Abstract
Purpose
To quantify clinical trial participants’ and investigators’ judgments with respect to the relative importance of efficacy and safety attributes of antipsychotic treatments for schizophrenia, and to assess the impact of formulation and adherence.
Methods
Discrete-choice experiment surveys were completed by patients with schizophrenia and physician investigators participating in two phase-3 clinical trials of paliperidone palmitate 3-month long-acting injectable (LAI) antipsychotic. Respondents were asked to choose between hypothetical antipsychotic profiles defined by efficacy, safety, and mode of administration. Data were analyzed using random-parameters logit and probit models.
Results
Patients (N=214) and physicians (N=438) preferred complete improvement in positive symptoms (severe to none) as the most important attribute, compared with improvement in any other attribute studied. Both respondents preferred 3-month and 1-month injectables to oral formulation (P<0.05), irrespective of prior adherence to oral antipsychotic treatment, with physicians showing greater preference for a 3-month over a 1-month LAI for nonadherent patients. Physicians were willing to accept treatments with reduced efficacy for patients with prior poor adherence. The maximum decrease in efficacy (95% confidence interval [CI]) that physicians would accept for switching a patient from daily oral to 3-month injectable was as follows: adherent: 9.8% (95% CI: 7.2–12.4), 20% nonadherent: 25.4% (95% CI: 21.0–29.9), and 50% nonadherent: >30%. For patients, adherent: 10.1% (95% CI: 6.1–14.1), nonadherent: the change in efficacy studied was regarded as unimportant.
Conclusion
Improvement in positive symptoms was the most important attribute. Patients and physicians preferred LAIs over oral antipsychotics, with physicians showing a greater preference for 3-month over 1-month LAI. Physicians and patients were willing to accept reduced efficacy in exchange for switching a patient from an oral formulation to a LAI.
Introduction
Schizophrenia, a chronic and severe psychiatric disorder, impairs psychosocial functioning, significantly diminishes quality of life, and requires continuous, long-term antipsychotic treatment.Citation1,Citation2 Treatments should balance reducing psychotic and functional symptoms while minimizing treatment-induced adverse events (AEs).Citation3 While clinical trials and observational studies provide information on the frequency of symptoms and events, benefit–risk decisions also require judging the clinical impact of these outcomes. These value judgments have traditionally been based on a physician’s perspective,Citation4 but there is increasing interest in using patient’s inputCitation5–Citation7 for clinical and regulatory decision-making. The US Food and Drug Administration (FDA) Center for Drug Evaluation and Research,Citation8 the European Medicines Agency, and Health Canada have taken steps to better understand and incorporate patient perspectives in benefit–risk evaluations.Citation9–Citation11 The FDA Center for Devices and Radiological Health specifically recommended incorporating patient preference information into premarket review to inform benefit–risk assessment,Citation9,Citation12,Citation13 a view strongly endorsed by several patient advocacy groups and public–private partnerships.Citation14,Citation15
Previous preference studies in schizophrenia, performed with online panels of psychiatrists and patients, demonstrated that schizophrenia patients were capable of completing such surveys,Citation16,Citation17 and that both physicians and patients place greater importance on improvements in positive symptoms than on improvements in negative symptoms or in avoiding treatment-related AEs (weight gain, extrapyramidal symptoms [EPS], hyperglycemia, and hyperprolactinemia).Citation18,Citation19 Patient adherence to oral antipsychotics was identified as an important factor in the assessment of oral versus injectable medicine formulations.Citation20–Citation22 For example, in pilot studies using online panels of patients and physicians, respondents preferred long-acting injectables (LAIs) over daily oral antipsychotics for hypothetical patients with past nonadherence to antipsychotics, though patients preferred the oral formulation for patients with high prior adherence.Citation18,Citation19 An important open question is whether the results of these pilot studies are reproducible in different samples, and particularly, whether the online panel results accurately reflect the preferences of schizophrenia patients who meet the clinical trial inclusion/exclusion criteria.Citation18,Citation19
This paper describes the results of preference surveys administered to trial participants and physician investigators during two phase-3, multinational clinical studies (NCT01515423 and NCT01529515)Citation23,Citation24 of paliperidone palmitate 3-month (PP3M) formulation, a LAI antipsychotic. The objective of these surveys was to quantify patient and physician preferences related to benefits and risks of antipsychotic treatments for schizophrenia, and to assess the impact of past patient adherence on the relative importance of treatment efficacy and formulation.
