Dear editor
Lung cancer is the most commonly diagnosed cancer and the leading cause of cancer death worldwide,Citation1 with the majority of patients presenting with advanced disease.Citation2 Treg cells diminish the activation and function of lymphocytes via cell-cell contact and secretion of soluble mediators.Citation3 PD-1 is expressed on the surface of activated T and B cells and regulates their activation and proliferation.Citation4 PD-L1 binds to the PD-1 receptor, leading to, among other responses, negative regulation of immune activity. Both Tregs and the PD-1/PD-L1 pathway play important roles in lung cancer pathogenesis;Citation5,Citation6 however, the association between these two factors remains poorly understood. Here, we examined PD-1 expression on Tregs, and compared these results with established clinical indicators of lung cancer. These analyses revealed significant expression of PD-1 on Tregs in lung cancer, which may be used to inform clinical diagnoses.
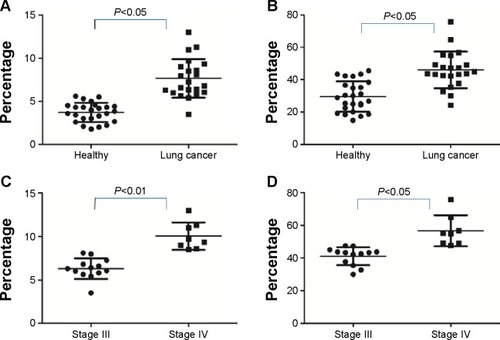
PD-1 expression was studied on CD4+CD25+CD127low Tregs isolated from peripheral blood mononuclear cells by flow cytometry. Twenty-two primary lung cancer patients and 25 healthy volunteers were recruited from the Second Affiliated Hospital of Soochow University (Suzhou, People’s Republic of China). Lung cancer patients had a nearly 2-fold increase in the number of circulating Tregs relative to healthy controls (7.66%±2.25% versus [vs] 3.76%±1.06%, respectively; P<0.05). The levels of PD-1 expression by CD4+CD25+CD127low Tregs were also higher in lung cancer samples compared to controls (46.01%±11.33% vs 33.34%±13.54%, respectively). Significant differences in both CD4+CD25+CD127low Treg abundance (6.29%±1.18% vs 10.06%±1.58%; P<0.01) and Treg PD-1 expression (41.85%±6.1% vs 56.57%±12.52%; P<0.05) were observed between clinical stages III and IV, respectively (); no differences were seen among other pathologic subtypes, or in terms of lymphatic metastasis.
Figure 1 Expression of Tregs PD-1 on Tregs in peripheral blood.
Tregs play a critical role in a variety of immunologic processes, including self-tolerance, anti-tumor immune responses, and transplantation.Citation7,Citation8 Our study revealed a significant increase in the number of CD4+CD25+CD127low Tregs in patients with lung cancer, relative to healthy controls. While the mechanisms underlying the increase in lung cancer-associated Tregs are not known, the overall increase in the number of immunosuppressive immune cells present in these patients may play an important role in both the development and progression of lung cancer.Citation9,Citation10
Costimulatory molecule receptors interacting with their corresponding ligand mediate both positive and negative costimulatory signals, which regulate immune cell activation, including the activation and proliferation of T cells, cytokine production, apoptosis, cell survival, and cytotoxicity.Citation11–Citation13 PD-1 belongs to the CD28 family of receptors, and is expressed on activated T, B, and myeloid cells.Citation4 PD-1 and its ligand PD-L1 deliver inhibitory signals that regulate the balance between effector T cell activation and immune-mediated tissue damage.Citation11,Citation12 In addition, the proliferation and immune inhibitory activity of Tregs is directly related to the expression of costimulatory molecules on the cell surface.Citation14 Conflicting reports on the role of PD-1 on Treg function have suggested that PD-1–PD-L1 ligation on Tregs promotes Treg stability and expansion,Citation15–Citation18 while others have suggested that this pathway inhibits Treg expansion and function.Citation19,Citation20 Our study revealed a distinct increase in Treg number and Treg PD-1 expression in patients with lung cancer, suggesting that the PD-1/PD-L1 pathway may play a role in Treg induction and is associated with impaired adaptive immunity. From these results, we hypothesize that the over-expression of PD-1 on Tregs and/or the increase in Treg number may participate in the immune inhibitory state of lung cancer patients. The cross-talk between Treg cells and PD-1/PD-L1-induced inhibition in lung cancer warrants further exploration for lung cancer associated immune pathogenesis.
