Abstract
Introduction
Therapeutic shoes are prescribed to prevent diabetic foot ulcers, but adherence to wearing the shoes is often poor.
Aim
The aim of this study was to review the literature on factors that are associated with adherence to wearing therapeutic shoes and construct a model of adherence to aid future research and development in the field.
Methods
We conducted a systematic search in PubMed, CINAHL, and PsycINFO for quantitative studies on factors associated with adherence to wearing therapeutic shoes among people with diabetes.
Results
Six studies were included in the review. The studies focused mainly on patient-, therapy-, and condition-related adherence factors. There is some evidence (three to five studies) that sex, diabetes duration, and ulcer history are not associated with adherence. The evidence for or against the other factors was weak (only one or two studies) or conflicting.
Conclusion
There is no conclusive evidence for using any factor to predict adherence to wearing therapeutic shoes, but there is some evidence against using certain factors for predicting adherence. Future studies should include a broader range of factors, including health system and social/economic factors, and they should investigate perceived costs and benefits of wearing therapeutic shoes in comparison with other shoes or no shoes. A seesaw model is presented illustrating the complex phenomenon of adherence. Further research is needed to identify factors associated with adherence to wearing therapeutic shoes, to enable the development of interventions to improve adherence and thereby reduce ulceration rates among people with diabetic foot complications.
Introduction
Redistributing pressures under the diabetic foot is essential to prevent and heal plantar ulcers. However, several studies have reported that people with diabetes tend to wear their offloading devices, such as walkers, half-shoes, and therapeutic shoes, less than would be advisable.Citation1–Citation7 Therefore, guidelines recommend using nonremovable devices, such as total contact casts, to offload pressure on ulcers.Citation8,Citation9 However, it is not feasible to use nonremovable devices once the ulcer has healed and often therapeutic shoes are prescribed to prevent reulceration. High reulceration rates have been reported in the literatureCitation10–Citation12 and low adherence to wearing the therapeutic shoes might be one explanation.Citation2 Thus, there is a need to understand the reasons for the low adherence to wearing therapeutic shoes to be able to improve it and thereby reduce ulceration rates among people with diabetes.
The World Health Organization defines adherence as “the extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes – corresponds with agreed recommendations from a health care provider.”Citation13 This definition emphasizes the person’s agreement to the recommendations, in contrast to the older term compliance, which suggests obedience to expert advice. People cannot simply be expected to follow their treatment regimen (and blamed if they do not), as a number of factors will affect their behavior and capacity to adhere. Adherence is thus a multidimensional concept, proposed to consist of five interconnected dimensions: 1) patient-related factors; 2) therapy-related factors; 3) condition-related factors; 4) health system-related factors; and 5) social and economic factors.Citation13
When people are asked about their therapeutic shoes, common complaints and reasons for not wearing them are that the shoes are found to be unattractive, too big, uncomfortable, or difficult to walk in.Citation1,Citation14–Citation16 These reasons are well known to clinicians prescribing therapeutic shoes, but there might be other, less obvious, factors that influence an individual’s decision to wear or not wear therapeutic shoes. These factors might include perceived severity of the foot condition, sensory neuropathy, and beliefs about what causes foot ulcers. Such reasons are not always obvious to the person with the foot condition and would therefore not be mentioned in interviews. Thus, there is a need to complement qualitative studies and clinical experience with quantitative studies that can reveal other factors that influence adherence, and thereby get a broader picture of the complex phenomenon of adherence to wearing therapeutic shoes.
The aim of this study was to review and discuss the current quantitative literature on factors associated with adherence to wearing therapeutic shoes among people with diabetes and construct a model of adherence to support future research and development in the field.
Methods
We searched PubMed, CINAHL, and PsycINFO in June 2016 from their inception. The language was restricted to English. Search details are presented in . The abstracts of all articles were read by one of the authors (GJ) and both authors read the full text of the articles that were relevant for the purpose of this review. Studies were included only if they included a statistical investigation of factors associated with adherence to wearing therapeutic shoes among people with diabetes.
