Abstract
Different plasma and urinary parameters have been tested as valuable prognostic markers for children with neuroblastoma (NB), but conclusive results from multivariate analyses are still lacking. Samples collected at diagnosis from 505 patients diagnosed in Italy between June 1994 and November 2010 were analyzed at the Italian reference laboratory according to standard methodologies. Patient clinical data were retrieved from the Italian NB Registry. For statistical analysis, patients were grouped according to stage, age, MYCN status, and outcome. Cumulative survival was calculated by the Kaplan–Meier procedure using the first quartile of the marker distribution as a cut-off value to stratify the patients. Multivariate analysis was performed by the Cox regression model by considering only the significant variables. When the entire cohort of patients was considered, none of the different parameters had an independent prognostic value. However, in patients with localized disease without MYCN amplification the significant positive associations between urinary and plasmatic vanillylmandelic acid (VMA)/homovanillic acid (HVA) ratio and a better prognosis remained significant (P < 0.05 and P < 0.01, respectively), as well as, the positive association between high lactate dehydrogenase (LDH) values and a worse prognosis (P < 0.001). Moreover, in stage 4 patients without MYCN amplification, neuron-specific enolase levels above 200 ng/mL and LDH levels above 2500 IU/mL maintained their significant association with a worse outcome (P = 0.01 and P = 0.0001, respectively). In conclusion, LDH had an independent prognostic value in patients of all stages without MYCN amplification. Moreover, the urinary and plasmatic VMA/HVA ratio was an independent predictor of prognosis in patients with localized disease without MYCN amplification. Since LDH and catecholamine metabolites are measured in all patients at diagnosis, these findings may be helpful for an easy, cost-effective, patient risk stratification.
Keywords:
Introduction
Ferritin, neuron-specific enolase (NSE), lactate dehydrogenase (LDH), and the catecholamine metabolites, vanillylmandelic acid (VMA) and homovanillic acid (HVA), are commonly assessed in children suspected to have neuroblastoma (NB), and the levels of these markers are commonly used for differential diagnosis.Citation1 Several studies performed over more than 3 decadesCitation2–Citation7 have suggested that they may have a prognostic value, but the small numbers of patients studied in each cohort have hampered the possibility to assess their role independent from stage, age, and MYCN status, which are the established parameters to stratify patients.Citation1 Only Berthold et alCitation6 demonstrated an independent prognostic role of plasma VMA/HVA ratio in patients with localized NB, but this finding was of limited interest since catecholamine metabolites are commonly measured in urine rather than in plasma. Methodological issues further limited the power of previous reports. Analyses were often performed at the home institutions rather than at a national reference laboratory, and unavoidable methodological changes occurred over the years.
Recently, it has been shown that the presence of either structural or numerical aberrations in the genome of primary NB tumor cells can predict outcome of low- and intermediate-risk NB patients.Citation8,Citation9 Thus, multicenter studies are currently stratifying patients in different protocol arms depending on these features, (see http://www.siopen-net.org). These analyses, however, require a primary tumor biopsy and are costly and time-consuming.
Thus, we decided to retrieve all the results obtained at the Italian reference laboratory where all the analyses for the various markers have been centralized since 1994, and check whether any of these markers was an independent predictor of survival.
Patients and methods
The study cohort includes all patients diagnosed in Italy with NB, according to the International Neuroblastoma Staging System (INSS) criteria,Citation10 between June 1994 and November 2010, for whom at least one diagnostic analysis was performed at the Italian reference laboratory located at the Gaslini Institute. None of the patients included were diagnosed by mass screening. Moreover, no modifications of the INSS criteria have occurred during the study period. The demographic, clinical and follow-up data (at January 2011) of the 505 study patients (109 stage 1, 39 stage 2, 92 stage 3, 217 stage 4, and 48 stage 4S) were retrieved from the Italian NB Registry.Citation11
Laboratory analysis
Urinary HVA and VMA concentrations were determined on samples derived from 24-hour urine collections. Urinary and plasma HVA and VMA were performed by gas chromatography coupled to mass spectrometry (GC-MS) as described by Hunneman.Citation12 Since 2006 urinary HVA and VMA were analyzed by high-pressure liquid chromatography coupled with electrochemical detection (HPLC-EC), using a commercially available method (HVA-VMA by HPLC; Bio Rad Laboratories, Milan, Italy). Urinary HVA and VMA concentrations were expressed as a ratio to creatinine concentration, previously determined using the Jaffè method. LDH, NSE, and ferritin were determined on heparinized plasma, using routine clinical chemistry laboratory methods. Sensitivity and specificity of urinary HVA and VMA are reported in Monsaingeon et alCitation13; sensitivity of plasma HVA, VMA, NSE, and LDH in Simon et alCitation14; specificity of NSE in Viallard et alCitation15; whereas ferritin and LDH are nonspecific markers.
