Abstract
Computed tomography (CT) and magnetic resonance imaging (MRI) are common imaging methods to detect cervical lymph node metastasis of head and neck cancer. We aimed to assess the diagnostic efficacy of CT and MRI in detecting cervical lymph node metastasis, and to establish unified diagnostic criteria via systematic review and meta-analysis. A systematic literature search in five databases until January 2014 was carried out. All retrieved studies were reviewed and eligible studies were qualitatively summarized. Besides pooling the sensitivity (SEN) and specificity (SPE) data of CT and MRI, summary receiver operating characteristic curves were generated. A total of 63 studies including 3,029 participants were involved. The pooled results of meta-analysis showed that CT had a higher SEN (0.77 [95% confidence interval {CI} 0.73–0.87]) than MRI (0.72 [95% CI 0.70–0.74]) when node was considered as unit of analysis (P<0.05); MRI had a higher SPE (0.81 [95% CI 0.80–0.82]) than CT (0.72 [95% CI 0.69–0.74]) when neck level was considered as unit of analysis (P<0.05) and MRI had a higher area under concentration-time curve than CT when the patient was considered as unit of analysis (P<0.05). With regards to diagnostic criteria, for MRI, the results showed that the minimal axial diameter of 10 mm could be considered as the best size criterion, compared to 12 mm for CT. Overall, MRI conferred significantly higher SPE while CT demonstrated higher SEN. The diagnostic criteria for MRI and CT on size of metastatic lymph nodes were suggested as 10 and 12 mm, respectively.
Introduction
The occurrence of cervical lymph node metastasis in patients with head and neck cancers are very common.Citation1 The presence of cervical lymph node metastasis may affect the optimal treatment choice as well as prognosis in patients.Citation2 Management of patients presenting with cervical lymph node metastasis includes selective or radical neck dissection, followed by radiotherapy and/or chemotherapy depending on the pathological findings of the nodes.Citation3–Citation5 Besides, the detection of cervical lymph node metastasis is very important for predicting prognosis in patients with head and neck cancers.Citation6–Citation8
Many imaging techniques exist for identifying cervical lymph node metastasis in patients with head and neck cancers.Citation9–Citation12 Among them, computed tomography (CT) and magnetic resonance imaging (MRI) are the most widely used tools.Citation13 Both of them have improved accuracy of nodal staging over clinical palpation and the nodes which are clinically occulted can be visualized through these techniques.Citation14 Usually the cervical lymph nodes demonstrate similar density as muscle on pre-contrast images of CT examination, and they can be separated from adjacent vessels by their differential enhancement after contrast administration.Citation15 On the other hand, MRI is considered to have similar accuracy for identifying the cervical lymph node metastasis of head and neck cancer.Citation16,Citation17 Because of the intrinsic high soft-tissue discrimination, MRI has become the preferred method for evaluating the soft tissues of the head and neck recently.Citation18 Under current health care settings, the routine practice for evaluating patients with head and neck cancer is to perform either CT or MRI, but not both.Citation19 Thus, to determine whether one of the two techniques is superior to the other is critical for providing guidance for clinical practice. Besides, since relevant studies utilized very different diagnostic criteria, it is warranted to determine the unified criteria that are most appropriate. A systematic review to assess all available evidence is thus needed for providing a comprehensive evaluation for these aims.
The aim of this study was thus to compare CT and MRI for detecting cervical lymph node metastasis in patients with head and neck cancer and to establish the unified diagnostic criteria by performing a systematic review and meta-analysis.
Methods
Inclusion criteria
The inclusion criteria were as follows: a) types of study: diagnostic accuracy test studies designed as cohort studies; b) participants: patients with biopsy proven head and neck cancers who would undergo neck dissection; c) index tests: CT and/or MRI; d) target condition: cervical lymph node metastasis; e) reference standard: histopathology examination; f) outcome: rates of true positive, false positive, false negative, and true negative or related data that could be used to calculate them.
Literature search
With no language restriction, the following databases were searched for retrieving studies: MEDLINE (1948 to 25 January 2014), EMBASE (1980 to 25 January 2014), China National Knowledge Infrastructure (1994 to 25 January 2014), VIP Chinese Journal Database (1989 to 25 January 2014), and Chinainfo (1998 to 25 January 2014).
The search strategy was optimized for all consulted databases, taking into account the differences in the various controlled vocabularies as well as the differences of database-specific technical variations.Citation20 Once relevant articles were identified, their reference lists were searched for additional articles. Both Medical Subject Headings (MeSH) and free text words were used in the search strategy with the following MeSH terms: “head and neck neoplasm”, “neoplasm metastases”, “SEN and SPE”, “Tomography, Spiral Computed” and “Magnetic Resonance Imaging”.
Study selection
Two reviewers independently examined the titles and abstracts of each search record to remove obviously irrelevant ones, and then retrieved the full text articles for potentially eligible articles. The full-texts were further examined according to the inclusion criteria. Discrepancies were resolved by consensus.
Data extraction
A standardized data extraction form was used by two authors independently for data extraction from included studies. Discrepancies were resolved by discussion, with input from a third author. The contents of the form included: name of first author, publication year, country, participants’ age, sex, number of included patients, tumor location, unit, details of CT and/or MRI, study design (prospective or retrospective).
Quality assessment
The methodological quality of included studies was assessed by The Quality Assessment Diagnostic Accuracy Studies statement-2 (QUADAS-2),Citation21 which included four domains: patient selection, index test, reference standard, and flow and timing. Each domain was assessed in terms of risk of bias and the first three were assessed in terms of concerns regarding applicability. Signaling questions were included to assist judgments on risk of bias. The signaling questions in the QUADAS-2 were presented as shown in . The result for each item was categorized as yes (Y), unclear (U), or no (N). The summary risk of bias for each study was categorized as low (A), unclear (B), or high (C).
Table 1 Signaling questions in the QUADAS-2
Meta-analysis
Measures of diagnostic efficacy of CT and/or MRI included sensitivity (SEN), specificity (SPE), positive likelihood ratio (+LR), negative likelihood ratio (−LR), accuracy (ACC), and diagnostic odds ratios (DOR) with 95% confidence intervals (CIs). Summary receiver operating characteristic (SROC) curves were then drawn. The area under the curve (AUC) and Q* (the point where SEN is equal to SPE on the SROC curve) were calculated.
To detect any differences for SEN, SPE, AUC, and Q* between CT and MRI, a Z-test was conducted (Z= (VAL1–VAL2)/SQRT (SE1Citation2+SE2Citation2). The test standard was set at α=0.05. VAL indicates the mean of SEN, SPE, AUC or Q* of the CT or MRI and SE indicates the standard error of the corresponding variable.