Methods
Two discrete-choice experiment (DCE) surveys, one for patients with schizophrenia and one for psychiatrists treating such patients, were incorporated into Trial-1 (NCT01515423) and Trial-2 (NCT01529515) as a prespecified exploratory end point requirement within the clinical protocols (–). In both of these randomized double-blind multicenter trials, men and women, aged 18–70 years (inclusive), diagnosed with schizophrenia (Diagnostic and Statistical Manual of Mental Disorders, 4th Edition [DSM-IV-TR], criteria) for >1 year before screening, and with a total Positive and Negative Syndrome Scale (PANSS) score between 70 and 120 (<120 for Study 2) at screening and baseline, were enrolled. Patients symptomatically stable on LAI antipsychotic treatments (including once-monthly PP [PP1M]) other than PP3M were eligible for study entry.
The key exclusion criteria were as follows: primary, active DSM-IV diagnosis other than schizophrenia; significant risk of suicidal behavior; history of substance dependence within 6 months before screening; involuntary status in a psychiatric hospital at screening; history of neuroleptic malignant syndrome, tardive dyskinesia, or any malignancy in the previous 5 years, except for basal cell carcinoma. Detailed descriptions of the two trials have been published.Citation20,Citation21 These surveys were adapted from versions used in pilot studies conducted with patients and physicians sampled from online panels.Citation18,Citation19
Preference surveys
Survey instruments
Design and testing of the surveys are described in the pilot studies.Citation18,Citation19 Briefly, DCEs offer a systematic way to elicit trade-offs and quantify the relative importance of treatment attributesCitation25 by asking respondents (physicians and patients) to evaluate which of the several hypothetical treatment profiles they judge to be more appropriate for a hypothetical patient in a series of choice questions.Citation19 Preferences were estimated by regressing treatment choices on the systematically altered features of each treatment profile.Citation26
The attributes were intended to incorporate aspects of treatment-related efficacy, safety, and mode of administration that patients and physicians take into account when choosing a therapy. The patient and physician surveys included analogous sets of attributes and levels, with labels adapted for each group of respondents. The first series of questions assessed the relative importance of three benefit attributes (improvements in positive symptoms, negative symptoms, and social functioning) and four risk (AEs) attributes (weight gain, EPS, hyperprolactinemia, and hyperglycemia). A second series of questions evaluated the effect of past patient adherence on preferences for the mode of administration (oral, 1-month LAI, 3-month LAI) and treatment efficacy. The physician survey also included the probability of EPS in the second series of questions. Each question in this series was asked with a primary and a follow-up question. First, respondents were asked to choose between treatments that could be administered to an adherent patient, ie, by pill or by injection, where the efficacy varied between treatments. Second, they were given additional information about the hypothetical schizophrenia patient’s past history of missing doses of oral medications and then asked to choose between the same medications. To lessen patient respondent burden, patient respondents were only asked this second question if they chose the oral formulation initially.
Survey participants
Physicians
English-speaking physicians who participated either as a principal investigator or as a subinvestigator in two clinical trials, and had direct contact with patients, were invited to complete the web-based preference survey. Invitations were sent ~3 months after their site opened, to allow physicians to have experience with a 3-month LAI. Physicians were excluded if their English skills were insufficient for the survey.
Patients
English-speaking patients enrolled at study sites in English-speaking countries (Australia, Canada, and the USA) in both trials were administered the survey on a tablet computer during a scheduled visit. Patients were asked to complete the survey at week 13 or later to allow treatment experience with a LAI.
Sample requirements
Survey requirements were prespecified: respondents were required to complete at least one survey choice question and at least one response from each of the two columns (A or B) when all eight questions in the first set of tasks were completed. Additionally, patient survey duration of at least 7 minutes was prespecified for a valid attempt. If a patient survey did not meet the above-mentioned criteria, up to one retest was requested. Completed surveys that did not meet these requirements were excluded from the analyses.
The survey was administered during the maintenance phases of the trials; if the patient’s condition was not stable enough (in the opinion of the investigator or site coordinator) to give sufficient attention to the survey during a scheduled visit, then the survey was scheduled for a subsequent visit. If the patient chose to withdraw from the study prior to study completion, then the patient was requested to complete the survey by the last visit, provided the study coordinator thought the patient would give the survey the required time and attention.