Treatment
After diagnosis the study patients were treated according to the Italian Neuroblastoma protocols,Citation11,Citation16–Citation18 until the commencement of the various International Society of Pediatric Oncology European Neuroblastoma Group (SIOPEN) protocols.Citation19–Citation22 All protocols were approved by the local Institutional Review Boards. Before being enrolled, and treated on their respective trials, patients or their guardians signed a consent form allowing the use of their clinical and genetic data for clinical research. No other specific informed consent was required for the purposes of this study.
Statistical analysis
For each marker, statistical analysis was first performed on the entire cohort of the study patients. Then patients were grouped according to the following variables: stage (localized, metastatic NB), age (≤18 months, .18 months), and MYCN status (not amplified, amplified). Differences were assessed by Mann–Whitney U test or Fisher’s exact test. Correlations were estimated by the Pearson’s coefficient. Cumulative survival was calculated by the Kaplan–Meier procedure using the first quartile of the marker distribution as cut-off value to stratify the patients. For event-free survival plots, the occurrence of relapse, progression, or death were considered as an event. Statistical significance was estimated by log rank test. Multivariate analysis was performed by the Cox regression method by including only the significant variables.
Results
In the study period, a total of 1717 children were diagnosed with NB in Italy. Of these, 505 patients had at least one urinary or plasma marker analyzed at diagnosis at the Italian reference laboratory. As shown in , where the demographic, biological and clinical features of the study patients are summarized, no significant differences were found between the study patients and the entire population of NB patients diagnosed in Italy during the study period. Moreover, the event-free and overall survival (EFS and OS) of the study patients, stratified by stage, age, MYCN status, and treatment protocol was similar to that of the entire population.Citation11
Table 1 Demographic, biological and clinical features of the study patients stratified by stage, and comparison with the whole NB population diagnosed during the study period
The results obtained for each marker in the entire study cohort are summarized in . Of the 411 patients that had urinary HVA and VMA determined, 174 had also plasma catecholamine determined. Correlation between urinary and plasma values was high (HVA: Pearson’s correlation coefficient = 0.19, P < 0.05; VMA: Pearson’s correlation coefficient = 0.25, P < 0.01), confirming previous findings.Citation6,Citation23 As reported previously,Citation2,Citation7,Citation24,Citation25 the median levels of VMA and HVA increased by stage and the higher levels were found in stage 4S infants (251 and 215 μg/mg creatinine, respectively, with a median ratio of 1.41).
Table 2 Concentration of each analyte in the entire cohort of study patients (N = 505) and in patients with localized disease (N = 288)
Values for ferritin, NSE, and LDH were available for half of the study patients, but overlapping with urinary HVA and VMA was relatively low (N = 162).
Prognostic values of urinary and plasmatic VMA/HVA ratio
VMA and HVA are the end product of two different pathways of catecholamine catabolism, thus their relative abundance seems to associate with different phenotypes, each characterized by different prognosis.Citation2,Citation26–Citation28 Indeed, plasma VMA/HVA ratio was shown to be predictive in localized patients.Citation6 In our cohort, univariate analysis demonstrated that neither VMA nor HVA had any prognostic value, even when patients with localized and metastatic disease were considered separately. However, in patients with localized NB, both urinary and plasma VMA/HVA ratio positively associated with a better outcome (). Patients with urinary VMA/HVA ratio < 0.50 had 3.44 times greater chance of relapse than patients with a ratio ≥ 0.50 (95% confidence interval [CI]: 1.26–9.39; P < 0.05). Most importantly, multivariate analysis demonstrated that in patients with localized disease without MYCN amplification, urinary VMA/HVA ratio < 0.5 and plasma VMA/HVA ratio < 0.15 were independent predictors of poor prognosis (, respectively; P = 0.017 for both).
