Abstract
The information–motivation–behavioral skills (IMB) model has been used to explain and promote medication adherence among patients with diabetes and HIV. The objective of this study was to examine whether the IMB model predicted medication adherence among vasculitis patients. Adult vasculitis patients (n=228) completed online questionnaires at baseline and 3-month follow-up. Linear regressions were calculated to determine the direct effects of information and motivation on medication adherence (P<0.05). A mediation analysis using a bootstrapping approach was used to test whether behavioral skills significantly mediated the effect of information and motivation on medication adherence. Participants reported high levels of information (M=4.0; standard deviation [SD]=0.68), moderate levels of motivation (M=2.7; SD=1.00), and high levels of behavioral skills (M=4.1; SD=0.74). In the regression model, only behavioral skills (B=0.38; P<0.001) were significantly associated with medication adherence; however, mediation analysis revealed that behavioral skills significantly mediated the effects of information and motivation on medication adherence. The results support the IMB-hypothesized relationships between information, motivation, behavioral skills, and medication adherence in our sample. Findings suggest that providers should work with vasculitis patients to increase their medication-related skills to improve medication adherence.
Introduction
Vasculitis is a rare disease that thickens, narrows, and scars the blood vessels.Citation1 It is associated with adverse health outcomes such as organ damageCitation1 and higher health care costs.Citation2 It has been found that low medication adherence is common among patients with vasculitis.Citation3 As vasculitis only affects ~30 per 100,000 individuals in the United States,Citation4 few interventions have been designed to promote medication adherence among patients with vasculitis. Therefore, a paucity of literature exists to assist public health researchers and physicians to increase their knowledge of modifiable behavioral skills that could be used to increase medication adherence behaviors among patients with vasculitis.Citation5,Citation6
Studies have established that poor vasculitis management, including medication adherence, is a predictor of adverse outcomes and lower the patient’s quality of life.Citation7–Citation12 Management of vasculitis includes adhering to the provider’s recommendations with respect to timing, dosage, and frequency of the medication regimen, being motivated to adhere to the medication regimen, and applying behavioral skills to adhere to their medication regimen in multiple settings and situations.Citation13,Citation14 Few studies have applied theoretical frameworks to understand vasculitis self-management behaviors. These studies have found that more conflicting medication information and less social support from network members (individuals who provide emotional, instrumental, informational, and appraisal) have been associated with worse medication adherence.Citation5,Citation6,Citation15,Citation16 For example, patients who received high social support from their providers had higher levels of motivation to adhere to medication regimen resulting in better medication adherence.Citation5,Citation13 Additional work has described the medication information-seeking behaviors of vasculitis patients, but has not examined whether medication information seeking is associated with increased behavioral skills (self-efficacy) or medication adherence.Citation15
The information–motivation–behavioral skills (IMB) model of health behavior change is a theoretical model that was developed to predict HIV preventive behavior. However, the IMB constructs can be applied to multiple health promotion behaviors including medication adherence among different populations.Citation17 Overall, the results of cross-sectional studies from individuals diagnosed with HIV have demonstrated support for the IMB model in designing interventions that improve and predict antiretroviral medication adherence among individuals living with HIV.Citation18–Citation22 The IMB model has also been applied successfully in assessing medication adherence among diabetic patients.Citation14 Therefore, the IMB model has proven to be effective in promoting medication adherence among other diseases and may be potentially successful among patients with vasculitis. Although many behavioral-specific theories such as the Health Belief Model,Citation23 the Theory of Planned Behavior,Citation24 and the Transtheoretical ModelCitation25 posit determinants of behavior that are amenable to change, the IMB model is the only model that includes adherence-specific information, motivation, and behavioral skills as needed for successful adherence among patients with vasculitis.
Given that information sources may be more limited for patients living with a rare disease, such as vasculitis, the IMB model offered a unique framework with which to investigate the effects of medication information on patient adherence. The IMB model posits that an individual who is well informed, motivated, and has the requisite behavioral skills (including a high level of self-efficacy) will enact and maintain a health promotion behavior such as medication adherence.Citation17 According to the IMB model, information is defined as adequate knowledge of the medication regimen, side effects, drug interactions and adherence, as well as heuristics and implicit theories.Citation26 Heuristics are rules permitting cognitively effortless behavior regarding adherence, whereas implicit theories are a set of beliefs that require cognitive effort to apply adherence decision-making skills.Citation26 Motivation consists of personal and social attitudes and beliefs about medication adherence (I do not like taking my vasculitis medicines because they remind me that I have vasculitis). Personal motivation is comprised of the individual’s attitudes and beliefs, whereas social motivation is comprised of social and instrumental support for medication adherence.Citation26 Lastly, behavioral skills is comprised of objective abilities to perform adherence behaviors (the ability to take and properly store medications) and self-efficacy (the confidence in the ability to perform such adherence behaviors). Thus, medication adherence is defined as the result of the individual being informed about the treatment regimen, motivation to adhere to the regimen, and having the behavioral skills (self-efficacy) to adhere to the regimen in multiple contexts such as the work and home setting. The IMB model specifically posits that behavioral skills mediate the effects of information and motivation on medication adherence.
The objective of this paper is to examine whether information, motivation, and behavioral skills predict medication adherence for vasculitis patients. We specifically investigate whether information and motivation directly affect medication adherence or whether they are mediated via behavioral skills. Based on the relationships posited in the IMB model, we hypothesized that more adherence-related information, greater motivation, and higher levels of behavioral skills would be significantly associated with higher vasculitis medication adherence among patients. We also hypothesized that behavioral skills would significantly mediate the positive effects of information and motivation on patient medication adherence.