Heterogeneity analysis
Heterogeneity between studies was evaluated by I2 statistic.Citation22,Citation23 If I2≤50% and P≥0.10, the heterogeneity was considered not significant and in such case the fixed-effects model would be used in meta-analysis. Otherwise, the random-effects model would be used.Citation24,Citation25
Meta-regression
Meta-regression was used to determine any potential source of heterogeneity that might influence the overall assessment. The test standard for meta-regression was set at α=0.10. Relevant variables which might cause heterogeneities were tested, and any suggested sources of heterogeneity were considered as proof for a subgroup analysis. Variables detected by meta-regression included publication year (0= published before 2000; 1= published in or after 2000), race (0= Mongolia; 1= Caucasian), study type (0= retrospective; 1= prospective), risk of bias (0= high; 1= unclear; 2= low), blinding of the radiologists (0= no or unclear; 1= yes) and blinding of the pathologists (0= no or unclear; 1= yes). Meta-disc 1.4 and STATA 11.0 (StataCorp LP, College Station, TX, USA) were used to perform the statistical analyses.Citation26,Citation27
Results
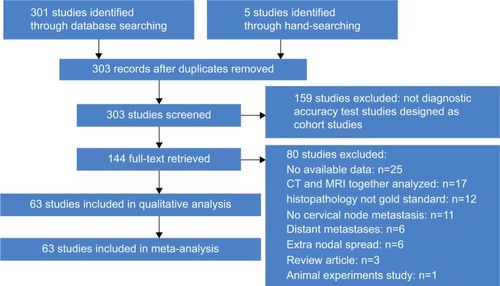
Selection of literature
The computerized and manual search retrieved a total of 306 articles. After assessing the titles and abstracts, 144 articles were found to be potentially relevant. After the full text assessment, 63 studies met the inclusion criteria and were included in this meta-analysis ().Citation28–Citation90
Study characteristics
Of the 63 included studies, 24 were retrospective and 39 were prospective. A total of 3,029 participants were involved in these studies. Among those patients, 1,044 underwent both CT and MRI examination, 2,395 underwent MRI examination, and 1,678 underwent CT examination. Three kinds of unit of analysis were used, including node, neck level (the neck was classified as five levels according to anatomical landmarks), and patients. When node was considered as the unit of analysis, available studies involved 22 with CT and 30 with MRI. When neck level was considered as the unit of analysis, eight studies with CT and 16 with MRI were available. When patient was considered as the unit of analysis, available studies included eight with CT and eleven with MRI. The tumor locations included floor of mouth, nasopharynx, retromolar trigonum, mandibule, maxilla, supra-glottic larynx, oropharynx, laryngopharynx, hypopharynx, parotid gland, submandibular gland, tonsil, thyroid gland, cervical esophageal, paranasal sinuses et al. The characteristics of included studies are listed in .
Table 2 Study characteristics and included data sets for CT and MRI of the included articles
Quality of included studies
All included studies had fairly good applicability. For the risk of bias assessment, only two studies had a low risk of bias, five had a high risk, and 56 had an unclear risk ().
Table 3 Risk of bias of included studies
Comparison of CT and MRI in detecting cervical lymph node metastasis with node as unit of analysis
For CT, meta-regression analysis showed that the diagnostic efficacy was not affected by any of the tested variables. These variables thus did not account for heterogeneity between studies. After pooling 22 studies, we detected that CT had a mean (CI) SEN of 0.77 (95% CI 0.73–0.80), SPE of 0.85 (0.84–0.87), +LR of 3.84 (2.51–5.87), −LR of 0.34 (0.24–0.27), ACC of 0.8357, and DOR of 13.57 (6.99–26.33). The SROC was demonstrated in and the AUC was 0.8429 and Q* was 0.7745. For MRI, meta-regression analysis also showed that the diagnostic efficacy was not affected by any of the tested variables. After pooling 30 studies, we identified that MRI had a mean (CI) SEN of 0.72 (0.70–0.74), SPE of 0.84 (0.83–0.85), +LR of 5.06 (3.72–6.88), −LR of 0.27 (0.21–0.34), ACC of 0.8126, and DOR of 25.21 (15.97–39.80). The SROC is shown in and the AUC was 0.9054 and Q* was 0.8371.
Figure 2 Summary receiver operator characteristic curves of CT and MRI (node as unit of analysis).
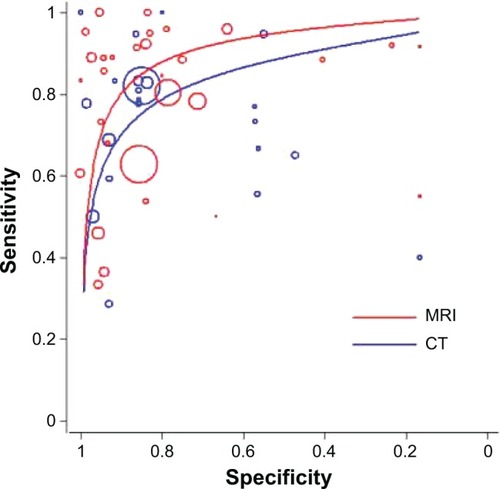
By comparing the diagnostic efficacy between CT and MRI when node was treated as the unit of analysis, the results indicated that CT had a higher SEN, although the SPE and summarized diagnostic efficacy were comparable. The details are listed in .
Table 4 Comparison of meta-analysis results on diagnostic efficacy between CT and MRI
Comparison of CT and MRI in detecting cervical lymph node metastasis with neck level as unit of analysis
For MRI, meta-regression analysis detected that none of the tested variables accounted for heterogeneity between studies. After pooling 16 studies, it was detected that MRI had a mean (CI) SEN of 0.80 (0.77–0.82), SPE of 0.81 (0.80–0.82), +LR of 5.34 (3.24–8.82), −LR of 0.27 (0.20–0.37), ACC of 0.5257, DOR of 24.61 (12.21–49.61) and the AUC was 0.8860 and Q* was 0.8165 (). For CT, similarly none of the tested variables accounted for heterogeneity. The pooling of available studies identified that CT had a mean (CI) SEN of 0.80 (0.75–0.84), SPE of 0.72 (0.69–0.74), +LR of 5.60 (2.13–14.73), −LR of 0.26 (0.19–0.36), ACC of 0.6888, DOR of 23.76 (7.87–71.79) and the AUC was 0.8787 and Q* was 0.8091 ().
Figure 3 Summary receiver operator characteristic curves of CT and MRI (neck level as unit of analysis).
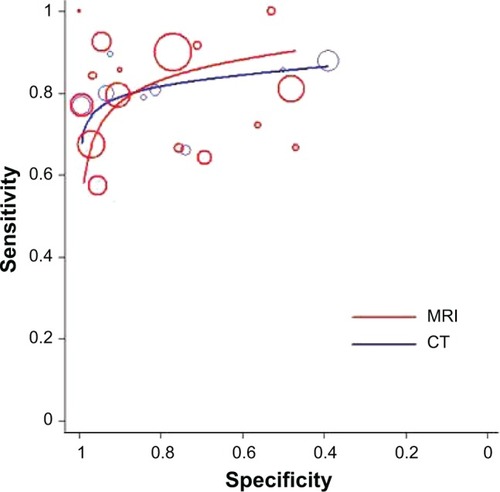
The comparison between CT and MRI showed that MRI had significantly higher SPE than CT while the other variables were comparable between these two techniques ().