Figure 1 Kaplan–Meier plots of event-free survival of (A) patients with localized NB stratified by urinary VMA/HVA cut-off value; (B) patients with localized disease stratified by plasma VMA/HVA cut-off value; (C) the entire cohort of study patients stratified by ferritin cut-off value; (D) patients with stage 4 disease stratified by NSE cut-off value; (E) patients with localized disease stratified by LDH cut-off value; and (F) patients with stage 4 disease stratified by LDH cut-off value.
Abbreviations: HVA, homovanillic acid; LDH, lactate dehydrogenase; NB, neuroblastoma; NSE, neuron-specific enolase; VMA, vanillylmandelic acid.
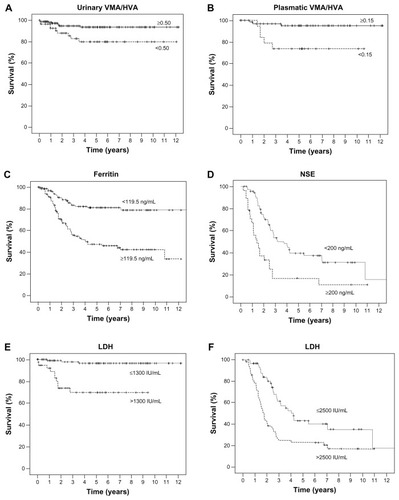
Table 3 Prognostic value of each marker in the different groups of neuroblastoma patients
Prognostic value of ferritin
Ferritin was evaluated in 272 patients (). In the whole cohort of patients, univariate analysis indicated a significant positive association between ferritin values higher than the first quartile value and a worse EFS (; P < 0.01). However, multivariate analysis demonstrated that ferritin levels positively associated with stage, thus eliminating its predictive power ().
Prognostic value of NSE
Neuron-specific enolase was evaluated in 233 patients (). When the entire cohort of patients was considered, NSE did not associate with EFS or OS. However, in stage 4 patients NSE levels < 200 ng/mL associated with a better EFS (). Multivariate analysis confirmed that the NSE levels were an independent predictor of prognosis in stage 4 patients without MYCN amplification ( and ; P < 0.01).
Prognostic value of LDH
Lactate dehydrogenase was evaluated in a total of 279 patients. Both in patients with localized and metastatic disease, high LDH values positively associated with a worse prognosis (P < 0.01). In particular, patients with localized disease with LDH values > 1300 IU/mL had 12.9 times greater chance of relapse (95% CI: 3.34–49.78; P < 0.001). However, multivariate analysis confirmed LDH predictive power only in patients without MYCN amplification ( and ; P = 0.0001). In stage 4 patients, the LDH cut-off value discriminating patients with good and bad prognosis was 2500 IU/mL (). Also, in stage 4 patients LDH was an independent prognostic factor only in patients without MYCN amplification (; P = 0.0001).
Discussion
The aim of this work was to investigate the independent prognostic value of different markers commonly evaluated at diagnosis in NB patients as a potential tool to stratify patients in different risk groups. The availability of a routine test, performed at diagnosis in peripheral blood or urine samples, may reduce the time and cost of prognostic analyses with respect to those performed on primary tumors.Citation8,Citation9
In our study, LDH values above 1300 IU/mL in patients with localized disease and above 2500 IU/mL in stage 4 patients were positively associated with a worse outcome, independent of age and stage. LDH levels, however, were positively associated with MYCN amplification. Thus, in prospective trials for patients with localized disease without MYCN amplification, LDH levels at diagnosis should be evaluated for their predictive power as compared to the genetic tests performed on the primary tumors. An association between LDH levels and outcome of patients with localized disease was also observed in the Localised Neuroblastoma European Study, but no multivariate analysis was performed.Citation19 Similarly, the Task Force of the International Neuroblastoma Risk GroupCitation29 found that a single LDH cut-off level of 587 IU/mL could dichotomize NB patients into good and poor prognosis. However, LDH was not included in the new INRG Staging System because of its unspecific nature.
Our study demonstrated that in patients with localized disease without MYCN amplification, urinary and plasmatic VMA/HVA ratio were also positively associated with a better event-free survival. In 1992, Berthold et alCitation6 demonstrated that plasma VMA/HVA ratio was an independent predictor of EFS for patients with localized disease. Although Gahr and HunnemanCitation23 had shown a good agreement between urinary and plasma catecholamine levels, urinary levels were globally measured. Thus, the report did not receive proper attention.
