Abstract
Purpose
Patients with a high risk of prostate carcinoma typically have higher rates of positive surgical margins and biochemical failure following radical prostatectomy and adjuvant hormone therapy. In this study, we assessed the effects of neoadjuvant hormone therapy (NHT) on prostate carcinoma in high-risk patients following robotic-assisted radical prostatectomy (RARP).
Methods
This retrospective study investigated the medical records of 28 patients who underwent RARP between January 2009 and October 2013. Twenty-two patients underwent NHT prior to RARP. Furthermore, six patients did not undergo NHT prior to RARP. Parameters including age, operating time, blood loss, blood transfusion status, and cancer stage were checked against anatomical correlations. Potential predictors of prolonged operating time and prolonged surgical procedures were assessed using multiple logistic regressions.
Results
NHT was shown to be an independent predictor of prolonged total operating time. Tumor stage alterations did not appear to be associated with NHT followed by RARP. The patients who underwent NHT were not more likely to have positive surgical margins, and an increase in patients requiring blood transfusion was not seen.
Conclusion
NHT appears to increase operative time during RARP. However, the perioperative morbidity of NHT patients undergoing RARP appears to be equivalent with that of non-NHT patients.
Introduction
The widespread use of the prostate-specific antigen (PSA) test has improved prostate cancer detection rates.Citation1 High-risk prostate carcinoma (PC) patients are at considerable risk of biochemical failure following radical prostatectomy, and surgical margins are more likely to be positive. This has raised questions regarding the need for neoadjuvant treatments. Radical retropubic prostatectomy (RP) has been shown to provide excellent long-term disease control in patients with clinically localized PC.Citation1 Laparoscopic prostatectomy, first described by Schuessler et alCitation2 is a standard treatment for localized PC, which is a minimally invasive surgery but still includes advantages associated with surgical removal and pathologic tumor staging. Robotic-assisted radical prostatectomy (RARP) and laparoscopic prostatectomy are equal when considering surgical and oncological outcomes.Citation3,Citation4 In Taiwan, RARP is more widely used to treat localized prostate cancer.Citation4
Using antiandrogen therapy to treat patients with PC who have undergone RARP remains controversial. The use of neoadjuvant hormone therapy (NHT) has also failed to gain widespread acceptance as a treatment for PC. Studies of patients who underwent NHT for 3 months demonstrated a decrease in pathologic stage without improvement in PSA for disease-free survival.Citation5,Citation6 Nonetheless, recent studies have shown that extending the duration of NHT therapy (>8 months) or combining it with antiandrogen therapy can enhance the effectiveness of this treatment technique. However, antiandrogen therapy has been shown to induce prostatic apoptosis associated with prostatic and periprostatic fibrosis.Citation7 This can lead to greater numbers of patients with positive tumor margins and higher morbidity rates following RARP. A lack of data has made it impossible to conclude whether periprostatic changes render retropubic prostatectomy more difficult. One previous study reported that NHT may decrease the seminal vesicle invasion rate.Citation8 However, few large-scale studies have investigated the impact of NHT on the operating parameters of laparoscopic prostatectomy. The aim of this study is to evaluate the effects of NHT on PC in high-risk patients following RARP. In addition, we tried to identify the predictors of prolonged operating time.
Materials and methods
Between January 2009 and October 2013, a total of 28 men were scheduled for RARP to treat localized PC. All the patients signed a consent form for the treatment. Basic patient characteristics are listed in . They included oral-form antiandrogen medication (bicalutamide 50 mg once a day) use, age, diabetes mellitus, hypertension, albumin, PSA, hemoglobin, and volume of prostate. Twenty-two patients who had received at least 1 month of neoadjuvant bicalutamide monotherapy, 50 mg once daily, before RARP for prostate cancer were identified. The remaining six patients did not receive hormone therapy. All patients underwent a transrectal ultrasound–guided prostate biopsy. The patients who received antiandrogen therapy were aged between 58 years and 74 years, with a mean age of 66 years. Among those who did not undergo antiandrogen therapy, ages ranged from 54 years to 75 years, and the mean age was 62 years. The average prostate size and average PSA level in the group that received antiandrogens were 47 mL and 20.5 ng/mL, respectively, compared to 39 mL and 20.5 ng/mL in the group that did not receive antiandrogens.
Table 1 Baseline characteristics of the patients undergoing robotic-assisted radical prostatectomy
We recorded preoperative and perioperative clinical and pathologic data, including patient age, preoperative PSA status, biopsy Gleason grade, clinical stage, pathologic stage, blood loss (including through urine and intraoperative blood loss), and surgical margin status. No significant differences were observed between the two groups with regard to clinical characteristics. Oncologic results were evaluated by staging samples obtained during the operation in accordance with the TNM 2002 classification scheme. The last serum PSA level after operation was 4.5 (2.0–7.5 ng/mL) years. Chi-square test was used to test qualitative data, and Mann–Whitney U-test was used to test numerical variables. A P-value of <0.05 was considered significant.
