Abstract
Aim
To explore the function of peer support from the perspective of adults with type 1 diabetes in Denmark.
Methods
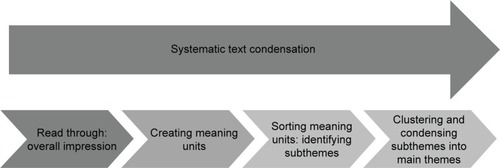
The study population consisted of 20 adults with type 1 diabetes. The sample was diverse in relation to educational background, age, sex, and cohabitation status. Inspired by action research, several methods and perspectives on peer support were explored and tested. Workshops and group and individual interviews were performed. Systematic text condensation was used to analyze data, supplemented with theory-based interpretive analysis.
Results
Adults with type 1 diabetes found peer support highly relevant to reduce a burdensome feeling of diabetes-specific loneliness. Peer support showed potential to create diabetes-specific social capital not only by creating reciprocal social support between peers but also, more importantly, by creating space for genuine trust and a feeling of communality. There was a widespread feeling of the pervasive impact of diabetes on daily life and thus the relevance of discussing all aspects of life. However, participants perceived peer support as particularly relevant in relation to big changes in life, for example, in family life, at work, or through treatment events such as getting an insulin pump.
Conclusion
Peer support programs focusing on creating and establishing diabetes-specific social capital using participatory approaches seem highly relevant among adults with type 1 diabetes. Content, methods, and effects of peer support need further exploration in collaboration with adults with type 1 diabetes.
Introduction
Managing their disease is a constant task for people with type 1 diabetes, and most daily management occurs without the involvement of health care professionals. People with type 1 diabetes often experience psychosocial problems such as anxiety and diabetes distress,Citation1,Citation2 and previous studies have indicated that lack of social support is associated with lower psychological well-being, as well as difficulties in managing diabetes and poorer glycemic control, in people with type 1 diabetes.Citation3,Citation4
The link between a lack of social support and poor physical and mental health is well established.Citation5,Citation6 Positive social support includes emotional, instrumental, and informational support and influences health and well-being through a variety of pathways, for example, by improving health behaviors, enhancing self-esteem with regard to performing self-care activities, and reducing distress.Citation7 Previous research has shown that high diabetes-specific social support is particularly associated with lower diabetes distress.Citation8 However, knowledge is lacking about methods and interventions to enhance diabetes-specific social support among adults with type 1 diabetes.
A promising way to enhance diabetes-specific social support is through peer support; studies among adults with diabetes have found peer support to be an effective method to provide emotional support for ongoing self-management.Citation9–Citation12 However, most studies focus on type 2 diabetes, and little is known about peer support among adults with type 1 diabetes.Citation13
Peer support in health care is defined as a method to create and strengthen social relationships, thereby improving and maintaining good health and well-being.Citation9,Citation14 The key functions of peer support have been identified by Peers for Progress – a program dedicated to promote evidence-based peer support as a key part of health care and prevention.Citation15 The key functions are, 1) assistance in daily management, 2) social and emotional support, 3) linkage to clinical care and community resources, and 4) ongoing support of chronic disease management.Citation16 Peer support creates a unique opportunity to reflect on daily life through sharing experiential knowledge.Citation9,Citation14,Citation17 However, the literature on diabetes-specific peer support currently addresses a wide range of peer interactions and interventions,Citation17 and the evidence is insufficient to determine which types of peer interactions, elements, and interventions are most applicable to and effective in type 1 diabetes. Furthermore, a 2013 review of diabetes-specific peer support literature revealed a tendency to confound diabetes-specific peer support with educational or self-management programs building on health professionals’ understanding of support.Citation17 Similarly, a frequent argument for the provision of diabetes-specific peer support is the growing number of people who need support and health care resources.Citation13,Citation18 This argument emphasizes peer support in lieu of professional care and does not stress the qualities of peer support as promoting and strengthening reciprocal social support between peers.
Although studies of diabetes-specific peer support generally focus on interactions between and support among people with diabetes, little is known about how members of the target group experience peer support. The aim of this study was to explore the function of peer support from the perspective of adults with type 1 diabetes in Denmark.
Methods
Study population
Twenty adults with type 1 diabetes participated in the study. Using convenience sampling, eleven adults were recruited from a specialized diabetes clinic in greater Copenhagen, Denmark, and nine adults were recruited from four different specialist diabetes clinics in the Central Region of Denmark. Participants were recruited through mailed invitations to individuals participating in a related study and notices on Danish Internet forums for people with type 1 diabetes posted by a study participant (Tine Filges, co-author). All adults with type 1 diabetes were eligible for participation, but the specific participants were selected to ensure a diverse sample in relation to educational background, age, sex, and cohabitation status ().
