOHRegulation of cancer cell migration and bone metastasis by RANKLNature2006440708469269616572175
- Gonzalez-SuarezEJacobAPJonesJRANK ligand mediates progestin-induced mammary epithelial proliferation and carcinogenesisNature2010468732010310720881963
- MillerRERoudierMJonesJArmstrongACanonJDougallWCRANK ligand inhibition plus docetaxel improves survival and reduces tumor burden in a murine model of prostate cancer bone metastasisMol Cancer Ther2008772160216918606716
- SmithMREgerdieBHernández TorizNDenosumab HALT Prostate Cancer Study GroupDenosumab in men receiving androgen-deprivation therapy for prostate cancerN Engl J Med2009361874575519671656
- FizaziKCarducciMSmithMDenosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind studyLancet2011377976881382221353695
- SmithMRSaadFColemanRDenosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trialLancet20123799810394622093187