Comparison of CT and MRI in detecting cervical lymph node metastasis with patient as unit of analysis
For the two studies, the pooled results showed that CT had a mean (CI): SEN, 0.81 (0.65–0.92); SPE, 0.35 (0.24–0.42); +LR, 1.14 (0.87–1.50); −LR, 0.70 (0.32–1.52); DOR, 1.66 (0.57–4.82) (Figure S1). For MRI, which included ten studies, meta-regression analysis showed that study type significantly affected the assessment of diagnostic efficacy (P=0.04) (). Based on the subgroup analysis according to study types, for the four retrospective studies, the pooled results indicated that MRI had a mean (CI) SEN, 0.77 (0.69–0.85); SPE, 0.48 (0.42–0.55); +CR, 2.42 (0.99–5.91); −CR, 0.54 (0.27–1.06); DOR, 5.24 (0.96–28.55) (Figure S2). For the five prospective studies, the pooled results showed that MRI had a mean (CI) SEN, 0.80 (0.72–0.86); SPE, 0.35 (0.67–0.86); +LR, 2.79 (1.44–5.40); −LR, 0.25 (0.08–0.76); DOR, 14.63 (3.64–58.70) (Figure S3). Pooling of the overall nine studies indicated the mean (CI) values for the following parameters to be: SEN, 0.79 (0.73–0.84); SPE, 0.56 (0.51–0.62); +LR, 2.64 (1.30–5.34); −LR, 0.37(0.20–0.71); DOR, 8.87 (2.42–32.55); AUC (0.8158); Q* (0.7498) (Figure S4).
Table 5 Results of meta-regression (MRI patient)
The comparison between CT and MRI showed that MRI had significantly higher AUC than CT while the other variables demonstrated no statistical significance between them. The details are listed in .
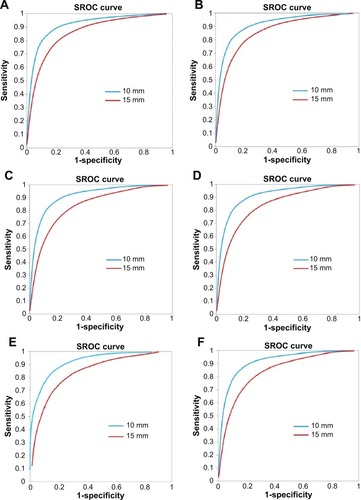
Lymph node size criteria
The size of metastatic lymph nodes used as diagnostic criteria of MRI and CT varied considerably among studies and among different neck levels (Table S1). To determine the best diagnostic criteria, a meta-analysis was conducted for different neck levels with lymph node unit data. For each neck level, the SROC curve was drawn to show the diagnostic efficacy of MRI for different node sizes (). The results revealed that the minimal axial diameter of 10 mm in lymph node-bearing regions could be considered as the best size criterion for assessing cervical lymph node metastasis in patients with head and neck cancer (Table S2). For CT, the suggested criterion was 12 mm (Table S3). Considering the limited number of studies for CT, SROC curves were not drawn.
Discussion
Head and neck cancer is a common malignant neoplasm worldwide.Citation1 One of the most important factors that influences treatment approaches and therapeutic outcomes for patients with head and neck cancer is the presence of metastatic cervical lymph node. The accurate detection of the cervical lymph node metastasis is thus very important.Citation91,Citation92 Clinical palpation used to be the method to detect cervical nodal metastasis before the development of imaging technologies. However, studies have shown that both the SEN and the SPE of this technique were unsatisfactory, with a high false positive rate of 25%–51%. The improvements in imaging technologies may make it possible for cervical lymph nodes metastasis in head and neck cancer patients can be effectively diagnosed, especially with CT and MRI.Citation11,Citation12,Citation93–Citation96 However, under current health care settings usually only one imaging technique will be performed. Thus a systematic evaluation regarding whether one of the two imaging techniques (CT and MRI) can have a better efficacy than the other will be critical to better guide the clinical practice.
In our systematic review and meta-analysis, we comprehensively evaluated all available evidence from 63 studies for evaluating this question whether one of the two imaging techniques (CT and MRI) can have a better efficacy. Besides pooling results from available studies, we assessed potential sources of heterogeneities via meta-regression and conducted sub-group analyses for significant heterogeneity sources detected. Our meta-analyses suggested that CT had a higher SEN than MRI when node was used as unit of analysis; MRI had a higher SPE when neck level was used as unit of analysis; and MRI had a higher AUC when patient was used as unit of analysis. Our findings showed that CT and MRI are effective tools for detecting the cervical lymph node metastasis in patients with head and neck cancer. Since the diagnostic criteria presented in relevant studies varied significantly, we also summarized available evidence to reveal the most appropriate ones for these two techniques, respectively. Usually, the diagnosis of metastatic cervical lymph nodes consisted of two parts, namely, structural and size changes. The structural changes included central necrosis or cystic degeneration, spherical (rather than flat or bean) shape, or abnormal grouping of nodes (a cluster of three or more lymph nodes of borderline size). In different studies, the description of the structural changes differed only mildly. However, the criteria for sizes differed considerably. Most authors recommended using the minimal axial diameter to assess metastasis. The criterion for minimal axial diameter varied between 5 to 15 mm. Our meta-analysis showed that the minimal axial diameter of 10 mm in lymph node-bearing regions could be considered as the best criterion for assessing cervical lymph node metastasis in patients with head and neck cancer for MRI, compared to 12 mm for CT. Several limitations should be acknowledged for the interpretation of our findings. Firstly, although we conducted meta-regression analyses and showed that the assessed variables largely did not account for heterogeneities between studies, additional undetected variables may account for heterogeneities which warrants further research. Secondly, in some of our analyses, only a very limited number of studies were available. For example, when focusing on the 12 mm size criterion, there was only one study available for evaluating CT with node unit, and future studies for evaluating relevant topics are warranted. In conclusion, through this comprehensive systematic review and meta-analysis, we identified that CT and MRI had acceptable diagnostic efficacy in detecting cervical lymph node metastasis in patients with head and neck cancer. When node was used as unit of analysis, CT had a higher SEN. When neck level was used as unit of analysis, MRI had a higher SPE. Out findings suggest that MRI is superior to CT in the diagnosis of cervical lymph node metastasis, especially in diagnosis confirmation. While CT had a better efficacy in diagnosis exclusion. The diagnostic criteria for MRI and CT for size of metastatic lymph nodes were established. Further high-quality studies are warranted to confirm our findings.
Supplementary materials
Figure S1 Meta-analysis of CT for detecting cervical lymph node metastasis in head and neck cancer patients (patient as unit of analysis).