Table 1 Search methods and results
Results and reflections
The search yielded 46 unique articles. One of the authors (GJ) read the abstracts (or full text, if no abstract was available) and excluded 34 articles that did not fulfill the inclusion criterion. Both authors read the full text of the 12 remaining and potentially relevant articles and excluded six more articles that did not fulfill the inclusion criterion. Thus, six articles were included in the review (). The studies investigated adherence with regard to factors related to the patient’s perceptions, the condition, the therapy, the patient’s social and economic circumstances, and the health system, with the main focus on patient-, therapy-, and condition-related factors.
Table 2 Studies included in the review
Description of included studies
Arts et alCitation17 studied 153 people with peripheral neuropathy and a recently healed plantar foot ulcer, and investigated the association between self-reported adherence and demographic variables, perceptions of the shoes and other factors in a multiple regression analysis. Participants were considered adherent (“frequent users”) if they wore therapeutic shoes for at least 60% of daytime hours.
BreuerCitation18 interviewed people with peripheral neuropathy and a healed ulcer. Fifty-one of the 85 interviewees were considered adherent, defined as wearing therapeutic shoes on the day of interview, and 34 were considered nonadherent. Characteristics of the participants and answers on a questionnaire were compared between the adherent and nonadherent groups.
Chantelau and HaageCitation3 interviewed 51 people attending a diabetic foot clinic. Sex, ulcer history, and frequency of foot care were compared between the 37 interviewees classified as adherent (those who reported that they wore therapeutic shoes for >60% of daytime hours) and the 14 interviewees classified as nonadherent.
ChurchmanCitation19 sent a questionnaire to people who had had a foot ulcer within the past 2 years, and 20 of the respondents had been prescribed therapeutic shoes. The relation between sex and self-reported use of therapeutic shoes (days per week and hours per day) was investigated.
Macfarlane and JensenCitation20 surveyed people who had been provided with therapeutic shoes and investigated correlations between the 50 respondents’ self-reported adherence and age, diabetes duration, and perceptions of their foot condition and shoes.
Waaijman et alCitation5 investigated adherence in 107 people with therapeutic shoes, using a temperature monitor in the shoe and a step activity monitor strapped to the leg. The association between adherence and factors related to the person, condition, shoes, and social situation was investigated in a multiple regression analysis.
The results are summarized in and the main findings are discussed further according to the five adherence dimensions proposed by the World Health Organization.Citation13 Many factors were investigated in only one study and most associations were nonsignificant.
Table 3 Summary of results of the included studies: associations with adherence to wearing therapeutic shoes
Patient-related factors
Sex differences in attitudes toward therapeutic shoes have been reported in the literature, with women being less satisfied than men with the choices of shoe style and color.Citation1 From this, it would be expected that women wear their therapeutic shoes to a lesser degree than men do. This was investigated in five studies,Citation3,Citation5,Citation17–Citation19 but no association between sex and adherence was found. Age has previously been found to be associated with adherence to physical activity and diet in people with diabetes.Citation13 Four studiesCitation5,Citation17,Citation18,Citation20 investigated the association between adherence to wearing therapeutic shoes and age, of which one studyCitation18 found an association: the nonadherent group was younger than the adherent group.
Two studiesCitation18,Citation20 investigated the association between adherence and perceived severity of the foot condition, but only oneCitation18 found a positive association. Surprisingly, and counterintuitively, BreuerCitation18 found that the proportion of people who expected ulcer recurrences whatever they did was higher in the adherent group than in the nonadherent group.