Table 1 Participant characteristics
Data collection
We collected data on participants’ perspectives on peer support during workshops and interviews. Inspired by action research,Citation19 we explored the function of peer support by evaluating different peer support methods at the workshops (). For example, we evaluated dialogue tools in the peer groups. Different probes were also used to prompt immediate reflection on peer support among participants, for example, presenting peer support scenario cartoons. Group discussions and individual interviews were guided by facilitating questions related to the specific aims and tools used in the workshops (). The investigation of participants’ view on peer support included exploring relevant topics to discuss with peers, the purpose of peer support, preferred characteristics of peer supporters, and preferred format of peer support. Workshops lasted 2.5 hours.
Table 2 Types of data generated in workshops and individual interviews
One workshop (nine participants) was held in the Central Region of Denmark. The group of eleven adults with type 1 diabetes recruited from Steno Diabetes Center, the specialized diabetes clinic in greater Copenhagen, participated in five workshops between January and November 2013. The number of workshops in which participants took part varied from five (three participants) to one (one participant). To ensure that all participants’ views were incorporated into the data, we conducted individual interviews with participants who did not participate in all workshops; interviews lasted ~1 hour. Data consisted of field notes, minutes, and transcribed group discussions from all six workshops, notes and completed exercises from workshop participants, and transcriptions from six individual interviews.
One researcher facilitated each workshop, and two or three researchers observed small group workshop and plenary sessions. One participant (Tine Filges, co-author) who was competent at research participated in workshop planning and facilitated selected exercises. Written informed consent was obtained from all participants. The study was approved by the Danish Data Protection Agency.
Qualitative analyses
Data were analyzed by systematic text condensation.Citation20 Initially, we read all data to obtain a general impression of important preliminary themes. All written text was then divided into units of meaning, and related units were sorted into groups representing subthemes. A final step was to cluster related subthemes to structure data into main themes.Citation20 While clustering subthemes into main themes, we used the constructs of social capital and loneliness as an interpretative framework.Citation21,Citation22 The choice of these constructs was not predetermined but emerged from the empirical subthemes. depicts the analytic approach.
Analyses were performed by the first and last authors, both of whom were present during all workshops. To ensure transparency and validity, the subthemes were presented to workshop participants; their comments and perspectives were incorporated into the analysis. Researchers involved in the workshops also commented on the subthemes.
Results
Diabetes-specific loneliness
Among participants, a widespread feeling existed that diabetes was pervasive throughout all aspects of life, and it was thus relevant to discuss diabetes with peers in relation to all aspects of life with type 1 diabetes. In general, participants’ descriptions of the function of peer support were connected to a feeling of loneliness related to their diabetes. Participants pointed out their experiences of dissatisfaction with social relations with regard to diabetes that included, 1) being on one’s own, 2) lack of connectedness and communality, and 3) lack of feeling understood ().
Table 3 Main themes based on empirical findings
Being on one’s own
Participants expressed that they felt “on their own” not only in relation to specific situations, such as travel planning, but also in general in daily life with diabetes, for example, “having no one to talk to” (male, age 35 years) and “having to make your own experiments on how to live well with diabetes” (male, age 46 years). Participants described how questions, feelings, and uncertainties arise in daily life with diabetes; they felt they had to handle most things by themselves. A woman diagnosed in adulthood expressed the feeling of being on her own:
No matter how good and well-meaning a health care professional is, it is in your everyday life that you face these problems, or challenges I would rather call them, and it is actually here that you need someone to talk to about your day and other things. So, I have to deal with all my thoughts and feelings on my own. Of course I can share these things with my friends and family, but they can … they can only listen, not engage in a dialogue. [Female, age 48 years]
Another woman from the Central Region of Denmark stated:
I don’t have anyone in my everyday life … I have a thing with counting carbohydrates – it would be amazing to come into contact with someone and ask them about how do you do it? and does it have any benefits for you? … and so on. [Age 56 years]
Feeling on one’s own also included the feeling of not having enough time with health care professionals.