Abbreviations: CT, computed tomography; CI, confidence interval; LR, likelihood ratio; df, degrees of freedom; SROC, summary receiver operating characteristic; AUC, area under the curve; SE, standard error.
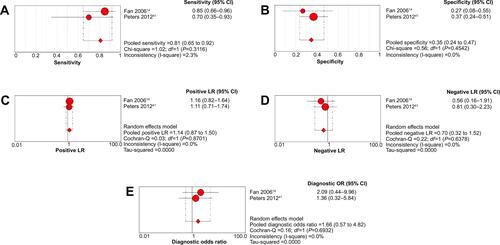
Figure S2 Meta-analysis of MRI for detecting cervical lymph node metastasis in head and neck cancer patients (patient as unit of analysis) (retrospective studies).
Abbreviations: MRI, magnetic resonance imaging; CI, confidence interval; df, degrees of freedom; LR, likelihood ratio; OR, odds ratio.
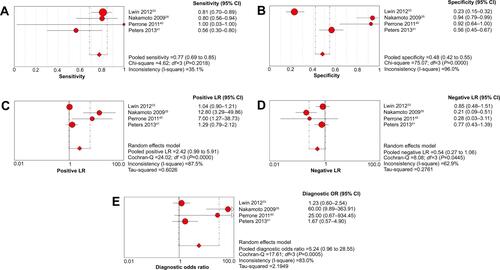
Figure S3 Meta-analysis of MRI for detecting cervical lymph node metastasis in head and neck cancer patients (patient as unit of analysis) (prospective studies).
Abbreviations: MRI, magnetic resonance imaging; CI, confidence interval; df, degrees of freedom; LR, likelihood ratio; OR, odds ratio.
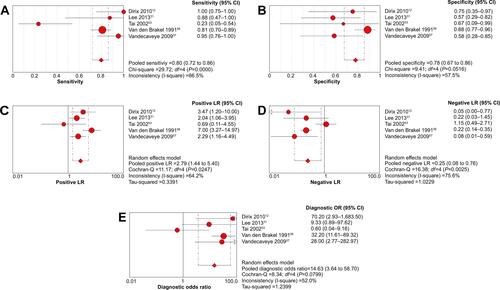
Figure S4 Meta-analysis of MRI for detecting cervical lymph node metastasis in head and neck cancer patients (patient as unit of analysis).
Abbreviations: MRI, magnetic resonance imaging; CI, confidence interval; df, degrees of freedom; LR, likelihood ratio; OR, odds ratio; SROC, summary receiver operating characteristic; AUC, area under the curve; SE, standard error.
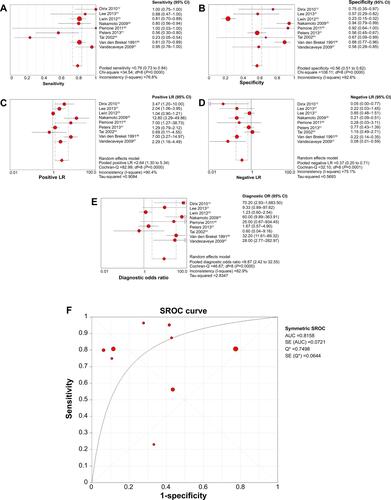
Table S1 Study characteristics of lymph node size per neck level
Table S2 Meta-analysis results on diagnostic efficacy of MRI on size of metastatic lymph nodes
Table S3 Meta-analysis results on diagnostic efficacy of CT on size of metastatic lymph nodes
References
- JemalASiegelRXuJWardECancer statistics, 2010CA Cancer J Clin201160527730020610543
- FooteRLOlsenKDDavisDLBase of tongue carcinoma: patterns of failure and predictors of recurrence after surgery aloneHead Neck19931543003078360051
- FerlitoARinaldoARobbinsKTChanging concepts in the surgical management of the cervical node metastasisOral Oncol200339542943512747966
- TankéréFCamprouxABarryBPrognostic value of lymph node involvement in oral cancers: a study of 137 casesLaryngoscope2000110122061206511129021
- ShahJCervical lymph node metastases: diagnostic, therapeutic, and prognostic implicationsOncology199041061652149826
- GolderWALymph node diagnosis in oncologic imaging: a dilemma still waiting to be solvedOnkologie200427219419915138355
- O’BrienCJMcNeilEBMcMahonJDSignificance of clinical stage, extent of surgery, and pathologic findings in metastatic cutaneous squamous carcinoma of the parotid glandHead Neck200224541742212001070
- KauRJAlexiouCStimmerHArnoldWDiagnostic procedures for detection of lymph node metastases in cancer of the larynxORL J Otorhinolaryngol Relat Spec200062419920310859520
- CastelijnsJAVan den BrekelMWImaging of lymphadenopathy in the neckEur Radiol200212472773811960218
- CastelijnsJAVan den BrekelMWDetection of lymph node metastases in the neck: radiologic criteriaAJNR Am J Neuroradiol20012213411158879
- HaoSPNgSHMagnetic resonance imaging versus clinical palpation in evaluating cervical metastasis from head and neck cancerOtolaryngol Head Neck Surg2000123332432710964315
- SternWBSilverCEZeiferBAPerskyMSHellerKSComputed tomography of the clinically negative neckHead Neck19901221091132312275
- KitagawaYNishizawaSSanoKProspective comparison of 18F-FDG PET with conventional imaging modalities (MRI, CT, and 67Ga scintigraphy in assessment of combined intraarterial chemotherapy and radiotherapy for head and neck carcinomaJ Nucl Med200344219820612571209
- SchöderHCarlsonDLKrausDH18F-FDG PET/CT for detecting nodal metastases in patients with oral cancer staged N0 by clinical examination and CT/MRIJ Nucl Med200647575576216644744
- LiHChenTWLiZLTumour size of resectable oesophageal squamous cell carcinoma measured with multidetector computed tomography for predicting regional lymph node metastasis and N stageEur Radiol201222112487249322653286
- RumboldtZGordonLGordonLBonsallRAckermannSImaging in head and neck cancerCurr Treat Options Oncol200671233416343366
- ChandawarkarRYKakegawaTFujitaHYamanaHHayabuthiNComparative analysis of imaging modalities in the preoperative assessment of nodal metastasis in esophageal cancerJ Surg Oncol19966132142178637210
- EscottEJRaoVMKoWDGuitierrezJEComparison of dynamic contrast-enhanced gradient-echo and spin-echo sequences in MRI of head and neck neoplasmsAJNR Am J Neuroradiol1997188141114199296179
- HamsbergerHRHandbook of Head and Neck ImagingChicagoMosby Year-Book1995283298
- LefebvreCManheimerEGlanvilleJSearching for studiesCochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 5.1.0EnglandThe Cochrane Collaboration20116.16.43
- WhitingPFRutjesAWWestwoodMEQUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studiesAnn Intern Med2011155852953622007046
- LauJIoannidisJPSchmidCHQuantitative synthesis in systematic reviewsAnn Intern Med199712798208269382404
- HigginsJPThompsonSGDeeksJJAltmanDGMeasuring inconsistency in meta-analysesBMJ200332741455756012958120
- HigginsJThompsonSDeeksJAltmanDStatistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practiceJ Health Serv Res Policy200271516111822262
- SchmidaCHStarkaPCBerlinbJALandaisPLauJMeta-regression detected association between heterogeneous treatment effects and study-level, but not patient-level, factorsJ Clin Epidemiol200457768369715358396
- ZamoraJAbrairaVMurielAKhanKCoomarasamyAMeta-DiSc: a software for meta-analysis of test accuracy dataBMC Med Res Methodol200663116836745
- DeeksJJHigginsJPAltmanDGAnalysing data and undertaking meta-analysesCochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 5.1.0EnglandThe Cochrane Collaboration20119.19.43
- AdamsSBaumRPStuckensenTBitterKHörGProspective comparison of 18F-FDG PET with conventional imaging modalities (CT, MRI, US) in lymph node staging of head and neck cancerEur J Nucl Med1998259125512609724374
- AkoğluEDutipekMBekişRAssessment of cervical lymph node metastasis with different imaging methods in patients with head and neck squamous cell carcinomaJ Otolaryngol200534638439416343398