An association could be expected between the value the person puts on the shoes and adherence, but the results were conflicting: one studyCitation18 found that the proportion of interviewees who would have therapeutic shoes rather than clothing, TV, or traveling was higher in the adherent group, whereas another studyCitation17 found no association between overall appreciation of the shoes and adherence. It has been hypothesized that perceived benefits are important for an individual’s decision to use therapeutic shoes and other assistive devices.Citation21,Citation22 One studyCitation17 found an association between perceived benefit of therapeutic shoes and adherence (although not significant in the case of benefit in the workplace, which might be attributed to the fact that few of the participants were working). Macfarlane and JensenCitation20 found that respondents who believe that wearing therapeutic shoes is important to prevent complications also wear them to a higher degree. Interestingly, the latter study did not find any association between adherence and the more general belief that therapeutic shoes are important. It might be the case that adherence is determined by an individual’s personal beliefs about his or her own feet and shoes, rather than by general beliefs about foot disease and therapeutic shoes. To the best of our knowledge, the study by Macfarlane and JensenCitation20 is the only one that has investigated whether the person’s belief in the main aim of prescribing therapeutic shoes, that is, reducing ulceration risks, influences adherence. Risk perception is an interesting aspect, given that many people with diabetes are not aware that they have sensory neuropathyCitation23 or do not consider it to be a risk factor for foot ulcers.Citation14 In the study by Macfarlane and Jensen,Citation20 most respondents felt that their foot condition was better than that of most other people with diabetes, even though 62% had a history of foot complications. Further studies are needed on how to educate and inform patients about risks and risk management. These risk education programs should observe that some people with foot ulcers may have cognitive difficultiesCitation24 and therefore need adapted teaching. An interesting avenue for patient education is the development of activity monitors and temperature sensors to measure adherence and provide feedback to patients.Citation25
Therapy-related factors
Attributes of the therapeutic shoes, such as appearance, comfort, and weight, are common sources of complaints and could therefore be expected to influence adherence.Citation20 Three studiesCitation5,Citation17,Citation18 considered shoe appearance, and one of themCitation5 found an association with adherence. Two studiesCitation5,Citation17 investigated other shoe attributes, such as shoe type and comfort, and found no association with adherence. The reason might be that the individuals and shoe types used are too heterogeneous to find common patterns.
Condition-related factors
People with diabetic foot complications often suffer from significant comorbidityCitation26 and thus undergo several simultaneous health treatments. Five studiesCitation3,Citation5,Citation17,Citation18,Citation20 investigated whether health conditions (including diabetes and related complications) and treatments influence adherence: diabetes duration consistently showed no association with adherence,Citation5,Citation17,Citation18,Citation20 while diabetes type was associated with adherence in oneCitation18 of three studies.Citation5,Citation17,Citation18 Four studiesCitation3,Citation5,Citation17,Citation18 investigated whether foot status influenced adherence: ulcer history consistently showed no association with adherence,Citation3,Citation5,Citation18 while the results were conflicting regarding the presence of minor amputationCitation5,Citation17,Citation18 and severity of foot deformity (including minor amputations).Citation5,Citation17 Only one studyCitation5 investigated the history of major amputation and found no association with adherence. OneCitation5 of two studiesCitation5,Citation17 investigating body mass index found a negative association with adherence.
Some authorsCitation27,Citation28 have hypothesized that sensory neuropathy reduces adherence to wearing offloading devices. The rationale is that pain is an important motivator for an individual to offload pressure on an ulcer, and with sensory neuropathy this motivator is diminished or absent. Neither Arts et alCitation17 nor BreuerCitation18 found any association between sensory neuropathy and adherence, but as the participants did not have ulcers at the time of the study and were not asked specifically about pain, it is not possible to corroborate or refute the hypothesis from these results. There are currently no studies on people without active ulcers investigating pain as a direct motivator for adherence, that is, the difference in pain between when wearing therapeutic and other shoes (or no shoes).