Lack of connectedness and communality
Participants described feeling “excluded from society”, “different than the rest”, and “worth less than others”. One woman expressed the feeling of “being second-rate” and “being shoved out of the community” in relation to employment: “When there’s an economic crisis like we have now, with lots of people unemployed, then having diabetes is a disadvantage, it becomes a kind of sorting mechanism” (age 60 years). She did not inform employers about her diabetes when applying for a new job. In a similar vein, other participants described feeling uncomfortable with others knowing about their diabetes. One woman expressed feeling that society requires people with type 1 diabetes to deal with diabetes in such a way that they do not become a burden. A related comment from another participant described feeling that health care professionals judged her as a number:
… when you consult the professional you have 15 minutes and it … you are just a social security number … and the lower your average blood sugar level is the better. It’s even fine if your blood sugar is a little low at times. That will lower the average [of the clinic’s overall population] slightly. It doesn’t matter that you are shaking a bit, it’s good for your Hba1c! [Female, age 35 years]
Other participants expressed feeling less worthy. A 35-year-old man stated: “I don’t think there are any girls who should content themselves with me. I feel like I am a sickness and a burden to people”.
Lack of feeling understood
Participants spoke frequently of experiences of lack of understanding from friends, family, health professionals, and society. A participant expressed the lack of understanding by society very explicitly:
If there was more recognition in our society, that there is also a lot going on in your head when you get the disease, it would be easier to talk about. I mean, the majority of people seem to be of the opinion that as long as you get your injections you’ll be fine … but it’s not quite like that. [Male, age 35 years]
Several participants felt that “friends and family can only listen” to their experiences of living with diabetes but cannot “really understand”. Participants lacked what they called “a real dialogue about diabetes” with family, friends, and colleagues. Participants also stated that they found it difficult or impossible to have a real dialogue about daily life with diabetes and to feel understood by health care professionals, even though the latter had relevant and important clinical knowledge. However, participants also stated that health care professionals often grasped problems during consultations.
Diabetes-specific social capital
Participants’ views of relevant peer support could be interpreted as a need for diabetes-specific social capital. The need for diabetes-specific social capital included perceptions of the importance of peer support and its ability to create experience sharing, cohesion and collectiveness, trust and confidence, and reciprocity and social participation related to life with type 1 diabetes ().
Experience sharing
Participants were very clear in distinguishing between experiences and knowledge when they talked about their need for peer support. As an example, one participant stated:
We don’t like the word “expert” [in relation to peer support]. We talk about experience. We are not experts – we are experienced. One’s expertise from living with diabetes cannot necessarily be applied to another person with type 1 diabetes. We live different lives. You cannot do that. [Male, age 57 years]
Participants did not want advice from peers based on general or “medical knowledge” of type 1 diabetes; they preferred to have the opportunity to reflect on their own lives in the light of other’s experiences. A 39-year-old woman pointed out that real-life experiences of others can be “the missing link” between knowledge obtained from physicians and how it can be used in their own lives.
Participant preferences for experience sharing included general and more specific topics. More general topics included worries and concerns about living with diabetes and those related to family and work. More specific topics included food, hypoglycemia, travel, sports/exercise, relationship with the doctor/nurse, use of social services, insulin pumps, etc. Participants emphasized that peer support is particularly relevant in relation to big “changes in life”, for example, in family or work situations or events such as getting an insulin pump.
Cohesion and collectiveness
Participants frequently expressed that peer support can create a “safe place” arising from just being among others with type 1 diabetes. A 46-year-old man expressed this feeling in a group discussion: “Just the fact that she [another participant] is measuring her blood sugar right now as we speak. That is so cool. And you’re thinking, wow, you have diabetes, too!” Others expressed similar feelings, such as “being on the same wavelength” and “having a mutual understanding”. As a participant stated during an interview:
Diabetes and what it does to you doesn’t have its own language. We don’t have words to define what it feels like when you have low blood sugar. When you talk to others [referring to people who do not have diabetes] you need something to compare with, to try and explain how it is, and it’s nice sometimes not having to do that. [Female, age 42 years]
Another participant, who had never met another person with type 1 diabetes before, experienced this:
To have the chance to talk about these worries, just to say them out loud and then to someone who knows exactly how it is. I experienced this the first time I was here. Me and B …. [another participant], we didn’t need to explain much, with just a few words, we knew what we were talking about. We had this mutual understanding and having that experience gave me a lot. I thought … well … I am not alone in the world. There are others like me. [Female, age 48 years]
Several participants expressed feeling that sharing experiences with peers helped them to view the state of having diabetes as normal and created a feeling of collectiveness that they did not experience in daily life. Being similar to and understood by other participants provided support. In the words of one participant, newly diagnosed with type 1, who felt that nobody truly understood her situation: “these workshops have saved my life” (female, age 36 years).