The survey and recruiting methods were approved by RTI International’s Institutional Review Board. Development and testing of the surveys were conducted according to good research practicesCitation25,Citation27 and involved key opinion leaders, physicians, and patients to ensure appropriateness of content. All patients were informed of their rights as survey participants. Patients provided an informed consent to participate in the survey by clicking “Yes, I agree to participate” in tablet devices. Physicians were exempt from providing informed consent.
Statistical analysis
Responses to the first series of choice questions were analyzed using a random-parameters logit model, where the choice of treatment profile was dependent upon attribute levels, specified as categorical effect-coded variables. The model estimated relative preference weights and importance scores for all attribute levels included in the surveys.
Physicians’ responses to the second series of choice questions were analyzed using a bivariate-probit model that jointly considered respondents’ answers to the primary and follow-up questions and estimated attribute-level weights that maximized the likelihood of both answers by respondents.Citation26 For patients, preference weights for primary and follow-up questions were computed using separate probit models, and the standard errors for both the models were standardized to account for correlations between models post-estimation. Heterogeneity of the first set of preferences among predefined subgroups was examined using the Wald test. Physician subgroups included sex, region, years in practice, % of patients treated with LAIs, and perceived patient adherence. Patient subgroups included trial, age, baseline PANSS score, body mass index, employment status, previous experience with LAIs, and reported adherence.
Second-series preference weights were used to compute the mean maximum acceptable reduction in benefit that would offset increases in utility associated with changes in treatment formulation for hypothetical patients with different levels of past adherence. Both analyses were conducted using NLOGIT 4.0 (Econometric Software, Inc., Plainview, NY, USA).
The random-parameters logit and probit models produced unique preference weights for each attribute level. The difference between these weights for best and worst attribute levels can be interpreted as the overall mean relative importance associated with moving from the least preferred to the most preferred level of that attribute.Citation5,Citation7,Citation28 In this study, the highest mean relative importance score from each model was assigned a value of 10 and was used to scale the mean relative importance for each of the other attributes.
Results
Participant demographics
Physicians
Invitations to complete the survey were sent to 588 physicians; 60 did not meet the eligibility criteria and 76 were excluded due to language issues. A total of 452 physicians in 27 countries completed the survey and answered at least one choice question; however, 14 physicians selected the same response (A or B) for all eight choice questions in the first series and were thus excluded, leaving 438 physician surveys with usable data. Most of the respondent physicians were men (n=255, 58.5%), and ~73% (n=318) had been practicing medicine for ≥10 years. The respondent physicians were from broad geographical regions ().
Table 1 Demographic characteristics of physicians and patients
Patients
The patient survey was a protocol requirement. However, patients who withdrew or relapsed prior to week 13 of the trial were not administered the survey. Thirty-eight patients did not meet the prespecified survey requirements on the initial test; of whom 5 refused a retest and 19 had usable retest data. A total of 219 patients from the two clinical trials completed the survey and answered at least one choice question. Of those 219 respondents, five patients who selected the same response (A or B) for all eight choice questions were excluded. The majority of patients who participated in the survey were men (n=166, 77.6%) and African-American (n=123, 57.5%) with a mean age of 40.5 years (), whereas the majority of trial patients were men (60%) and white (n=1,077, 60%) with a mean age of 38.4 years.
Benefit and risk trade-offs
Physicians
Analysis of the first series of choice tasks indicated that physicians considered complete improvement in positive symptoms (from no improvement to very much improved) as the most important attribute () and was assigned an importance value of 10. Physicians appraised all remaining efficacy attributes (improved social functioning: 7.38; improved negative symptoms: 5.19) as more important than elimination of any of the side effects assessed (hyperglycemia: 2.38; EPS: 2.30; 15% weight gain: 1.61; and hyperprolactinemia: 1.59). Physicians valued total improvement in negative symptoms (no improvement to very much improved) as approximately half as important as total improvement in positive symptoms ().
Figure 1 Preference weights for first series of choice questions for physicians.
Abbreviations: CI, confidence interval; EPS, extrapyramidal symptoms; N, number of respondents who answered the question.