As first reported by Laug et alCitation2 and confirmed by several groups,Citation7,Citation24,Citation25 a higher VMA/HVA ratio was found in stage 4S infants. VMA and HVA are the byproducts of two distinct catecholamine metabolic pathways starting from norepinephrine and dopa, respectively. Gitlow et alCitation30 first suggested that high HVA levels were produced by undifferentiated, unfavorable prognosis tumors. KontrasCitation31 showed that high VMA levels correlated to a more differentiated phenotype with better prognosis. In our study, information on the differentiation of the primary tumors was not available, thus precluding any study of association. However, our multivariate analysis confirmed the association between low VMA levels and MYCN amplification,Citation25–Citation28 and added weight to the association between low VMA levels and poor prognosis previously found in smaller cohorts of NB patients.Citation2,Citation4,Citation24
Our multivariate analysis, performed separately in patients with metastatic and localized disease, also explained the contrasting results found in these two subsets of patients by Aydin et alCitation7 with regard to the association of VMA levels with outcome. In fact, the frequency of MYCN amplification in stage 4 patients is higher than in localized patients, whose VMA levels increase from stage 1 to stage 3. In view of this effect, the use of VMA/HVA ratio had greater advantage with respect to the use of VMA alone.
As for the other two markers evaluated in our study, ferritin association with outcome was dependent on the stage of disease, whereas NSE levels > 200 ng/mL positively associated with a worse outcome only in stage 4 patients without MYCN amplification, thus limiting their utility in patient risk stratification.
It is important to note that in our study about 30% of the NB patients had unknown MYCN status, thus the association of each marker with MYCN status must be taken with caution. Further validation of our findings in a future prospective study is needed.
Conclusion
Urinary and plasma VMA/HVA ratio > 0.5 and 0.15, respectively, and LDH values < 1300 IU/mL were found to be independent predictors of good prognosis in patients with localized NB without MYCN amplification. Thus, these data, commonly determined at diagnosis in all NB patients, should be collected in future protocols for this subset of patients, and their prognostic value compared to that of structural and numerical chromosomal aberrations present in the primary tumors.
Acknowledgments
This study was supported in part by Fondazione Italiana per la Lotta al Neuroblastoma. The authors thank Angelo Maffia and Daniela Bugnone, Genoa, for keeping the plasma and urinary repositories, and all the nurses and physicians that centralized the samples. SB is recipient of a Fondazione Italiana Neuroblastoma fellowship.
Disclosure
The authors report no conflicts of interest in this work.
References
- MarisJMRecent advances in neuroblastomaN Engl J Med2010362232202221120558371
- LaugWESiegelSEShawKNLandingBBaptistaJGutensteinMInitial urinary catecholamine metabolite concentrations and prognosis in neuroblastomaPediatrics19786217783683787
- ZeltzerPMMarangosPJParmaAMRaised neuron-specific enolase in serum of children with metastatic neuroblastoma. A report from the Children’s Cancer Study GroupLancet1983283463613636135871
- IzbickiTBozekJPerekDWozniakWUrinary dopamine/noradrenaline and dopamine/vanillylmandelic acid ratios as a reflection of different biology of adrenergic clones in children’s neuroblastic tumorsJ Pediatr Surg19912610123012341779334
- ShusterJJMcWilliamsNBCastleberryRSerum lactate dehydrogenase in childhood neuroblastoma. A Pediatric Oncology Group recursive partitioning studyAm J Clin Oncol19921542953031514525
- BertholdFHunnemanDHHarmsDKaserHZieschangJSerum vanillylmandelic acid/homovanillic acid contributes to prognosis estimation in patients with localised but not with metastatic neuroblastomaEur J Cancer199228A12195019541419287
- AydinGBKutlukMTYalcinBVaranAAkyuzCBuyukpamukcuMThe prognostic significance of vanillylmandelic acid in neuroblastomaPediatr Hematol Oncol201027643544820578806