Results
Clinical characteristics of patients are presented in . Mean age ± standard deviation of patients who received RARP alone was 61.8±9.1 years, and the mean age of patients who underwent NHT with RARP was 66±4.4 years (P=0.187). Mean serum PSA levels before prostate biopsy were similar between both the groups.
Significant differences were only observed in the duration of the operations. Specifically, the group that received RARP and NHT had an average operation time of 254 min, while the average operation time for the group that underwent just RARP was only 209 min (). It was conceivable that the blood loss in the NHT group would be more than the compared group; however, our findings found no significant difference (). No difference was observed between the groups with regard to prostate size, and no significant correlations were observed between hormone therapy and blood loss, blood transfusion volume, or a drop in hemoglobin levels. It is interesting to note that the percentage of down-and upstaging in hormone therapy is greater and less than that of nonhormone therapy, respectively (). In our study, severe perioperative complications such as wound infection, intestinal obstruction, great vessel injury, hallow organ injury, or rectal injury was not reported in either of the two groups. None of the patients had a conversion to an open procedure, and no patient mentioned any complaint about a remarkable stress urinary incontinence after the operation. Additionally, we did not observe any cases of mortality in this series, and no significant differences were observed with regards to positive surgical margins between the two groups, as shown in . Postoperative pathologic data revealed that tumor vessel invasion was zero percent in patients undergoing RARP and 9.1% in patients undergoing RARP with NHT (P=0.999). Perineural invasion occurred in three patients (50%) belonging to the group that received only RARP and in nine of the patients (40.9%) belonging to the group that received both RARP and NHT (P=0.99). Following the operation, no significant changes were observed in Gleason score for either group (P=0.584), Furthermore, postoperative medications did not differ among the two groups, and blood transfusion rates were also similar. However, operating times were significantly lower in the group that received only RARP than in the group that received both RARP and NHT (P=0.019). We used multiple logistic regressions to identify the independent factors affecting the total operating time. Our study results revealed that the patients who received antiandrogen treatment before RARP required more time to get through the operation. Furthermore, we found that among all the possible variables that may affect the total operating time, the using of antiandrogen was the only independent factor, as shown in .
Figure 1 Comparison of intraoperative times associated with robotic-assisted radical prostatectomy with or without neoadjuvant antiandrogen therapy.
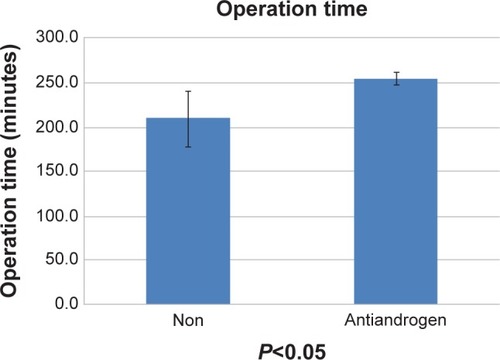
Table 2 Comparison of intraoperative, early, and late postoperative complications in patients who received RARP alone or in conjunction with neoadjuvant antiandrogen therapy
Table 3 Comparison of the two groups in the pathologic findings of robotic-assisted radical prostatectomy
Table 4 Multiple logistic regressions to evaluate the independent variables affecting operating time
Discussion
A consensus has yet to be reached regarding the effects of NHT on the operating conditions associated with retropubic prostatectomy. Some studies have reported that NHT decreases the operative parameters, thereby making the surgical procedure easier to perform.Citation9,Citation10 Other studies have reported no differences in operating times, blood loss, transfusion rates, and complication rates between patients who received NHT treatment and those who did not.Citation11,Citation12 Despite the potential of neoadjuvant therapy, the use of antiandrogen agent before definitive surgical treatment should be limited to clinical evidence. Nonetheless, a study that investigated androgen deprivation and docetaxel treatment prior to prostatectomy yielded encouraging results with regard to recurrence-free survival rates.Citation13
A previous study found that high body mass index and high prostate weight were independent predictors of prolonged total operating times in extraperitoneal laparoscopic radical prostatectomies.Citation14 However, that study did not find NHT to be a risk factor in prolonged operating time. In contrast, our findings showed a positive correlation between antiandrogen therapies and extended operating times. On the contrary, we did not find any significant correlations among body mass index, prostate weight, and operating time. We believe that adhesion is the main reason to prolong the operative time after hormone therapy. The morphological changes observed in antiandrogen-treated prostatic adenocarcinoma include programmed cell death, loss of glandular architecture, cytoplasmic vacuolization, nuclear pyknosis, and remarkable inflammatory response.Citation15 Therefore, the adhesions between the prostate and the surrounding tissue would be a great challenge during the operation. We found that it was more difficult to separate the prostate from the rectum and the neurovascular bundle in the NHT group, and as a result, it was more time consuming. Although the pathologic changes made it more difficult to complete the surgical procedure in the patients of the NHT group, by using robotic surgery, which is more precise in comparison to the traditional operation, no increased complication rate was found in the NHT group.