Patients
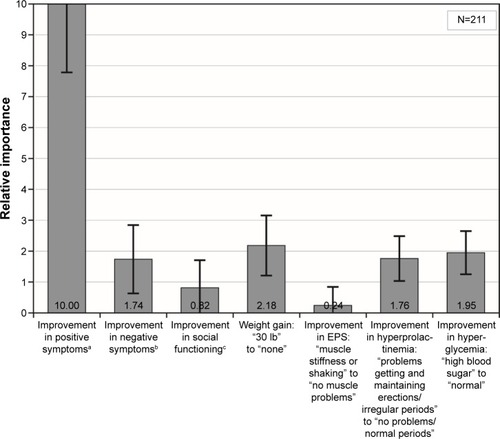
Analysis of the first series of choice tasks indicated that patients considered complete improvement in positive symptoms (from severe to none) as the most important attribute (relative importance: 10) and was four times as important as any other efficacy endpoint (improved negative symptoms: 1.74; improved social functioning: 0.82) or AE (no weight gain: 2.18; no hyperglycemia: 1.96; no hyperprolactinemia: 1.76) assessed in the survey ().
Figure 2 Preference weights for first series of choice questions for patients.
Abbreviations: CI, confidence interval; EPS, extrapyramidal symptoms; N, number of respondents who answered the question.
There were no statistically significant differences between the estimated preferences for the first series of choice questions for any of the physician or patient subgroups.
Effect of formulation and adherence
Physicians
Physicians had higher preference for LAI over a daily pill (P<0.05) for both adherent and nonadherent patients (). Physicians preferred the 3-month over 1-month LAI for patients with a history of skipping 20% (P=0.02) and 50% (P=0.003) doses.
Figure 3 Relative importance assigned by physicians in second series of choice questions.
Abbreviations: CI, confidence interval; EPS, extrapyramidal symptoms; N, number of respondents who answered the question.
In exchange for switching an adherent patient from a daily oral to a 1-month LAI, physicians would be willing to accept up to a 8.9% (95% confidence interval [CI]: 6.4–11.5) decrease in the percentage of patients with at least minimally improved positive symptoms (efficacy). For 20% nonadherent (missing 20% doses) and 50% nonadherent (missing 50% doses) patients, the maximum acceptable decrease in efficacy was 21.2% (95% CI: 17.3–25.0) and 35.6% (95% CI: 27.8–43.4), respectively. Similarly, in exchange to switching from a daily oral to a 3-month LAI, physicians would be willing to accept a reduction in efficacy of 9.8% (95% CI: 7.2–12.4), 25.4% (95% CI: 21.0–29.9), and >30% for adherent, 20% nonadherent, and 50% nonadherent patients, respectively. While the formal calculation of maximum acceptable risk for adherent patients yields 42.8% (95% CI: 33.3–52.4), because the survey only considered a range of efficacy from 20% to 50% chance of minimal improvement, it is not possible to state the maximum acceptable risk beyond this range of 30%.
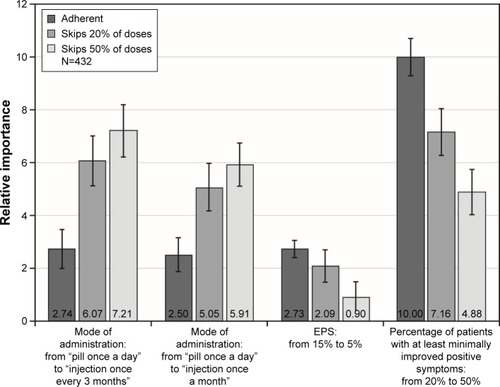
Patients
The adherence choice tasks enquired about nonadherence at two levels: missing 20% and 50% of doses; there was no difference between these results, which were pooled and referred to as nonadherent.
For both adherent and nonadherent patients, both 1-month and 3-month LAIs were preferred to daily pills (P<0.05). Differences in preference between 1-month and 3-month LAIs were not significant (). When adherence and efficacy were jointly assessed, respondents clearly valued increasing efficacy for a hypothetical adherent patient, ie, increasing the percentage of patients with mild versus severe positive symptoms. However, for a nonadherent patient, the differences in preference weights were very small, slightly disordered, and not statistically significantly different, suggesting that respondents saw little value in improvements in the probability of efficacy for nonadherent patients.
Figure 4 Relative importance assigned by patients to second series of choice questions.
Abbreviations: CI, confidence interval; N, number of respondents who answered the question.