Trust and confidence
In group discussions about preferred types of peer support, participants often used words such as “trust”, “confidence”, and “presence”. A 56-year-old woman pointed out the necessity for a basic feeling of trust and safety among participants in a peer support program in order to address difficult topics. Another woman elaborated:
I think that sharing experiences related to more concrete things are important and maybe that is the easiest part. The more uncomfortable thoughts and questions about situations in everyday life which we confront are, perhaps, better left out until a greater level of trust is established. [Female, age 62 years]
In contrast, other participants felt that confidence naturally arose from being among others with type 1 diabetes. A 46-year-old man referred to a conversation with a woman from the workshop:
That kind of confidence you feel when you are among other people with diabetes … I feel like I’ve spent many years trying to find out who I am – “diabetes-wise” and otherwise. I think that I’ve made a lot of progress. But at the same time there is still a lot of questions and concerns which crop up all the time. It felt safe to talk about it with her (another peer).
Reciprocity and social participation
Participants repeatedly emphasized that a natural reciprocity exists in relationships between people with type 1 diabetes and that peer support should focus on enhancing this reciprocity in the form of peer-to-peer partnerships or a group of peers in which everyone shares experiences and has the chance to reflect on their own lives with diabetes. However, participants also stated that in specific situations, such as being newly diagnosed, a mentoring relationship might be more appropriate. Participants had different perspectives about how to match peers. Some participants argued that differences in sex, age, and diabetes duration would be a barrier to reciprocity; others believed that differences would enhance the perspective on one’s own life with diabetes and the possibilities for reflexivity. The workshops, for which participants were selected so as to include differences in sex, occupation, age, and diabetes duration, showed that they in fact benefited from experience sharing and mutual understanding, despite these differences. Data also showed participants’ strong interest in social participation related to diabetes; they expressed interest in providing social support to others with type 1 diabetes as well as receiving support from peers. Furthermore, they showed a genuine interest in helping each other and in widening the scope of support for people with type 1 diabetes in general.
Discussion
To the best of our knowledge, ours is the first study to explore patient perspectives on the function of peer support in adult type 1 diabetes. The need for peer support arose from a feeling of diabetes-specific loneliness that was shared across differences in sex, age, diabetes duration, employment status, and marital status, and relevant peer support can create diabetes-specific social capital. The concept of diabetes-specific social capital was identified in this study; it emphasizes both the collective importance of experience sharing between people with type 1 diabetes and the broader need for communality related to type 1 diabetes. Furthermore, diabetes-specific social capital highlights the fact that social participation – being able to share experiences, support, and being with people with the same condition – is just as important as receiving support. Other studies in diabetes have indicated greater benefits to self-care activities from providing social support to peers than receiving support from them.Citation23
The concepts of loneliness and social capital were identified through our empirical findings and served as a theoretical framework in the analyses. Others have identified that loneliness relates to specific types of social relationships, for example, research among adolescents has differentiated between peer-related loneliness and family-related loneliness.Citation24 To the best of our knowledge, no previous study has explored loneliness specifically related to diabetes. However, the well-known Problem Areas in Diabetes survey incorporates one item regarding “feeling alone with diabetes”.Citation25 Our findings concerning lack of communality correspond with those of a global diabetes study (DAWN2), in which approximately one-fifth of people with diabetes felt they had been discriminated against because of their disease.Citation26 Generally, feelings such as reciprocity, belonging, participation, high social support, and feelings of solidarity are traits of communities with high social capital.Citation21,Citation27,Citation28 Sense of belonging is an important factor in health promotion, and studies of social capital have found that low social capital is related to both lower quality of life and higher morbidity.Citation29–Citation31 The influence of social capital has also been explored in people with diabetes but not social capital created between people with diabetes specifically. With this broader perspective, for example, trust and solidarity in the local neighborhood have been found to be associated with good glycemic control.Citation32,Citation33 Further research should explore whether enhancing diabetes-specific social capital can improve psychosocial and physical outcomes in people with type 1 diabetes.