- SchleiermacherGMichonJRibeiroASegmental chromosomal alterations lead to a higher risk of relapse in infants with MYCN-non-amplified localised unresectable/disseminated neuroblastoma (a SIOPEN collaborative study)Br J Cancer2011105121940194822146831
- CocoSTheissenJScaruffiPAge-dependent accumulation of genomic aberrations and deregulation of cell cycle and telomerase genes in metastatic neuroblastomaInt J Cancer201213171591160022234802
- BrodeurGMPritchardJBertholdFRevisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatmentJ Clin Oncol1993118146614778336186
- HauptRGaraventaAGambiniCImproved survival of children with neuroblastoma between 1979 and 2005: a report of the Italian Neuroblastoma RegistryJ Clin Oncol201028142331233820351331
- HunnemanDHMass fragmentographic determination of homovanillic and 4-hydroxy-3-methoxy mandelic acids in 50 microliter plasmaClin Chim Acta198313521691746652925
- MonsaingeonMPerelYSimonnetGCorcuffJBComparative values of catecholamines and metabolites for the diagnosis of neuroblastomaEur J Pediatr2003162639740212684897
- SimonTHeroBHunnemanDHBertholdFTumour markers are poor predictors for relapse or progression in neuroblastomaEur J Cancer200339131899190312932669
- ViallardJLTigetFHartmannOSerum neuron-specific/nonneuronal enolase ratio in the diagnosis of neuroblastomasCancer19886212254625533191453
- De BernardiBConteMManciniALocalized resectable neuroblastoma: results of the second study of the Italian Cooperative Group for NeuroblastomaJ Clin Oncol19951348848937707115
- GaraventaABoniLLo PiccoloMSLocalized unresectable neuroblastoma: results of treatment based on clinical prognostic factorsAnn Oncol200213695696412123342
- De BernardiBCarliMCasaleFStandard-dose and high-dose peptichemio and cisplatin in children with disseminated poor-risk neuroblastoma: two studies by the Italian Cooperative Group for NeuroblastomaJ Clin Oncol19921012187018781453202
- De BernardiBMosseriVRubieHTreatment of localised resectable neuroblastoma. Results of the LNESG1 study by the SIOP Europe Neuroblastoma GroupBr J Cancer20089971027103318766186
- CaneteAGerrardMRubieHPoor survival for infants with MYCN-amplified metastatic neuroblastoma despite intensified treatment: the International Society of Paediatric Oncology European Neuroblastoma ExperienceJ Clin Oncol20092771014101919171715
- De BernardiBGerrardMBoniLExcellent outcome with reduced treatment for infants with disseminated neuroblastoma without MYCN gene amplificationJ Clin Oncol20092771034104019171711
- LadensteinRValteau-CouanetDBrockPRandomized Trial of prophylactic granulocyte colony-stimulating factor during rapid COJEC induction in pediatric patients with high-risk neuroblastoma: the European HR-NBL1/SIOPEN studyJ Clin Oncol201028213516352420567002
- GahrMHunnemanDHThe value of determination of homovanillic and vanillylmandelic acids in plasma for the diagnosis and follow-up of neuroblastoma in childrenEur J Pediatr198714654894933678274
- StrengerVKerblRDornbuschHJDiagnostic and prognostic impact of urinary catecholamines in neuroblastoma patientsPediatr Blood Cancer200748550450916732582
- Di CataldoADauDConteMDiagnostic and prognostic markers in infants with disseminated neuroblastoma: a retrospective analysis from the Italian Cooperative Group for NeuroblastomaMed Science Monit2009151MT1118
- ParodiSPapioFHauptRConteMDe BernardiBThe prognostic role of urinary catecholamines in infants with disseminated neuroblastoma may be mediated by MYCN amplificationPediatr Blood Cancer2007485593 author reply 593–59416937359
- NakagawaraAIkedaKHigashiKSasazukiTInverse correlation between N-myc amplification and catecholamine metabolism in children with advanced neuroblastomaSurgery1990107143492404349
- ZambranoEReyes-MugicaMHormonal activity may predict aggressive behavior in neuroblastomaPediatr Dev Pathol20025219019911910515
- CohnSLPearsonADLondonWBThe International Neuroblastoma Risk Group (INRG) classification system: an INRG Task Force reportJ Clin Oncol200927228929719047291
- GitlowSEBertaniLMRausenAGribetzDDziedzicSWDiagnosis of neuroblastoma by qualitative and quantitative determination of catecholamine metabolites in urineCancer1970256137713835422912
- KontrasSBUrinary excretion of 3-methoxy-4-hydroxymandelic acid in children with neuroblastomaCancer19621597898614458280