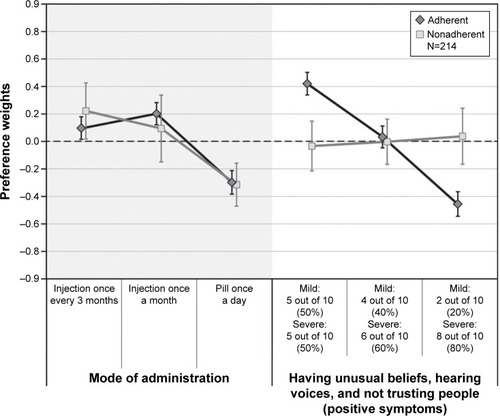
For a patient switching from a daily oral to a 3-month LAI, the maximum acceptable decrease in efficacy was 10.1% (95% CI: 6.1–14.1) for adherent patients. As patients placed no value on improving efficacy over the range assessed in the survey for a nonadherent patient, estimation of maximum acceptable decrease in efficacy was not possible to determine.
Discussion
An understanding of patient and physician priorities regarding treatment, and a patient’s active involvement in selecting a disease management strategy, is important in regulatory decisions, in clarifying acceptable medical options, and in choosing an appropriate treatment.Citation12,Citation29 This is the first time a DCE for both patients and physicians has been successfully incorporated into a clinical trial, and it may play an important role in the assessments of patients’ and physicians’ preferences in future clinical studies.
Physicians and patients placed the greatest importance on improvement in positive symptoms. Although improvements in positive symptoms were the main feature that drove patients’ preferences, physicians regarded total improvement in negative symptoms and social functioning as at least 50% as important as total improvement in positive symptoms. While the rationale behind the measured relative importance scores was not studied, one possible explanation is that patients may understand the dangers associated with severe positive symptoms, while physicians’ first concern might be stabilizing a psychotic patient, considering that AEs are much more manageable by adjusting the dose and choice of antipsychotic.
In this survey, both physicians and patients preferred LAIs to a daily oral medication. Physicians judged LAIs superior to daily pills regardless of patient’s degree of adherence (P<0.05), with greater preference for the 3-month over 1-month LAI for nonadherent patients. As adherence decreased, physician preference for the LAIs increased, and physicians would accept a decrease in efficacy in exchange for switching a patient from a daily oral to a LAI. Patients also preferred a LAI over a daily pill for both adherent and nonadherent patients, with no significant difference observed between 1-month and 3-month LAIs.
Patients were indifferent to changes in the probability of efficacy (mild vs severe positive symptoms) over the 20%–50% range, assessed when making judgments about nonadherent patients, while they regarded such changes as important for adherent patients. In contrast, physicians regarded improvements in the probability of efficacy as important, regardless of the adherence level. While the survey did not address the motivation behind their choices, these results suggest that patient’s judge adherence as critical in treatment decisions. These results also indicate the importance of including adherence when conducting DCEs for indications where adherence is a known concern.
The findings of this study were comparable with those of pilot studies and other published studies.Citation18,Citation19,Citation30,Citation31 In those studies, respondents (physicians and/or patients) rated improvements in positive symptoms and social functioning as more important than improvement in negative symptoms and avoidance of AEs.Citation18,Citation19,Citation30,Citation31 Recent studies assessing patient and physician judgments about medications’ benefits and risks have shown that both made treatment decisions primarily on the basis of improvement in positive symptoms.Citation19,Citation32
There were several important limitations of this study. This survey measured and quantified preferences across benefits, risks, and mode of treatment administration, but these studies typically do not study the rationale behind respondent decisions. Also, the survey was designed to allow respondents to interpret the attributes consistently and as intended. However, it is not possible to prove consistent interpretation by respondents. Evaluation of choice tasks could be cognitively difficult for respondents, although the training section of the survey provided details on attribute definitions and practice questions, and the same instruments have been used successfully in earlier studies.Citation18,Citation19 Additionally, stated preference confronts respondents with hypothetical scenarios, and the choices indicated by patients do not have the same impact as the actual decisions. Hence, there was a potential for hypothetical bias.