- OkumuraKFujimotoYHasegawaY[Retropharyngeal node metastasis in cancer of the oropharynx and hypopharynx: analysis of retropharyngeal node dissection regarding preoperative radiographic diagnosis]Nihon Jibiinkoka Gakkai Kaiho19981015573577 Japanese9642997
- AnzaiYBlackwellKEHirschowitzSLInitial clinical experience with dextran-coated superparamagnetic iron oxide for detection of lymph node metastases in patients with head and neck cancerRadiology199419237097157520182
- De BondtRBHoeberigsMCNelemansPJDiagnostic accuracy and additional value of diffusion-weighted imaging for discrimination of malignant cervical lymph nodes in head and neck squamous cell carcinomaNeuroradiology200951318319219137282
- BraamsJWPruimJNikkelsPGNodal spread of squamous cell carcinoma of the oral cavity detected with PET-tyrosine, MRI and CTJ Nucl Med19963768979018683307
- BraamsJWPruimJFrelingNJDetection of lymph node metastases of squamous-cell cancer of the head and neck with FDG-PET and MRIJ Nucl Med19953622112167830116
- BruschiniPGiorgettiABruschiniLPositron emission tomography (PET) in the staging of head neck cancer: comparison between PET and CTActa Otorhinolaryngol Ital200323644645315198047
- CurtinHDIshwaranHMancusoAAComparison of CT and MRI imaging in staging of neck metastasesRadiology199820711231309530307
- DammannFHorgerMMueller-BergMRational diagnosis of squamous cell carcinoma of the head and neck region: comparative evaluation of CT, MRI, and 18FDG PETAJNR Am J Roentgenol2005184413261331
- DingZXLiangBLShenJ[Magnetic resonance imaging diagnosis of cervical lymph node metastasis from lingual squamous cell carcinoma]Ai Zheng2005242199203 Chinese15694033
- DirixPVandecaveyeVDe KeyzerFDiffusion-weighted MRI for nodal staging of head and neck squamous cell carcinoma: impact on radiotherapy planningInt J Radiat Oncol Biol Phys201076376176619540069
- EidaSSumiMYonetsuKKimuraYNakamuraTCombination of helical CT and Doppler sonography in the follow-up of patients with clinical N0 stage neck disease and oral cancerAJNR Am J Neuroradiol200324331231812637273
- FanWYSunJWEvaluation of enhanced CT on the cervical lymph node metastasis of head and neck neoplasmsChinese Journal of Clinical Healthcare20069236237 Chinese
- FukunariFOkamuraKZezeRCervical lymph nodes with or without metastases from oral squamous carcinoma: a correlation of MRI findings and histopathologic architectureOral Surg Oral Med Oral Pathol Oral Radiol Endod2010109689089920299250
- GrossNDWeissmanJLTalbotJMMRI detection of cervical metastasis from differentiated thyroid carcinomaLaryngoscope200111111 Pt 11905190911801967
- GuYFQiuWLLuoJCComparison on MRI and CT for Diagnosing Cervical Lymph Node MetastasisJournal of Shang Hai Tie Dao University2000213336 Chinese
- GuenzelTFranzenAWiegandSThe value of PET compared to MRI in malignant head and neck tumorsAnticancer Res20133331141114623482793
- GuoBShuDLRanWA [Clinical Study of Early-stage-diagnosis in Cervical Lymph Node Metastasis of Oral Carcinoma Using MRI]International Medicine and Health Guidance News2002122526 Chinese
- HannahAScottAMTochon-DanguyHEvaluation of 18 F-fluorodeoxyglucose positron emission tomography and computed tomography with histopathologic correlation in the initial staging of head and neck cancerAnn Surg2002236220821712170026
- HaoSPNgSHMagnetic resonance imaging versus clinical palpation in evaluating cervical metastasis from head and neck cancerOtolaryngol Head Neck Surg2000123332432710964315
- HafidhMALacyPDHughesJPDuffyGTimonCVEvaluation of the impact of addition of PET to CT and MRI scanning in the staging of patients with head and neck carcinomasEur Arch Otorhinolaryngol2006263985385916724209
- HlawitschkaMNeiseEBredowJFDG-PET in the pretherapeutic evaluation of primary squamous cell carcinoma of the oral cavity and the involvement of cervical lymph nodesMol Imaging Biol200241919814538052
- HoffmanHTQuetsJToshiakiTFunctional magnetic resonance imaging using iron oxide particles in characterizing head and neck adenopathyLaryngoscope200011091425143010983936
- JeongHSBaekCHSonYIUse of integrated 18F-FDG PET/CT to improve the accuracy of initial cervical nodal evaluation in patients with head and neck squamous cell carcinomaHead Neck200729320321017111430
- KauRJAlexiouCLaubenbacherCLymph node detection of head and neck squamous cell carcinomas by positron emission tomography with Fluorodeoxyglucose F 18 in a routine clinical settingArch Otolaryngol Head Neck Surg1999125121322132810604409
- KawaiYSumiMNakamuraTTurbo short tau inversion recovery imaging for metastatic node screening in patients with head and neck cancerAJNR Am J Neuroradiol20062761283128716775280
- KeZLiuMLiuYDiagnostic value of 18F-FDG PET/CT in the detection of the cervical lymph nodes metastasisLin Chuang Er Bi Yan Hou Ke Za Zhi2006206243245 Chinese16739373
- KrabbeCADijkstraPUPruimJFDG PET in oral and oropharyngeal cancer. Value for confirmation of N0 neck and detection of occult metastasesOral Oncol2008441313617306603
- LaubenbacherCSaumweberDWagner-ManslauCComparison of fluorine-18-fluorodeoxyglucose PET, MRI and endoscopy for staging head and neck squamous-cell carcinomasJ Nucl Med19953610174717577562038
- LeeMCTsaiHYChuangKSLiuCKChenMKPrediction of nodal metastasis in head and neck cancer using a 3T MRI ADC mapAJNR Am J Neuroradiol201334486486922997167
- LuHJRibere-BrugelLydiaEmmanuelITThe comparison of PET/CT with contrast enhanced CT in the assessment of cervical lymph nodes in head and neck cancerModern Oncology20071515551557 Chinese
- LwinCTHanlonRLoweDAccuracy of MRI in prediction of tumour thickness and nodal stage in oral squamous cell carcinomaOral Oncol201248214915422154129
- McGuirtWWilliamsDW3rdKeyesJWJrA comparative diagnostic study of head and neck nodal metastases using positron emission tomographyLaryngoscope19951054 Pt 13733757715380
- NakamotoYTamaiKSagaTClinical value of image fusion from MRI and PET in patients with head and neck cancerMol Imaging Biol2009111465318769975
- NishimuraHTanigawaNHiramatsuMPreoperative esophageal cancer staging: magnetic resonance imaging of lymph node with ferumoxtran-10, an ultrasmall superparamagnetic iron oxideJ Am Coll Surg2006202460461116571430