Authors’ contributions
Both Anyuan Zhong and Xue Pan contributed equally to this letter. This letter has been approved by all authors for publication. All authors contributed toward data analysis, drafting, and revising the letter.
Acknowledgments
Our studies were supported by grants from the Natural Science Foundation of China (no 81272610).
Disclosure
The authors have no conflicts of interest to declare.
References
- SiegelRNaishadhamDJemalACancer statistics, 2013CA Cancer J Clin2013631113023335087
- SiegelRDeSantisCVirgoKCancer treatment and survivorship statistics, 2012CA Cancer J Clin201262422024122700443
- SakaguchiSNaturally arising Foxp3-expressing CD25+CD4+ regulatory T cells in immunological tolerance to self and non-selfNat Immunol20056434535215785760
- AgataYKawasakiANishimuraHExpression of the PD-1 antigen on the surface of stimulated mouse T and B lymphocytesInt Immunol1996857657728671665
- PircherAGamerithGAmannANeoadjuvant chemo-immunotherapy modifies CD4(+)CD25(+) regulatory T cells (Treg) in non-small cell lung cancer (NSCLC) patientsLung Cancer2014851818724780112
- ReckMPaz-AresLImmunologic Checkpoint Blockade in Lung CancerSemin Oncol201542340241725965358
- SakaguchiSRegulatory T cells: key controllers of immunologic self-toleranceCell2000101545545810850488
- MorseMClayTMMoscaPLyerlyHKImmunoregulatory T cells in cancer immunotherapyExpert Opin Biol Ther20022882783412517262
- ZhangDChenZWangDCWangXRegulatory T cells and potential inmmunotherapeutic targets in lung cancerCancer Metastasis Rev Epub2015512
- Domagala-KulawikJThe role of the immune system in non-small cell lung carcinoma and potential for therapeutic interventionTransl Lung Cancer Res20154217719025870800
- SharpeAHWherryEJAhmedRFreemanGJThe function of programmed cell death 1 and its ligands in regulating autoimmunity and infectionNat Immunol20078323924517304234
- KeirMEFranciscoLMSharpeAHPD-1 and its ligands in T-cell immunityCurr Opin Immunol200719330931417433872
- DayCLKaufmannDEKiepielaPPD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progressionNature2006443710935035416921384
- KitazawaYFujinoMWangQInvolvement of the programmed death-1/programmed death-1 ligand pathway in CD4+CD25+ regulatory T-cell activity to suppress alloimmune responsesTransplantation200783677478217414712
- FranciscoLMSalinasVHBrownKEPD-L1 regulates the development, maintenance, and function of induced regulatory T cellsJ Exp Med2009206133015302920008522
- PeriasamySDhimanRBarnesPFProgrammed death 1 and cytokine inducible SH2-containing protein dependent expansion of regulatory T cells upon stimulation With Mycobacterium tuberculosisJ Infect Dis201120391256126321383382
- ZhouQMungerMEHighfillSLProgram death-1 signaling and regulatory T cells collaborate to resist the function of adoptively transferred cytotoxic T lymphocytes in advanced acute myeloid leukemiaBlood2010116142484249320570856
- WangHYLeeDAPengGTumor-specific human CD4+ regulatory T cells and their ligands: implications for immunotherapyImmunity200420110711814738769
- FranceschiniDParoliMFrancavillaVPD-L1 negatively regulates CD4+CD25+Foxp3+ Tregs by limiting STAT-5 phospho-rylation in patients chronically infected with HCVJ Clin Invest2009119355156419229109
- KarimRJordanovaESPiersmaSJTumor-expressed B7-H1 and B7-DC in relation to PD-1+ T-cell infiltration and survival of patients with cervical carcinomaClin Cancer Res200915206341634719825956