From the perspective of participants, peer support is unique and in contrast to the type of diabetes peer programs that build on health professionals’ understanding of support and focus on peer education.Citation10,Citation13,Citation17,Citation18 Our findings emphasize that adults with type 1 diabetes perceive the primary role of peer support as creating social networks of people who understand their mutual situation in a way that other social networks do not. Health care professionals cannot create or provide diabetes-specific social capital – and peer support cannot substitute for support from health care professionals. However, our findings confirm our initial description of the aim of peer support in chronic illness.Citation14
Our findings also highlight the fact that few studies have focused on peer support targeting people with type 1 diabetes, although it seemed to be very much needed. Some participants had never met another person with type 1 diabetes; having the opportunity to do so was very meaningful to them. Our findings included differing perspectives on how to best match peers to provide mutual support. Although some participants stated that peers needed to have similar characteristics, the workshops indicated that the possibility of enhancing diabetes-specific social capital existed within the group despite large differences between participants. Further research is needed in relation to what combination of participant characteristics in peer support best creates diabetes-specific social capital.
Strengths of our study include continuous analyses during data collection, allowing reflection and validation among participants and co-researchers. The inclusion of different settings is also a strength.Citation34 The data across settings were very similar; participants in the two groups even used similar wording, such as the request for “real dialogue” and “support in life transitions”. They also articulated “sterile answers” from professionals and “real-life experiences” in both settings. The comparison of the two settings indicated that data saturation was reached.
The use of group discussions and participatory methods revealed dimensions of understanding that might have remained untapped in more conventional data collection techniques.Citation35,Citation36 For example, testing different peer support methods enabled reactions to concrete peer relations and revealed unmet and, for some participants, unknown needs. The use of various methods and a diverse sample is believed to increase the robustness of the results.Citation34
A limitation of our study is that participants might have chosen to participate in the study due to positive preferences for peer support. However, some participants were recruited based on earlier involvement in a study that was unrelated to peer support. Group discussions and interviews may have constrained participants from sharing views that diverged from the group consensus. We found a tendency toward more openness and in-depth descriptions of personal experiences with regard to feelings of diabetes-specific loneliness in individual interviews rather than in group interviews.Citation37
With the use of a theoretical framework and the diverse empirical data, the findings of this study seem relevant and highly likely to be transferable to other adults with type 1 diabetes in Denmark, as well as in similar countries. It is also likely that the feeling of diabetes loneliness and the need of diabetes-specific social capital are present among people with type 1 diabetes in other countries as well, as the findings of our studies are grounded in theoretical constructs and relate to existing literature as discussed earlier. However, potential differences, including cultural differences, in subgroups need to be explored. The study does not provide evidence about the prevalence of diabetes loneliness or the need for diabetes-specific social capital. Differences in prevalence of adults with type 1 diabetes in different subgroups need further exploration. Furthermore, research into effects of enhancing diabetes-specific social capital is needed, for example, in relation to the potential to decrease diabetes distress and improve self-management behaviors. Our study indicates a substantial need for peer support among adults with type 1 diabetes, focusing on the creation and strengthening of diabetes-specific social capital as a response to a shared feeling of diabetes-specific loneliness. Methods and settings for enhancing diabetes-specific social support through peer support need further exploration and testing in collaboration with people with type 1 diabetes.
Acknowledgments
We thank all the participants for their participation in workshops and individual interviews. LEJ and IW are employed by Steno Diabetes Center A/S, a research hospital working in the Danish National Health Service and owned by Novo Nordisk A/S. Steno Diabetes Center receives part of its core funding from unrestricted grants from the Novo Foundation and Novo Nordisk A/S.
Disclosure
The authors report no conflicts of interest in this work.