- Valdés OlmosRAKoopsWLoftusBMCorrelative 201Tl SPECT, MRI and ex vivo 201Tl uptake in detecting and characterizing cervical lymphadenopathy in head and neck squamous cell carcinomaJ Nucl Med19994091414141910492358
- OuYQLinYMagnetic resonance imaging diagnosis of 24 cases of cervical lymph node metastasis from oral carcinomaFujian Med J2936 Chinese
- PaulusPSambonAVivegnisD18FDG-PET for the assessment of primary head and neck tumors: clinical, computed tomography, and histopathological correlation in 38 patientsLaryngoscope199810810157815839778305
- PerroneAGuerrisiPIzzoLDiffusion-weighted MRI in cervical lymph nodes: differentiation between benign and malignant lesionsEur J Radiol201177228128619716671
- PetersTTCastelijnsJALjumanovicRDiagnostic value of CT and MRI in the detection of paratracheal lymph node metastasisOral Oncol201248545045522226512
- PoharSBrownRNewmanNWhat does PET imaging add to conventional staging of head and neck cancer patients?Int J Radiat Oncol Biol Phys200768238338717379443
- RenKZhangJRMaSSCT-Pathologic Correlative Study on the Cervical Lymph Node Metastasis of Laryngeal CancerChinese J Med Imaging20008347351 Chinese
- SchwartzDLFordERajendranJFDG-PET/CT imaging for preradiotherapy staging of head-and-neck squamous cell carcinomaInt J Radiat Oncol Biol Phys200561112913615629603
- Curvo-SemedoLDinizMMiguéisJUSPIO-enhanced magnetic resonance imaging for nodal staging in patients with head and neck cancerJ Magn Reson Imaging200624112313116755542
- SeitzOChambron-PinhoNMiddendorpM18F-Fluorodeoxyglucose-PET/CT to evaluate tumor, nodal disease, and gross tumor volume of oropharyngeal and oral cavity cancer: comparison with MRI imaging and validation with surgical specimenNeuroradiology2009511067768619727695
- StokkelMPten BroekFWHordijkGJKooleRvan RijkPPPreoperative evaluation of patients with primary head and neck cancer using dual-head 18fluorodeoxyglucose positron emission tomographyAnn Surg2000231222923410674615
- StuckensenTKovácsAFAdamsSBaumRPStaging of the neck in patients with oral cavity squamous cell carcinomas: a prospective comparison of PET, ultrasound, CT and MRIJ Craniomaxillofac Surg200028631932411465137
- SumiMKimuraYSumiTNakamuraTDiagnostic performance of MRI relative to CT for metastatic nodes of head and neck squamous cell carcinomasJ Magn Reson Imaging20072661626163317968896
- SumiMVan CauterenMNakamuraTMRI microimaging of benign and malignant nodes in the neckAJR Am J Roentgenol2006186374975716498102
- SumiMSakihamaNSumiTDiscrimination of metastatic cervical lymph nodes with diffusion-weighted MRI imaging in patients with head and neck cancerAJNR Am J Neuroradiol20032481627163413679283
- SunJTZhangZXZhangWJDiagnosis of molecular imaging on head and neck carcinoma and cercical lymph node metastasisChinese Journal of Coal Industry Medicine20131610491052 Chinese
- TaiCJShiauYCTsaiMHDetection of cervical lymph node metastases in nasopharyngeal carcinomas: comparison between technetium-99m methoxyisobutylisonitrile single photon emission computed tomography and magnetic resonance imagingNeoplasma200249425125412382024
- TakashimaSSoneSTakayamaFPapillary thyroid carcinoma: MRI diagnosis of lymph node metastasisAJNR Am J Neuroradiol19981935095139541309
- TuliHSSinghBPrasadVDiagnostic accuracy of 99mTc-MIBI-SPECT in the detection of lymph node metastases in patients with carcinoma of the tongue: comparison with computed tomography and MRINucl Med Commun200829980380818677208
- Van den BrekelMWCastelijnsJACrollGAMagnetic resonance imaging vs palpation of cervical lymph node metastasisArch Otolaryngol Head Neck Surg199111766636732036191
- VandecaveyeVDe KeyzerFVander PoortenVHead and neck squamous cell carcinoma: value of diffusion-weighted MRI imaging for nodal stagingRadiology2009251113414619251938
- WangQTakashimaSFukudaHDetection of medullary thyroid carcinoma and regional lymph node metastases by magnetic resonance imagingArch Otolaryngol Head Neck Surg1999125884284810448729
- WideJMWhiteDWWoolgarJAMagnetic resonance imaging in the assessment of cervical nodal metastasis in oral squamous cell carcinomaClin Radiol1999542909410050735
- WilsonGRMcLeanNRChippindaleAThe role of MRI scanning in the diagnosis of cervical lymphadenopathyBr J Plast Surg19944731751798193855
- WuYQFanXCDengYValue of Spiral CT Scan on Cervical Lymph node Metastasis of Laryngo and Hypolaryngo carcinomaHei Long Jiang Medical Journal34761763 Chinese
- YoonDYHwangHSChangSKCT, MRI, US, 18F-FDG PET/CT, and their combined use for the assessment of cervical lymph node metastases in squamous cell carcinoma of the head and neckEur Radiol200919363464218843493
- YuanYGHanDMFanEZThe evaluation of cervical lymph node metastasis of laryngeal cancer using magnetic resonance imaging (MRI)Lin Chuang Er Bi Yan Hou Ke Za Zhi20001410449451 Chinese12563714
- ShumJWDierksEJEvaluation and Staging of the Neck in Patients with Malignant DiseaseOral Maxillofac Surg Clin North Am201426220922124656885
- SunFLiYFLiuJHXiongYImpact of postoperative adjuvant therapy on prognosis of low-risk cervical cancer: analysis of 208 casesNan Fang Yi Ke Da Xue Xue Bao201434401405 Chinese24670458
- LindbergRDistribution of cervical lymph node metastases from squamous cell carcinoma of the upper respiratory and digestive tractsCancer1972296144614495031238
- BoccaECalearoCde VincentiisIOccult metastases in cancer of the larynx and their relationship to clinical and histological aspects of the primary tumor: a four year multicentric researchLaryngoscope1984948108610906748835
- FriedmanMRobertsNKirshenbaumGColomboJNodal size of metastatic squamous cell carcinoma of the neckLaryngoscope199310388548568361287
- JohnsonJTA surgeon looks at cervical lymph nodesRadiology199017536076102188292
Disclosure
The first and corresponding authors had full access to all of the data in the study and had final responsibility for the decision to submit for publication. The authors have no conflicts of interest in this work.