Additional limitations were constraints on cognition that restricted the number of end points and levels of those end points that could be considered simultaneously by survey respondents. For reasons given previously,Citation18,Citation19 the levels of social functioning did not include “no symptoms” or “complete cure” level unlike positive and negative symptoms. If the full range of social functioning were incorporated, it might have shown greater importance than negative symptoms. These surveys were not designed to address the question of whether judgments would change depending on the experience with a particular AE. The survey assessed judgment, which is distinct from personal preference or choice. Schizophrenia patients are very sensitive about revealing their personal information, and prior surveys demonstrated that such patients answer hypothetical questions about judgments more easily than preferences.Citation17 Formulating the questions as judgments also avoided confusion with patients’ experiences and expectations about how treatments could affect their own emotional responses, encouraged objectivity, and reduced potential bias compared with a question about what patients would choose for themselves.Citation33,Citation34
Finally, several factors may limit the representativeness and generalizability of the preference results. The patient survey was administered within a few English-speaking countries and the physician survey was administered within a diverse range of countries, each with varying clinical and cultural practices. Both patients and physicians chose to participate in a clinical trial and had to satisfy the specific criteria. For these reasons, the sample may have preferences that differ from the underlying populations.
Conclusion
Preference surveys administered to trial participants and physician investigators of two phase-3, multinational clinical studies of LAI PP3M demonstrated that they appraised treatments primarily on the basis of improvement in positive symptoms. Both patients and physicians judged LAIs to be better than the oral formulation irrespective of patient’s adherence, wherein physicians showed greater preference for the 3-month over 1-month LAI. Additionally, these results suggest the importance of determining patients’ own preferences and physicians’ judgments in regulatory decisions and, potentially, individual treatment decision-making.
Author contributions
Drs Katz, Levitan, Gopal, Fairchild, Hauber, Pugh, and Weinstein contributed to the design of this study, data analysis, interpretation, and authorship. All authors met ICMJE criteria and all those who fulfilled those criteria are listed as authors. All authors had access to the study data, provided direction and comments on the manuscript, had final approval of the document, and made the final decision about where to publish these data.
Acknowledgments
The authors acknowledge Vaibhav Deshpande (SIRO Clinpharm Pvt. Ltd.) for writing support, Ashwini Patil, ISMPP CMPP™ (SIRO Clinpharm Pvt. Ltd., Thane, Maharashtra, India) for assistance with revisions and editorial support, and Ellen Baum (Janssen Research & Development, LLC, Raritan, NJ, USA) for additional editorial support for the development of this manuscript. Janssen Research & Development, LLC provided funding to RTI Health Solutions to conduct this study.
Supplementary materials
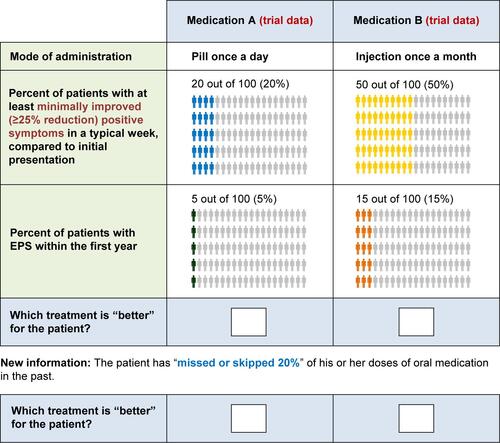
Figure S1 Example of physician discrete-choice question (first set).
Abbreviation: EPS, extrapyramidal symptoms.
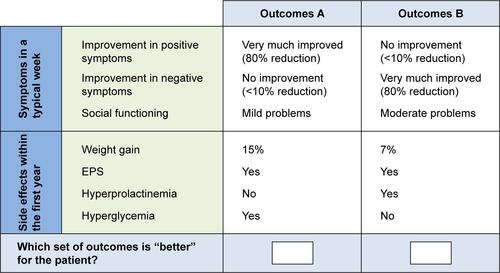
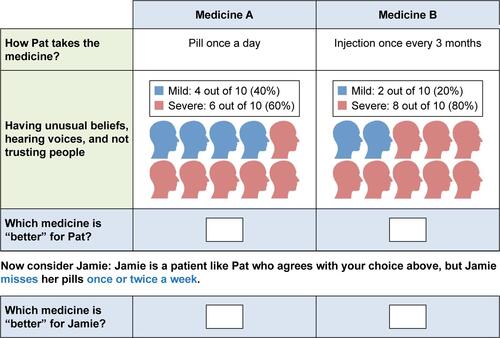
Figure S2 Example of patient (female) discrete-choice question (first set).