Health system-related factors
One studyCitation18 investigated the association between adherence and the extent to which interviewees felt sufficiently informed about the foot disease, but found no association. Some authors have hypothesized that the payment structures for therapeutic shoes might influence adherence. SoorikumaranCitation29 hypothesized that people would wear the shoes more if they had to pay a fee for them, in accordance with the sunk-cost effect, which is manifested in a greater tendency to continue an endeavor (in this case, wearing therapeutic shoes) once an investment has been made.Citation30,Citation31 On the other hand, a fee might be an obstacle for some people to obtain therapeutic shoes at all.Citation14 To the authors’ knowledge, the hypothesis about the impact of fees on adherence to wearing therapeutic shoes has not been studied empirically. Neither has any study investigated the effects of presumably important health system-related factors, such as the reimbursement system, frequency of follow-up, continuity of care, and communication style of the shoe provider.
Social and economic factors
Three studiesCitation5,Citation17,Citation18 investigated different social factors and found no impact on adherence from living alone,Citation5,Citation18 employment,Citation5,Citation18 or education level.Citation5,Citation17 None of the studies investigated whether social support influences adherence.
The scarcity of studies investigating social and economic factors is surprising, given the impact of social context on fashion and clothing. In rural areas in developing countries, it is common to walk barefoot outside, even among people with diabetes,Citation32,Citation33 and there are large variations across countries in the extent and type of shoes that are worn indoors. Some professions demand that employees wear protective shoes or shoes with a certain appearance, and therapeutic shoes might reveal the individual’s diabetes diagnosis to other people, which can be unwelcome.Citation22,Citation34 Thus, there is a need to include social, professional, and other environmental factors in future studies on adherence. Simply instructing people to wear their therapeutic shoes all the time without taking context into account is probably not a successful strategy. There is a need to “tailor the treatment to the patient’s lifestyle, not the other way around.”Citation35
Discussion
Studies to date have mostly focused on adherence to wearing therapeutic shoes in relation to the patient’s perceptions, therapy (eg, shoe comfort) and condition (diabetes and its complications), with little emphasis given to factors related to the patient’s social and economic circumstances or the health system. Many factors have only been investigated in a single study and most have turned out to be nonsignificant. There are too few studies to draw any firm conclusions at present, but there is some evidence (three to five studies) for not using sex, diabetes duration, or ulcer history as predictors of adherence. The evidence for or against the other factors is weak (only one or two studies) or conflicting.
It might seem counterintuitive that complaints that are common in qualitative studies and clinical practice, such as shoe appearance, in most cases are not associated with adherence. The reason might be that people give different weight to different factors. Some do not wear the shoes because they are unattractive, while others wear the shoes even though they are unattractive, because they perceive some other benefit of wearing them. The results of this review also contrast with studies on mixed samples of people with diabetes and other health conditions, where sex and opinions about shoe attributes have been associated with adherence levels.Citation36,Citation37 However, the results are difficult to compare with the current review, as shoes are prescribed for different reasons according to the diagnosis, for example, ulcer prevention for people with diabetes and pain relief for people with rheumatoid arthritis.
The results on objective and subjective foot status were mixed, with some studies supporting an association with adherence and some studies not. Knowles and BoultonCitation1 state that the person needs to be convinced of the severity of the foot condition and the benefit of wearing therapeutic shoes. We agree and pose the following hypothesis: adherence to wearing therapeutic shoes is positively influenced by the foot condition only if two prerequisites are fulfilled: 1) the person thinks that the foot condition is a problem (which might be more apparent with a minor amputation than with a healed ulcer); and 2) the person believes that wearing therapeutic shoes solves this problem better than wearing other shoes (or no shoes). Interestingly, two studiesCitation17,Citation20 found that the perceived benefit of wearing therapeutic shoes was associated with higher adherence. This is in line with a theory of adherence to using assistive technology, emphasizing the impact on adherence of perceived benefits of using the technology in comparison with other interventions.Citation21 Therefore, we suggest that future studies should ask people specifically about perceived costs and benefits of wearing therapeutic shoes in comparison with other shoes (or no shoes).