References
- JoensenLETapagerIWillaingIDiabetes distress in type 1 diabetes – a new measurement fit for purposeDiabet Med20133091132113923701311
- TriefPMSandbergJGDimmockJAForkenPJWeinstockRSPersonal and relationship challenges of adults with type 1 diabetes: a qualitative focus group studyDiabetes Care20133692483248823474590
- JoensenLEAlmdalTPWillaingIType 1 diabetes and living without a partner: psychological and social aspects, self-management behaviour, and glycaemic controlDiabetes Res Clin Pract2013101327828523891305
- LloydCEWingRROrchardTJBeckerDJPsychosocial correlates of glycemic control: the Pittsburgh epidemiology of diabetes complications (EDC) StudyDiabetes Res Clin Pract1993212–31871958269821
- KawachiIBerkmanLFSocial ties and mental healthJ Urban Health200178345846711564849
- KawachiISocial capital and healthBirdCConradPFremontAMTimmermansSHandbook of Medical Sociology6th edNashville, TNVanderbilt University Press20101832
- BerkmanLFGlassTBrissetteISeemanTEFrom social integration to health: Durkheim in the new millenniumSoc Sci Med200051684385710972429
- JoensenLEAlmdalTPWillaingIAssociations between patient characteristics, social relations, diabetes management, quality of life, glycaemic control and emotional burden in type 1 diabetesPrim Care Diabetes2016101415026163949
- HeislerMDifferent models to mobilize peer support to improve diabetes self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future researchFam Pract201027suppl 1i23i3219293400
- World Health OrganizationWorld Health Report: Peer Support Programs in DiabetesGenevaWHO2008
- van DamHAvan der HorstFGKnoopsLRyckmanRMCrebolderHFvan den BorneBHSocial support in diabetes: a systematic review of controlled intervention studiesPatient Educ Couns200559111216198213
- HarknessEMacdonaldWValderasJCoventryPGaskLBowerPIdentifying psychosocial interventions that improve both physical and mental health in patients with diabetes: a systematic review and meta-analysisDiabetes Care201033492693020351228
- DaleJRWilliamsSMBowyerVWhat is the effect of peer support on diabetes outcomes in adults? A systematic reviewDiabet Med201229111361137722804713
- DennisCLPeer support within a health care context: a concept analysisInt J Nurs Stud200340332133212605954
- Peers for Progress (homepage)University of North Carolina at Chapel Hill Available at http://peersforprogress.org/Accessed April 29, 2016
- FisherEBAyalaGXIbarraLPeers for Progress Investigator GroupContributions of peer support to health, health care, and prevention: papers from peers for progressAnn Fam Med201513suppl 1S2S826304968
- SimmonsDBunnCCohnSGraffyJWhat is the idea behind peer-to-peer support in diabetes?Diabetes Manage2013216170
- BrownsonCAHeislerMThe role of peer support in diabetes care and self-managementPatient20092151722273055
- MeyerJQualitative research in health care. Using qualitative methods in health related action researchBMJ2000320722817818110634744
- MalterudKSystematic text condensation: a strategy for qualitative analysisScand J Public Health201240879580523221918
- PutnamRDBowling Alone: The Collapse and Revival of American CommunityNew York, NYSimon & Schuster2000
- PeplauLLoneliness research: basic concepts and findingsSarasonISarasonBSocial Support: Theory, Research, and ApplicationsBostonMartinus Nijhoff Publishers1985269286
- HeislerMPietteJD“I help you, and you help me”: facilitated telephone peer support among patients with diabetesDiabetes Educ200531686987916288094
- LasgaardMGoossensLBramsenRHTrillingsgaardTElklitADifferent sources of loneliness are associated with different forms of psychopathology in adolescenceJ Res Pers2011452233237
- PolonskyWHAndersonBJLohrerPAAssessment of diabetes-related distressDiabetes Care19951867547607555499
- NicolucciAKovacs BurnsKHoltRIDAWN2 Study GroupDiabetes attitudes, wishes and needs second study (DAWN2): cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetesDiabet Med201330776777723711019
- NieminenTMartelinTKoskinenSAroHAlanenEHyyppaMTSocial capital as a determinant of self-rated health and psychological well-beingInt J Public Health201055653154220361226
- FerlanderSThe importance of different forms of social capital for healthActa Sociol2007502115128
- MurayamaHFujiwaraYKawachiISocial capital and health: a review of prospective multilevel studiesJ Epidemiol201222317918722447212
- KawachiIKennedyBPGlassRSocial capital and self-rated health: a contextual analysisAm J Public Health19998981187119310432904
- KawachiIKennedyBPLochnerKProthrow-StithDSocial capital, income inequality, and mortalityAm J Public Health1997879149114989314802
- LongJAFieldSArmstrongKChangVWMetlayJPSocial capital and glucose controlJ Community Health201035551952620143139
- FarajzadeganZJafariNNazerSKeyvanaraMZamaniASocial capital – a neglected issue in diabetes control: a cross-sectional survey in IranHealth Soc Care Community20132119810323057630
- PattonMQQualitative Research and Evaluation MethodsThousand Oaks, CASage Publications2002
- Lavie-AjayiM“I didn’t know I was isolated until I wasn’t isolated any more”: the use of groups in qualitative psychology researchQualitative Inquiry2014202175182
- KitzingerJQualitative research. Introducing focus groupsBMJ199531170002993027633241
- KvaleSInterviews – An Introduction to Qualitative Research InterviewingThousand Oaks, CASage Publications1996