References
- AdamsSBaumRPStuckensenTProspective comparison of 18F-FDG PET with conventional imaging modalities (CT, MRI, US) in lymph node staging of head and neck cancerEur J Nucl Med199825125512609724374
- AkoğluEDutipekMBekişRAssessment of cervical lymph node metastasis with different imaging methods in patients with head and neck squamous cell carcinomaJ Otolaryngol20053438439416343398
- OkumuraKFujimotoYHasegawaYRetropharyngeal node metastasis in cancer of the oropharynx and hypopharynx: analysis of retropharyngeal node dissection regarding preoperative radiographic diagnosis [Article in Japanese]Nihon Jibiinkoka Gakkai Kaiho19981015735779642997
- AnzaiYBlackwellKEHirschowitzSLInitial clinical experience with dextran-coated superparamagnetic iron oxide for detection of lymph node metastases in patients with head and neck cancerRadiology19941927097157520182
- De BondtRBHoeberigsMCNelemansPJDiagnostic accuracy and additional value of diffusion-weighted imaging for discrimination of malignant cervical lymph nodes in head and neck squamous cell carcinomaNeuroradiology20095118319219137282
- BraamsJWPruimJNikkelsPGNodal spread of squamous cell carcinoma of the oral cavity detected with PET-tyrosine, MRI and CTJ Nucl Med1996378979018683307
- BraamsJWPruimJFrelingNJDetection of lymph node metastases of squamous-cell cancer of the head and neck with FDG-PET and MRIJ Nucl Med1995362112167830116
- BruschiniPGiorgettiABruschiniLPositron emission tomography (PET) in the staging of head neck cancer: comparison between PET and CTActa Otorhinolaryngol Ital20032344645315198047
- CurtinHDIshwaranHMancusoAAComparison of CT and MRI imaging in staging of neck metastasesRadiology19982071231309530307
- DammannFHorgerMMueller-BergMRational diagnosis of squamous cell carcinoma of the head and neck region: comparative evaluation of CT, MRI, and 18FDG PETAJNR Am J Roentgenol200518413261331
- DingZXLiangBLShenJMagnetic resonance imaging diagnosis of cervical lymph node metastasis from lingual squamous cell carcinoma [Article in Chinese]Ai Zheng20052419920315694033
- DirixPVandecaveyeVDe KeyzerFDiffusion-weighted MRI for nodal staging of head and neck squamous cell carcinoma: impact on radiotherapy planningInt J Radiat Oncol Biol Phys20107676176619540069
- EidaSSumiMYonetsuKCombination of helical CT and Doppler sonography in the follow-up of patients with clinical N0 stage neck disease and oral cancerAJNR Am J Neuroradiol20032431231812637273
- FanWYSunJWEvaluation of enhanced CT on hte cervical lymph node metastasis of head and neck neoplasmsChinese Journal of Clinical Healthcare [Article in Chinese]20069236237
- FukunariFOkamuraKZezeRCervical lymph nodes with or without metastases from oral squamous carcinoma: a correlation of MRI findings and histopathologic architectureOral Surg Oral Med Oral Pathol Oral Radiol Endod201010989089920299250
- GrossNDWeissmanJLTalbotJMMRI detection of cervical metastasis from differentiated thyroid carcinomaLaryngoscope20011111905190911801967
- GuYFQiuWLLuoJCComparison on MRI and CT for Diagnosing Cervical Lymph Node Metastasis [Article in Chinese]Journal of Shang Hai Tie Dao University2000213336
- GuenzelTFranzenAWiegandSThe value of PET compared to MRI in malignant head and neck tumorsAnticancer Res2013331141114623482793
- GuoBShuDLRanWA Clinical Study of Early-stage-diagnosis in Cervical Lymph Node Metastasis of Oral Carcinoma Using MRI [Article in Chinese]International Medicine and Health Guidance News2002122526
- HannahAScottAMTochon-DanguyHEvaluation of 18F-fluorodeoxyglucose positron emission tomography and computed tomography with histopathologic correlation in the initial staging of head and neck cancerAnn Surg200223620821712170026
- HaoSPNgSHMagnetic resonance imaging versus clinical palpation in evaluating cervical metastasis from head and neck cancerOtolaryngol Head Neck Surg200012332432710964315
- HafidhMALacyPDHughesJPEvaluation of the impact of addition of PET to CT and MRI scanning in the staging of patients with head and neck carcinomasEur Arch Otorhinolaryngol200626385385916724209
- HlawitschkaMNeiseEBredowJFDG-PET in the pretherapeutic evaluation of primary squamous cell carcinoma of the oral cavity and the involvement of cervical lymph nodesMol Imaging Biol20024919814538052
- HoffmanHTQuetsJToshiakiTFunctional magnetic resonance imaging using iron oxide particles in characterizing head and neck adenopathyLaryngoscope20001101425143010983936
- JeongHSBaekCHSonYIUse of integrated 18F-FDG PET/CT to improve the accuracy of initial cervical nodal evaluation in patients with head and neck squamous cell carcinomaHead Neck20072920321017111430
- KauRJAlexiouCLaubenbacherCLymph node detection of head and neck squamous cell carcinomas by positron emission tomography with Fluorodeoxyglucose F 18 in a routine clinical settingArch Otolaryngol Head Neck Surg19991251322132810604409
- KawaiYSumiMNakamuraTTurbo short tau inversion recovery imaging for metastatic node screening in patients with head and neck cancerAJNR Am J Neuroradiol2006271283128716775280
- KeZLiuMLiuYDiagnostic value of 18F-FDG PET/CT in the detection of the cervical lymph nodes metastasis [Article in Chinese]Lin Chuang Er Bi Yan Hou Ke Za Zhi20062024324516739373
- KrabbeCADijkstraPUPruimJFDG PET in oral and oropharyngeal cancer. Value for confirmation of N0 neck and detection of occult metastasesOral Oncol200844313617306603
- LaubenbacherCSaumweberDWagner-ManslauCComparison of fluorine-18-fluorodeoxyglucose PET, MRI and endoscopy for staging head and neck squamous-cell carcinomasJ Nucl Med199536174717577562038
- LeeMCTsaiHYChuangKSPrediction of nodal metastasis in head and neck cancer using a 3T MRI ADC mapAjnr Am J Neuroradiol20133486486922997167
