Abstract
Purpose
To investigate the impact of chemotherapy and/or radiotherapy on disease-free survival (DFS) and overall survival (OS) rates of patients with thymic carcinoma after complete resection.
Methods
Between 2001 and 2013, 54 patients with complete resection of thymic carcinoma in Hangzhou Cancer Hospital were retrospectively reviewed. The Kaplan–Meier method was used to evaluate the survival rates. The Cox proportional hazard model was used for multivariate analysis.
Results
Among the 54 patients, Masaoka stage I was observed in seven patients, II in 22 patients, and III in 25 patients. Sixteen patients received adjuvant chemotherapy (six with chemotherapy alone and ten with radiotherapy and chemotherapy), 25 patients received adjuvant radiotherapy, and 13 patients did not receive radiotherapy and/or chemotherapy. The 5-year DFS and OS rates for all patients were 63.0% and 73.4%, respectively. Univariate analysis revealed that radiotherapy was significantly associated with DFS and OS (P=0.014 and P=0.029, respectively), while adjuvant chemotherapy was not (P=0.122 and P=0.373, respectively). Multivariate analysis showed that adjuvant radiotherapy increased DFS (P=0.041), but not OS (P=0.051).
Conclusion
Complete resection followed by adjuvant radiotherapy increased disease-free rates of thymic carcinoma patients.
Introduction
Thymic carcinoma is a relatively rare mediastinal tumor.Citation1 Surgery is the standard treatment for early-stage thymic carcinoma, and complete resection is the most important prognostic factor for survival.Citation2,Citation3 Although chemotherapy and radiation are widely applied in thymic carcinoma, the role of adjuvant chemotherapy and/or radiotherapy after complete resection remains controversial with very few studies.Citation4–Citation6
According to the guidelines of the National Comprehensive Cancer Network, systemic chemotherapy was not recommended after complete resection of thymic carcinoma, but radiotherapy was recommended after complete tumor resection in stages II and III of thymic carcinoma; however, the recommended category is low. Studies focusing on adjuvant treatment after resection of thymic carcinoma are lacking now.Citation5
In this study, we retrospectively evaluated the prognosis and treatment of patients with completely resected thymic carcinoma and explored the impact of chemotherapy and/or radiotherapy on disease-free survival (DFS) and overall survival (OS) rates of patients with thymic carcinoma after complete resection.
Patients and methods
Methods
Fifty-four patients who had complete resection for thymic carcinoma between January 2001 and December 2013 in Hangzhou Cancer Hospital were included in the study. Based on the Masaoka staging system, the stage of thymic carcinoma was classified. Pathologically proven primary type C (WHO histological classification) thymic carcinoma by surgery. All patients underwent complete resection, and pathology proved no positive margins. No patients underwent induction chemotherapy or radiotherapy before surgery. Recurrence or metastases were confirmed using chest computed tomography (CT) as well as ultrasound and/or CT of the abdomen. The study was approved by the Ethics Committee of Hangzhou Cancer Hospital (Hangzhou, People’s Republic of China). All patients provided written informed consent for this study.
Follow-up
Surviving patients were followed every 3–6 months for the first 5 years and then annually. The history, physical examination, and chest CT scan were recorded during the follow-up time. Survival case was recorded from the first day of operation to the date of death or last follow-up time. December 2014 was the last censoring date for survival. The median time from surgery to the last censoring date was 72 months, ranging from 25 to 168 months.
Statistical analysis
The survival curves were generated using the Kaplan–Meier method and compared with log-rank test. The Cox proportional hazard model was applied for multivariate analysis. The statistical analysis using the SPSS Version 16 (SPSS Inc., Chicago, IL, USA) was performed.
Results
Patient characteristics
Patient characteristics and histological subtypes are listed in . The median age was 49 years (range, 22–74 years). Squamous cell carcinoma (70.4%) was the most common histological subtype followed by undifferentiated carcinoma and neuroendocrine tumors. Among the 54 patients, five patients had positive mediastinal lymph nodes at surgical resection. Performance score was 0 in 39 patients and 1 for 27.8% patients. Two young males (aged 31 years and 33 years) presented with myasthenia gravis at first diagnosis with elevated AChR-binding antibody levels. The pathology report confirmed no component of thymoma in these two cases.