There are several limitations with the included studies and, therefore, we did not find it meaningful to grade the quality of the studies. All studies were observational cross-sectional studies, many studies had small samples of participants and the studies defined and measured adherence in different ways; these weaknesses made it more difficult to draw conclusions about the influence of various factors on adherence. Four of the studies only used univariate analysis, which makes the results more vulnerable to confounding. Finally, all studies were conducted in North America or Western Europe, limiting the generalizability of the results. Future studies should preferably be conducted in different cultural settings and use an experimental, longitudinal study design, and multivariate analysis to gain more robust evidence for causal mechanisms. A limitation of this review was that the search was restricted to publications in English. Hence, we cannot exclude the possibility that we might have missed some relevant studies, especially studies conducted outside North America and Western Europe.
In general, studies have not yet been very successful in finding predictors of adherence, which might have three possible explanations. First, researchers might have focused on the wrong factors and need to broaden the focus to include more factors related to the patient’s social and economic situation and the health system. Second, researchers might have used the wrong perspective, for example, focusing on perceptions of the therapeutic shoes per se instead of perceptions of the relative costs and benefits of wearing therapeutic shoes compared with other shoes (or no shoes).Citation21,Citation22 Third, researchers might have paid too little attention to the distinction between group and individual-level predictors of adherence. People with diabetic foot complications are a heterogeneous group and the reasons for choosing to wear or not wear therapeutic shoes might vary so strongly between individuals that predictors for adherence can only exist on the level of the individual or subgroup, and not on the level of the whole group. Regardless of whether there are group-level predictors that have yet to be found or whether such general predictors do not exist, there is a need for a deeper understanding of the multifaceted nature of adherence as phenomenon. A model to aid such understanding is presented in the following section.
A model of adherence to wearing therapeutic shoes
We constructed a seesaw model to illustrate how different factors impact a person’s or a group of people’s adherence to wearing therapeutic shoes (). The factors are represented by boxes, whose position on the seesaw represents the direction of impact (toward adherence or nonadherence) and the size of the boxes represents the relative weights of different factors. The net effect of the factors is illustrated by the tipping of the seesaw toward adherence or nonadherence. Importantly, the factors (boxes), their direction of influence (box position), and the weight given to them (box size) are all seen from the perspective of the person with the foot condition. For example, it is the perception of the extent that therapeutic shoes reduce ulceration risks that influences adherence, not whether the shoes objectively do reduce the risks.
Figure 1 A seesaw model illustrating how different factors affect adherence to wearing therapeutic shoes.
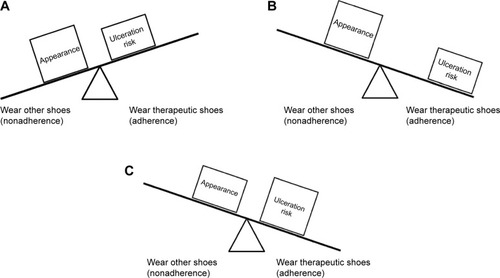
The model can be used to understand how, and in what way, perceptions influence adherence (or nonadherence) to wearing therapeutic shoes. Furthermore, the model can be used to highlight what actions can be taken to improve adherence. We can influence adherence (tipping of the seesaw) by changing the factors’ direction of influence (box positions), relative weights (box sizes), or a combination of the two. The lines of action are illustrated with a fictive case: a middle-aged man with a recently healed plantar ulcer. Note that the case is strongly simplified and only includes two factors to illustrate the use of the model. Although the man believes that wearing therapeutic shoes reduces the risk of ulceration compared with other shoes, he believes that the difference is small and this is outweighed by the fact that he finds his therapeutic shoes less attractive, a factor he gives more weight to. The net result is nonadherence (). The first option to improve his adherence would be to influence his perceptions of ulceration risks when wearing therapeutic and other shoes. Mueller et alCitation38 demonstrated how visualizations of plantar pressures can be used to educate people with sensory neuropathy about the offloading effect of therapeutic shoes because they no longer experience the sensation of pressure on the foot. If the person is convinced that wearing therapeutic shoes substantially reduces ulceration risks compared with other shoes, this will give a stronger motivation for adherence (). The second option to improve the man’s adherence would be to facilitate the process of adapting to wearing therapeutic shoes. A qualitative case study by Paton et alCitation39 illustrates the dynamic process of adherence, in which some individuals shift priorities over time, resulting in higher adherence. This process can be viewed as a shift from the everyday perspective of shoes as items of clothing (emphasizing appearance), to a professional’s perspective of shoes as medical devices (emphasizing ulcer prevention).Citation39 By understanding where an individual is in the process of adaptation, we might be able to facilitate the process and thereby improve adherence ().