Abbreviation: Pat, patient.
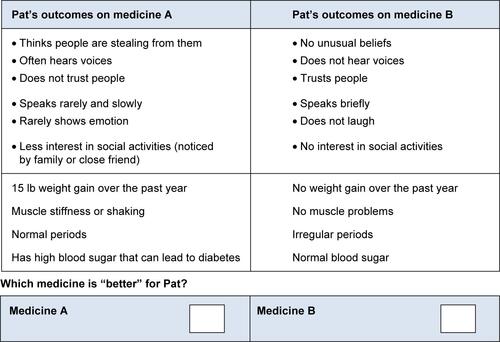
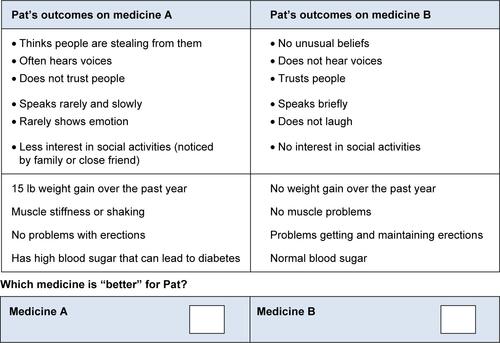
Figure S3 Example of patient (male) discrete-choice question (first set).
Abbreviation: Pat, patient.
Disclosure
Drs Katz, Gopal, Levitan, and Weinstein are employees of Janssen and hold company stocks. Dr Levitan is also a stockholder in Baxter International, Inc., Pharmaceutical Holdrs Trust, and Zimmer Holdings, Inc. He also owns stock in a variety of companies that at times include pharmaceutical and health care–related companies. Dr Hauber is an employee of RTI Health Solutions. Drs Pugh and Fairchild were employees of RTI Health Solutions at the time this study was conducted. The authors report no other conflicts of interest in this work.
References
- CoppolaDMelkoteRLannieCEfficacy and safety of paliperidone extended release 1.5 mg/day-a double-blind, placebo- and active-controlled, study in the treatment of patients with schizophreniaPsychopharmacol Bull2011442119
- KaneJMAgugliaEAltamuraACGuidelines for depot antipsychotic treatment in schizophrenia. European Neuropsychopharmacology Consensus Conference in Siena, ItalyEur Neuropsychopharmacol19988155669452941
- VolavkaJCitromeLOral antipsychotics for the treatment of schizophrenia: heterogeneity in efficacy and tolerability should drive decision-makingExpert Opin Pharmacother200910121917192819558339
- KienleGSKieneHClinical judgement and the medical professionJ Eval Clin Pract201117462162720973873
- BridgesJFMohamedAFFinnernHWWoehlAHauberABPatients’ preferences for treatment outcomes for advanced non-small cell lung cancer: a conjoint analysisLung Cancer201277122423122369719
- Brett HauberAMohamedAFBeamCMedjedovicJMauskopfJPatient preferences and assessment of likely adherence to hepatitis C virus treatmentJ Viral Hepat201118961962720579276
- MohamedAFHauberABNearyMPPatient benefit–risk preferences for targeted agents in the treatment of renal cell carcinomaPharmacoeconomics2011291197798821854079
- Food and Drug Administration (FDA)The voice of the patient: a series of reports from FDA’s Patient-Focused Drug Development Initiative2015 Available from: http://www.fda.gov/ForIndustry/UserFees/PrescriptionDrugUserFee/ucm368342.htmAccessed February 25, 2016
- European Medicines AgencyThe patient’s voice in the evaluation of medicinesHow patients can contribute to assessment of benefit and risk2013 Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Report/2013/10/WC500153276.pdfAccessed September 8, 2015
- European Medicines AgencyPatients to discuss benefit – risk evaluation of medicines with the Committee for Medicinal Products for Human Use2014 Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Press_release/2014/09/WC500173511.pdfAccessed 4 Jan 2016
- Health Canada, Government of CanadaArchived – Minister Ambrose announces patient involvement pilot for orphan drugs2014 Available from: http://news.gc.ca/web/article-en.do?mthd=tp&crtr.page=7&nid=873619&crtr.tp1D=1Accessed February 26, 2016
- Food and Drug Administration (FDA)Enhancing benefit-risk assessment in regulatory decision-making2014 Available from: http://www.fda.gov/ForIndustry/UserFees/PrescriptionDrugUserFee/ucm326192.htmAccessed September 7, 2015
- Center for Devices and Radiological Health (CDRH)Patient preference information – submission, review in PMAs, HDE applications, and De Novo requests, and inclusion in device labeling Draft Guidance for industry, food and Drug Administration Staff, and other stakeholders2015 Available from: http://www.fda.gov/ucm/groups/fdagov-public/@fdagov-meddev-gen/documents/document/ucm446680.pdfAccessed September 8, 2015