Table 1 Demographic characteristics of the study population
Treatment after operation
All 54 patients underwent complete surgical resection. Sixteen patients underwent chemotherapy (six with only chemotherapy and ten with radiotherapy and chemotherapy), 25 patients received radiotherapy, and 13 patients did not receive radiotherapy and/or chemotherapy (). On day 1, the most common regimen was the combination of cyclophosphamide (400 mg/m2), adriamycin (40 mg/m2), and cisplatin (75 mg/m2) (n=8); the second common regimen was the combination of taxol (175 mg/m2) and cisplatin (75 mg/m2) (n=6); and other regimens included docetaxel (75 mg/m2) and cisplatin (75 mg/m2) (n=1) as well as vinorelbine (25 mg/m2) and cisplatin (75 mg/m2) (n=1). Two-dimensional radiotherapy planning system was used in eleven patients and three-dimensional conformal radiotherapy in 14 patients. The median dose was 54.2 Gy (range, 52–61.2 Gy). There were no differences among age (P=0.47), sex (P=0.52), Masaoka stage (P=0.76), and histology (P=0.31) between the radiotherapy and no-radiotherapy patients.
Factors affecting OS by univariate and multivariate analyses
The 5-year DFS and OS rates for all patients were 63.0% and 73.4%, respectively. The results of univariate analysis for DFS and OS are listed in . Age, sex, chemotherapy, histology, myasthenia gravis, and Masaoka stage showed no significant association with DFS and OS (), while radiotherapy showed significant association with DFS and OS (P=0.014 and P=0.029, respectively) ( and ). There were significant differences for DFS among the radiotherapy alone, radiotherapy and chemotherapy, chemotherapy alone, and no adjuvant treatment patients (P=0.013), but not for OS (P=0.054) ( and ).
Figure 1 DFS in radiotherapy group and no-radiotherapy treatment group (P=0.014).
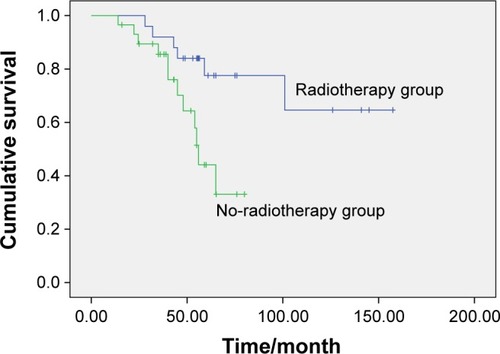
Figure 2 OS in radiotherapy group and no-radiotherapy treatment group (P=0.029).
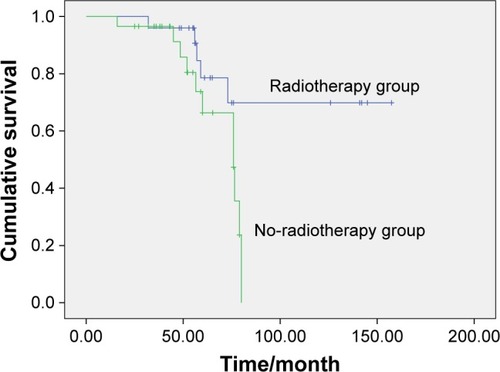
Figure 3 DFS among the radiotherapy alone, radiotherapy and chemotherapy, chemotherapy alone, and no adjuvant treatment group (P=0.013).
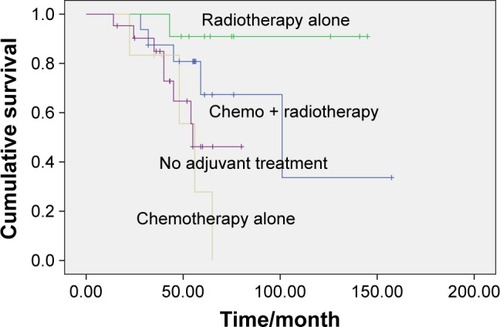
Figure 4 OS among the radiotherapy alone, radiotherapy and chemotherapy, chemotherapy alone, and no adjuvant treatment group (P=0.054).
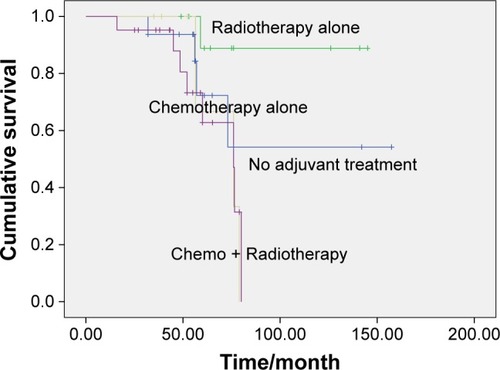
Table 2 Univariate analysis of the patient survival according to the clinicopathologic characteristics
A multivariate Cox regression model showed that adjuvant radiotherapy and stage significantly influenced DFS, but not OS ().