Obviously, the model is a simplification of the real-life situation where a multitude of factors may interact and influence adherence. Nevertheless, the case illustrates that the model can highlight different lines of action that can be taken to improve adherence. Notably, the two examples of how to improve the man’s adherence do not include (but do not exclude) any improvement in the appearance of the shoes, although this was his self-reported reason for not wearing them.
Conclusion
There are too few studies to draw any definitive conclusions about factors associated with adherence to wearing therapeutic shoes. There is some evidence for not using sex, diabetes duration, or ulcer history as predictors of adherence. High-quality studies are needed, simultaneously investigating the impact on adherence of a broader range of factors, including those related to the health system and the patient’s social and economic situation. The framework of perceived costs and benefits of wearing therapeutic shoes compared with other shoes or no shoes is an interesting starting point for further inquiry. A model of adherence is proposed that can hopefully support further research and development in the field.
Acknowledgments
This study was supported by Region Örebro County, Sweden.
Disclosure
The authors report no conflicts of interest in this work.
References
- KnowlesEABoultonAJDo people with diabetes wear their prescribed footwear?Diabet Med19961312106410688973889
- BusSAWaaijmanRArtsMEffect of custom-made footwear on foot ulcer recurrence in diabetes: a multicenter randomized controlled trialDiabetes Care201336124109411624130357
- ChantelauEHaagePAn audit of cushioned diabetic footwear: relation to patient complianceDiabet Med19941111141168181241
- PatonJSRobertsABruceGKMarsdenJPatients’ experience of therapeutic footwear whilst living at risk of neuropathic diabetic foot ulceration: an interpretative phenomenological analysis (IPA)J Foot Ankle Res2014711624559125
- WaaijmanRKeukenkampRde HaartMPolomskiWPNolletFBusSAAdherence to wearing prescription custom-made footwear in patients with diabetes at high risk for plantar foot ulcerationDiabetes Care20133661613161823321218
- ArmstrongDGLaveryLAKimbrielHRNixonBPBoultonAJActivity patterns of patients with diabetic foot ulceration: patients with active ulceration may not adhere to a standard pressure off-loading regimenDiabetes Care20032692595259712941724
- McCabeCJStevensonRCDolanAMEvaluation of a diabetic foot screening and protection programmeDiabet Med199815180849472868
- BusSAArmstrongDGvan DeursenRWLewisJECaravaggiCFCavanaghPRIWGDF guidance on footwear and offloading interventions to prevent and heal foot ulcers in patients with diabetesDiabetes Metab Res Rev201632Suppl 1253626813614
- HingoraniALaMuragliaGMHenkePThe management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular MedicineJ Vasc Surg2016632 Suppl3S21S26804367
- ApelqvistJLarssonJAgardhCDLong-term prognosis for diabetic patients with foot ulcersJ Intern Med199323364854918501419
- PetersEJArmstrongDGLaveryLARisk factors for recurrent diabetic foot ulcers: site mattersDiabetes Care20073082077207917507693
- PoundNChipchaseSTreeceKGameFJeffcoateWUlcer-free survival following management of foot ulcers in diabetesDiabet Med200522101306130916176187
- SabatéEAdherence to Long-Term Therapies: Evidence for ActionGenevaWorld Health Organization2003
- van de WegBCompliance with orthopaedic footwear in patients with diabetesDiabetic Foot J2002513236
- BakerNLeatherdaleBAudit of special shoes: are they being worn?Diabetic Foot J199923100104