- Medical Device Innovation Consortium (MDIC)Patient Centered Benefit-Risk Project Report2015 Available from: http://mdic.org/wp-content/uploads/2015/05/MDIC_PCBR_Framework_Proof5_Web.pdfAccessed September 8, 2015
- Innovative Medicines Initiative (IMI)Europe 2 Programme: 5th Call for proposals2015 Available from: http://www.imi.europa.eu/sites/default/files/uploads/documents/IMI2Call5/IMI2_C5_PUBLICATION.pdfAccessed 5 Jan 2016
- RevickiDAShakespeareAKindPPreferences for schizophrenia-related health states: a comparison of patients, caregivers and psychiatristsInt Clin Psychopharmacol1996112101108
- BridgesJFKinterETSchmedingARudolphIMuhlbacherACan patients diagnosed with schizophrenia complete choice-based conjoint analysis tasks?Patient20114426727521995832
- LevitanBMarkowitzMMohamedAFPatients’ preferences related to benefits, risks, and formulations of schizophrenia treatmentPsychiatr Serv201566771972625772762
- MarkowitzMALevitanBSMohamedAFPsychiatrists’ judgments about antipsychotic benefit and risk outcomes and formulation in schizophrenia treatmentPsychiatr Serv20146591133113924828964
- CitromeLNew second-generation long-acting injectable antipsychotics for the treatment of schizophreniaExpert Rev Neurother201313776778323898849
- ShulerKMApproaches to improve adherence to pharmacotherapy in patients with schizophreniaPatient Prefer Adherence2014870171424868149
- KaplanGCasoyJZummoJImpact of long-acting injectable antipsychotics on medication adherence and clinical, functional, and economic outcomes of schizophreniaPatient Prefer Adherence201371171118024265549
- BerwaertsJLiuYGopalSEfficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trialJAMA Psychiatry201572883083925820612
- SavitzAJXuHGopalSEfficacy and safety of paliperidone palmitate 3-month formulation for patients with schizophrenia: a randomized, multicenter, double-blind, noninferiority studyInt J Neuropsychopharmacol2016197 pii:pyw018
- BridgesJFHauberABMarshallDConjoint analysis applications in health – a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task ForceValue Health201114440341321669364
- HanemannMLoomisJKanninenBStatistical efficiency of double-bounded dichotomous choice contingent valuationAm J Agric Econ199173412551263
- JohnsonFRLancsarEMarshallDConstructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task ForceValue Health201316131323337210
- HauberABMohamedAFJohnsonFRFalveyHTreatment preferences and medication adherence of people with Type 2 diabetes using oral glucose-lowering agentsDiabet Med200926441642419388973
- MullardAPatient-focused drug development programme takes first stepsNat Rev Drug Discov201312965165223989777
- ShumwayMSentellTChouljianTTellierJRozewiczFOkunMAssessing preferences for schizophrenia outcomes: comprehension and decision strategies in three assessment methodsMent Health Serv Res20035312113515224446
- ShumwayMSaundersTShernDPreferences for schizophrenia treatment outcomes among public policy makers, consumers, families, and providersPsychiatr Serv20035481124112812883140
- MarkowitzMLevitanBMohammedAPsychiatrists’ preferences for benefit and risk outcomes and formulation in schizophrenia treatments: a conjoint analysis studyPoster Presentation (PS5-05) at the Institute on Psychiatric ServicesOctober 4–7; 2012New York, NY
- Marta-PedrosoCFreitasHDomingosTTesting for the survey mode effect on contingent valuation data quality: a case study of web based versus in-person interviewsEcol Econ2007623–4388398
- NielsenJSUse of the Internet for willingness-to-pay surveys: a comparison of face-to-face and web-based interviewsResour Energy Econ2011331119129