Table 3 Multivariate survival analysis for DFS and OS
Discussion
Due to the rarity of thymic tumors, randomized controlled data are lacking, and the available evidence on adjuvant treatment comes from small retrospective studies. Our results suggest that adjuvant radiotherapy after complete resection could impact the DFS rates of thymic carcinoma patients.
The role of postoperative radiation therapy and chemotherapy in reducing the rate of recurrence and increasing the OS remains controversial. A multi-institutional retrospective studyCitation7 demonstrated that adjuvant radiation does not improve the OS rate in patients with completely resected thymic carcinoma. In contrast, another multi-institutional retrospective study by Omasa et al showed that postoperative radiotherapy increased relapse-free survival for stages II and III thymic carcinoma.Citation8 Patel et al reported the results of 1,464 patients with thymic carcinoma from centers that participated in the Surveillance, Epidemiology, and End Results program,Citation9 which indicated that OS significantly improved with radiotherapy, and an improved cause-specific survival trend was observed. In this study, the patients benefited from adjuvant radiotherapy, which is consistent with the findings of Omasa et al.
Adjuvant chemotherapy in some studies showed a benefit of reducing distant metastasis rate and prolonging OS and others did not indicate any role.Citation5,Citation10–Citation16 Song and ZhangCitation5 and Sun et alCitation16 found no DFS and OS differences in completely resected thymic carcinoma patients receiving surgery alone versus surgery plus adjuvant chemotherapy. Our series also revealed that adjuvant chemotherapy showed no significant effect in completely resected thymic carcinoma.
Our study is limited by its retrospective nature and with a small number of patients included. However, considering the rarity of the disease, the report of 54 cases is regarded as a relatively large study; our retrospective study may also be meaningful.
Conclusion
In summary, adjuvant radiotherapy after complete resection of thymic carcinoma could increase DFS. Prospective trials are required to further elucidate the effect and survival after adjuvant chemotherapy and radiation.
Disclosure
The authors report no conflicts of interest in this work.
References
- EngelsEAEpidemiology of thymoma and associated malignanciesJ Thorac Oncol201051S260S26520859116
- SongZZhangYOutcomes after surgical resection of thymic carcinoma: a study from a single tertiary referral centreEur J Surg Oncol201440111523152724953416
- VenutaFAnileMDisoDThymoma and thymic carcinomaEur J Cardiothorac Surg2010371132519615917
- ShenSAiXLuSLong-term survival in thymic epithelial tumors: a single-center experience from ChinaJ Surg Oncol2013107216717222996015
- SongZZhangYAdjuvant therapy in stage II thymic carcinomaJ Cancer Res Clin Oncol2014140234935224305755
- FanCFengQChenYPostoperative radiotherapy for completely resected Masaoka stage III thymoma: a retrospective study of 65 cases from a single institutionRadiat Oncol20131319923937886
- KondoKMondenYTherapy for thymic epithelial tumors: a clinical study of 1,320 patients from JapanAnn Thorac Surg200376387888412963221
- OmasaMDateHSozuTJapanese Association for Research on the ThymusPostoperative radiotherapy is effective for thymic carcinoma but not for thymoma in stage II and III thymic epithelial tumors: the Japanese Association for Research on the Thymus Database StudyCancer201512171008101625565590
- PatelSMacdonaldOKNagdaSBittnerNSuntharalingamMEvaluation of the role of radiation therapy in the management of malignant thymomaInt J Radiat Oncol Biol Phys20128251797180121596484
- SakaiMOnukiTInagakiMEarly-stage thymic carcinoma: is adjuvant therapy required?J Thorac Dis20135216116423585943
- KondoKMondenYLymphogenous and hematogenous metastasis of thymic epithelial tumorsAnn Thorac Surg20037661859186414667600
- LeeCYBaeMKParkIKKimDJLeeJGChungKYEarly Masaoka stage and complete resection is important for prognosis of thymic carcinoma: a 20-year experience at a single institutionEur J Cardiothorac Surg200936115916219324568
- WekslerBDhuparRParikhVNasonKSPennathurAFersonPFThymic carcinoma: a multivariate analysis of factors predictive of survival in 290 patientsAnn Thorac Surg201395129930323141529
- FilossoPLGuerreraFRendinaAEOutcome of surgically resected thymic carcinoma: a multicenter experienceLung Cancer201483220521024370198
- OkerekeICKeslerKAFreemanRKThymic carcinoma: outcomes after surgical resectionAnn Thorac Surg20129351668167222421590
- SunYLiuJYuXTreatment and prognosis of Masaoka stage 3 thymic carcinoma: a retrospective study of 32 casesOnco Targets Ther2015869970225897244