- LUHJLydia RIBERE – BRUGEL, Emmanue lITTThe comparison of PET/CT with contrast enhanced CT in the assessment of cervical lymph nodes in head and neck cancer [Article in Chinese]Modern Oncology20071515551557
- LwinCTHanlonRLoweDAccuracy of MRI in prediction of tumour thickness and nodal stage in oral squamous cell carcinomaOral Oncol20124814915422154129
- McGuirtWWilliamsDWIIIKeyesJWJrA comparative diagnostic study of head and neck nodal metastases using positron emission tomographyLaryngoscope19951053733757715380
- NakamotoYTamaiKSagaTClinical value of image fusion from MRI and PET in patients with head and neck cancerMol Imaging Biol200911465318769975
- NishimuraHTanigawaNHiramatsuMPreoperative esophageal cancer staging: magnetic resonance imaging of lymph node with ferumoxtran-10, an ultrasmall superparamagnetic iron oxideJ Am Coll Surg200620260461116571430
- OlmosRAKoopsWLoftusBMCorrelative 201Tl SPECT, MRI and ex vivo 201Tl uptake in detecting and characterizing cervical lymphadenopathy in head and neck squamous cell carcinomaJ Nucl Med1999401414141910492358
- OuYQMLinYMagnetic resonance imaging diagnosis of 24 cases of cervical lymph node metastasis from oral carcinoma [Article in Chinese]Fu jian Med J2936
- PaulusPSambonAVivegnisD18FDG-PET for the assessment of primary head and neck tumors: clinical, computed tomography, and histopathological correlation in 38 patientsLaryngoscope1998108157815839778305
- PerroneAGuerrisiPIzzoLDiffusion-weighted MRI in cervical lymph nodes: differentiation between benign and malignant lesionsEur J Radiol20117728128619716671
- PetersTTCastelijnsJALjumanovicRDiagnostic value of CT and MRI in the detection of paratracheal lymph node metastasisOral Oncol20124845045522226512
- PoharSBrownRNewmanNWhat does PET imaging add to conventional staging of head and neck cancer patients?Int J Radiat Oncol Biol Phys20076838338717379443
- RenKZhangJRMaSSCT-Pathologic Correlative Study on the Cervical Lymph Node Metastasis of Laryngeal Cancer [Article in Chinese]Chines e J Med Imaging20008347351
- SchwartzDLFordERajendranJFDG-PET/CT imaging for preradiotherapy staging of head-and-neck squamous cell carcinomaInt J Radiat Oncol Biol Phys20056112913615629603
- Curvo-SemedoLDinizMMiguéisJUSPIO-enhanced magnetic resonance imaging for nodal staging in patients with head and neck cancerJ Magn Reson Imaging20062412313116755542
- SeitzOChambron-PinhoNMiddendorpM18F-Fluorodeoxyglucose-PET/CT to evaluate tumor, nodal disease, and gross tumor volume of oropharyngeal and oral cavity cancer: comparison with MRI imaging and validation with surgical specimenNeuroradiology20095167768619727695
- StokkelMPten BroekFWHordijkGJPreoperative evaluation of patients with primary head and neck cancer using dual-head 18fluorodeoxyglucose positron emission tomographyAnn Surg200023122923410674615
- StuckensenTKovácsAFAdamsSStaging of the neck in patients with oral cavity squamous cell carcinomas: a prospective comparison of PET, ultrasound, CT and MRIJ Craniomaxillofac Surg20002831932411465137
- SumiMKimuraYSumiTDiagnostic performance of MRI relative to CT for metastatic nodes of head and neck squamous cell carcinomasJ Magn Reson Imaging2007261626163317968896
- SumiMVan CauterenMNakamuraTMRI microimaging of benign and malignant nodes in the neckAJNR Am J Roentgenol2006186749757
- SumiMSakihamaNSumiTDiscrimination of metastatic cervical lymph nodes with diffusion-weighted MRI imaging in patients with head and neck cancerAJNR Am J Neuroradiol2003241627163413679283
- SunJTZhangZXZhangWJDiagnosis of molecular imaging on head and neck carcinoma and cercical lymph node metastasis [Article in Chinese]Chinese Journal of Coal Industry Medicine20131610491052
- TaiCJShiauYCTsaiMHDetection of cervical lymph node metastases in nasopharyngeal carcinomas: comparison between technetium-99m methoxyisobutylisonitrile single photon emission computed tomography and magnetic resonance imagingNeoplasma20024925125412382024
- TakashimaSSoneSTakayamaFPapillary thyroid carcinoma: MRI diagnosis of lymph node metastasisAJNR Am J Neuroradiol1998195095139541309
- TuliHSSinghBPrasadVDiagnostic accuracy of 99mTc-MIBI-SPECT in the detection of lymph node metastases in patients with carcinoma of the tongue: comparison with computed tomography and MRINucl Med Commun20082980380818677208
- Van den BrekelMWCastelijnsJACrollGAMagnetic resonance imaging vs palpation of cervical lymph node metastasisArch Otolaryngol Head Neck Surg19911176636732036191
- VandecaveyeVDe KeyzerFVander PoortenVHead and neck squamous cell carcinoma: value of diffusion-weighted MRI imaging for nodal stagingRadiology200925113414619251938
- WangQTakashimaSFukudaHDetection of medullary thyroid carcinoma and regional lymph node metastases by magnetic resonance imaging [Article in Chinese]Arch Otolaryngol Head Neck Surg199912584284810448729
- WideJMWhiteDWWoolgarJAMagnetic resonance imaging in the assessment of cervical nodal metastasis in oral squamous cell carcinomaClin Radiol199954909410050735
- WilsonGRMcLeanNRChippindaleAThe role of MRI scanning in the diagnosis of cervical lymphadenopathyBr J Plast Surg1994471751798193855
- WuYQFanXCDengYValue of Spiral CT Scan on Cervical Lymph node Metastasis of Laryngo and Hypolaryngo carcinoma [Article in Chinese]Hei Long Jiang Medical Journal34761763
- YoonDYHwangHSChangSKCT, MRI, US, 18F-FDG PET/CT, and their combined use for the assessment of cervical lymph node metastases in squamous cell carcinoma of the head and neckEur Radiol20091963464218843493
- YuanYGHanDMFanEZThe evaluation of cervical lymph node metastasis of laryngeal cancer using magnetic resonance imaging (MRI) [Article in Chinese]Lin Chuang Er Bi Yan Hou Ke Za Zhi20001444945112563714