Current evidence supports the use of RARP as a treatment option for localized advanced PC; however, some researchers believe that NHT treatment can lead to potentially dangerous side effects, which make margins of the prostate capsule difficult to identify. Nonetheless, our data indicate that treatment with NHT for a period of 2–4 weeks is safe for patients with localized advanced PC. In this current study, no differences in preoperative risk were observed between the two groups (RARP alone versus RARP with NHT), as shown in . Additionally, no cases of comorbidity were included in the long-term NHT group. However, our study focused only on the perioperative impact of NHT for patients who received RARP and therefore lacked the long-term results. This is the disadvantage of our study, and the evaluation of the 5-year survival rate will be our goal in the future. Whether NHT treatment over longer periods may reduce positive surgical margin levels and help to improve cancer-free survival rates or not also needs a long-term follow-up period to verify.
Conclusion
Our results demonstrate that RARP is a safe and effective procedure for patients who have received NHT. The perioperative morbidity of NHT patients undergoing RARP appears to be equivalent to that of non-NHT patients. Patients who received NHT also demonstrated lower rates of positive surgical margins. Nonetheless, we found that prostate cancer patients who underwent antiandrogen therapy prior to surgical treatment had significantly longer operating times in comparison to those who did not. To prove the value of antiandrogen therapy prior to prostate cancer surgery, future research will need to investigate a greater number of cases. This excellent outcome makes a compelling argument for better definition of high-risk patients for further trials.
Acknowledgments
This research was supported by grants from the Chang Gung Memorial Hospital (CMRPG3D0311 and CMRPG392163) and the National Science Council, Taiwan, (NSC 101-2314-B-182A-099-MY3).
Disclosure
The authors report no conflicts of interest in this work.
References
- CarrollPRPrestiJCJrSmallERoachM3rdFocal therapy for prostate cancer 1996: maximizing outcomeUrology1997493A suppl84949123742
- SchuesslerWWSchulamPGClaymanRVKavoussiLRLaparoscopic radical prostatectomy: initial short-term experienceUrology19975068548579426713
- FicarraVNovaraGArtibaniWRetropubic, laparoscopic, and robotic-assisted radical prostatectomy: a systemic review and cumulative analysis of comparative studiesEur Urol2009551037106319185977
- WuSTTsuiKHTangSHLaparoscopic radical prostatectomy: initial experience of robotic surgery in TaiwanAnticancer Res2008284A1989199218649737
- SchuesslerWWSchulamPGClaymanRVKavoussiLRLaparoscopic radical prostatectomy: initial short-term experienceUrology19975068548579426713
- GleaveMEGoldenbergSLChinJLCanadian Uro-Oncology GroupRandomized comparative study of 3 versus 8-month neoadjuvant hormonal therapy before radical prostatectomy: biochemical and pathological effectsJ Urol20011662500506 discussion 506–50711458055
- BrownJAGarlitzCStrupSEHuboskySGGomellaLLaparoscopic radical prostatectomy after neoadjuvant hormonal therapy: an apparently safe and effective procedureJ Laparoendosc Adv Surg Tech A200414633533815684777
- SolowayMSPareekKSharifiRLupron Depot Neoadjuvant Prostate Cancer Study GroupNeoadjuvant androgen ablation before radical prostatectomy in cT2bNxMo prostate cancer: 5-year resultsJ Urol2002167111211611743286
- SchulmanCCSassineAMNeoadjuvant hormonal deprivation before radical prostatectomyEur Urol19932444504557507045
- SassineAMSchulmanCCNeoadjuvant hormonal deprivation before radical prostatectomyEur Urol199324suppl 246507505231
- MacfarlaneMTAbi-AadASteinADanellaJBelldegrunAde KernionJBNeoadjuvant hormonal deprivation in patients with locally advanced prostate cancerJ Urol199315011321347685421
- CivantosFSadekSObekCLaiSSolowayMNeoadjuvant hormonal therapy prior to radical prostatectomyMol Urol19993320120410851324
- ChiKNChinJLWinquistEKlotzLSaadFGleaveMEMulticenter phase II study of combined neoadjuvant docetaxel and hormone therapy before radical prostatectomy for patients with high risk localized prostate cancerJ Urol200818056557018554663
- ShelleyMDKumarSWiltTStaffurthJColesBMasonMDSystematic review and meta-analysis of randomized trials of neo-adjuvant hormone therapy for localized and locally advanced prostate carcinomaCancer Treat Rev200935191718926640
- ReuterVEPathological changes in benign and malignant prostatic tissue following androgen deprivation therapyUrology199749316229123731