- PatonJSRobertsABruceGKMarsdenJDoes footwear affect balance? the views and experiences of people with diabetes and neuropathy who have fallenJ Am Podiatr Med Assoc2013103650851524297987
- ArtsMLde HaartMBusSABakkerJPHackingHGNolletFPerceived usability and use of custom-made footwear in diabetic patients at high risk for foot ulcerationJ Rehabil Med201446435736224356801
- BreuerUDiabetic patient’s compliance with bespoke footwear after healing of neuropathic foot ulcersDiabet Metab1994204415419
- ChurchmanNA retrospective audit of footwear use by high-risk individuals in North DerbyshireDiabetic Foot J20081111018
- MacfarlaneDJJensenJLFactors in diabetic footwear complianceJ Am Podiatr Med Assoc200393648549114623991
- LenkerJAPaquetVLA new conceptual model for assistive technology outcomes research and practiceAssist Technol200416111015357144
- van NettenJJDijkstraPUGeertzenJHPostemaKWhat influences a patient’s decision to use custom-made orthopaedic shoes?BMC Musculoskelet Disord2012139222682404
- BongaertsBWRathmannWHeierMOlder subjects with diabetes and prediabetes are frequently unaware of having distal sensorimotor polyneuropathy: the KORA F4 studyDiabetes Care20133651141114623275355
- NatovichRKushnirTHarman-BoehmICognitive dysfunction: part and parcel of the diabetic footDiabetes Care20163971202120727208339
- BusSAWaaijmanRNolletFNew monitoring technology to objectively assess adherence to prescribed footwear and assistive devices during ambulatory activityArch Phys Med Rehabil201293112075207922771483
- GershaterMALondahlMNybergPComplexity of factors related to outcome of neuropathic and neuroischaemic/ischaemic diabetic foot ulcers: a cohort studyDiabetologia200952339840719037626
- Van De WegFBVan Der WindtDAVahlACWound healing: total contact cast vs custom-made temporary footwear for patients with diabetic foot ulcerationProsthet Orthot Int200832131117943623
- HelmPAWalkerSCPulliumGFRecurrence of neuropathic ulceration following healing in a total contact castArch Phys Med Rehabil199172129679701953319
- SoorikumaranSSurgical footwearBMJ198929967059762508959
- ArkesHRBlumerCThe psychology of sunk costOrgan Behav Hum Dec1985351124140
- Christensen-SzalanskiJJNorthcraftGBPatient compliance behavior: the effects of time on patients’ values of treatment regimensSoc Sci Med19852132632733929392
- JayasingheSAAtukoralaIGunethillekeBSiriwardenaVHerathSCDe AbrewKIs walking barefoot a risk factor for diabetic foot disease in developing countries?Rural Remote Health20077269217571928
- ShankhdharKShankhdharLKSkankhdharUDiabetic foot care in the land of no podiatristsWCET J20082812023
- JohnsonMNewtonPGoyderEPatient and professional perspectives on prescribed therapeutic footwear for people with diabetes: a vignette studyPatient Educ Couns2006641–316717216469472
- AronsonJKCompliance, concordance, adherenceBr J Clin Pharmacol200763438338417378797
- van NettenJJJanninkMJHijmansJMGeertzenJHPostemaKLong-term use of custom-made orthopedic shoes: 1.5-year follow-up studyJ Rehabil Res Dev201047764364921110260
- van NettenJJJanninkMJHijmansJMGeertzenJHPostemaKUse and usability of custom-made orthopedic shoesJ Rehabil Res Dev2010471738120437329
- MuellerMJSmithKECommeanPKRobertsonDDJohnsonJEUse of computed tomography and plantar pressure measurement for management of neuropathic ulcers in patients with diabetesPhys Ther199979329630710078773
- PatonJRobertsAGlasserSCollingsRMarsdenJ“All I wanted was a pair of shoes”: a qualitative case studyDiabetic Foot J2014173100106