Methods
Study design
Data for this analysis come from the Accessing Social Support in Symptom Treatment (ASSIST) study, which was a longitudinal study that assessed how social support and information seeking influenced patient medication adherence among patients diagnosed with vasculitis. Data collection was from June 2008 to February 2009.Citation6
Recruitment
A convenience sample of participants was recruited through four methods including distributing study brochures at a vasculitis patient conference (n=39), mailing recruitment letters to vasculitis patients who were part of the Glomerular Disease Collaborative Network (GDCN) (n=361), contacting physician-diagnosed vasculitis patients (n=124), and posting study information on vasculitis websites, and patient newsletters, email groups, and support group meetings (n=147). Carpenter et al describe these recruitment efforts in greater detail.Citation6
Sample
Participants completed two online questionnaires administered 3 months apart. Inclusion criteria included 1) patients who had a self-reported diagnosis of vasculitis; 2) were ≥18 years of age; 3) were able to read and write in English; 4) had Internet access; and 5) currently taking at least one vasculitis medication. Out of 306 patients, 253 patients were eligible for the study. Reasons for ineligibility included currently not taking vasculitis medications (n=25), death (n=9), lack of access to the Internet (n=9), being too busy (n=4), not having vasculitis (n=1), and refusing to participate in the study (n=5). A total of 232 patients (91.7%) of the 253 eligible patients completed the 1-hour baseline questionnaire. Yet technical issues (n=7), being too sick (n=4), being too busy (n=3), or never responding to study correspondence (n=7) were reasons for non-completion. Of the 232 participants who completed the baseline survey, only four did not complete the 3-month follow-up survey. Three were lost to follow-up and one experienced technical difficulties. Thus, resulting in a final sample of 228 participants and a 98.2% study completion rate. Participants who completed both questionnaires received a ten-dollar gift card. Written informed consent was obtained from all individual participants included in the study. This study was approved by the University of North Carolina at Chapel Hill Institutional Review Board.
Measures
The baseline questionnaire assessed sociodemographic characteristics, disease status, and the information measure of the IMB model. The 3-month questionnaire assessed vasculitis medication adherence, motivation, and behavioral skills measures of the IMB model.
Sociodemographic and clinical characteristics
Participants answered one item regarding age (in years), gender, race/ethnicity (categorized as Non-Hispanic White vs other), education (in years), health insurance status (insured vs uninsured), disease duration (in years), perceived vasculitis severity (1= not at all severe to 10= extremely severe), relapse status (currently experiencing a flare vs not), and vasculitis type (ie, granulomastosis with polyangiitis, microscopic polyangiitis, eosinophilic granulomatosis with Polyangiitis, anti-neutrophil cytoplasmic autoantibody, Takayasu arteritis, polyarteritis nodosa, Behcet’s disease, do not know, and other).
IMB constructs
IMB model constructs were assessed using the validated and reliable LifeWindows questionnaire (LW-IMB-AAQ).Citation27 The IMB questionnaire contains three subscales, including information, motivation, and behavioral skills. Because the IMB questionnaire had not been used previously with a vasculitis patient population, we conducted five cognitive interviews with patients to assess the comprehension and relevance of the questionnaire items. Cognitive interviews are defined as a technique that allows individuals to verbalize their opinions and feelings when examining information on a specific topic.Citation28 Based on the results of these interviews, one item was omitted from the motivation scale because this item referred to stigma, which is less of an issue with vasculitis patients than HIV patients (). We also conducted a confirmatory factor analysis with three factors and promax rotation to assess item loadings. Six items were omitted for the following reasons: two informational scale items cross-loaded with the behavioral skills scale and one information scale item did not load on any factor, and two items on the behavioral skills scale cross-loaded on the information scale ().
Table 1 Sample characteristics (N=228)
In this study, our final measure included six information items, six motivation items, and ten behavioral skills items. The information scale included items about possible side effects, how to take the medications, and what action to take if a dose is missed. Motivation items were reverse-scored so that higher motivation scores indicated more positive medication attitudes and beliefs. Examples of motivation items included being frustrated, upset, and worried about taking vasculitis medications; higher motivation scores indicated more negative medication attitudes and beliefs. Behavioral items were reverse-scored so that higher values reflected higher levels of behavioral skills (self-efficacy). Behavioral items included such items as managing side effects, storing medications properly, and refilling medications on time. Participants responded to the information and motivation items using a 5-item scale including 1= “strongly disagree,” 2= “somewhat disagree,” 3= “neither,” 4= “somewhat agree,” and 5= “strongly agree.” The participants responded to the behavioral skills items using a 5-item scale including 1= “very easy,” 2= “fairly easy,” 3= “neither,” 4= “fairly hard,” 5= “very hard.” Summary subscale scores were created by averaging item responses. Higher scores indicated greater levels of vasculitis knowledge, vasculitis skills, and motivation (attitudes and beliefs of vasculitis management). The Cronbach’s alphas were acceptable to excellent for the subscales: information (α=0.70), motivation (α=0.82), and behavioral skills (α=0.91).
Vasculitis medication adherence
The Vasculitis Self-Management Survey (VSMS) medication adherence subscale measured medication adherence.Citation29 Participants self-reported their medication taking behavior during the past 4 weeks. A summary score was created by averaging item responses and had a possible range of 0–35. The scale was comprised of seven items on a 5-point Likert scale. For six items, the scale ranged from 1= “none of the time” to 5= “all of the time.” For example, “I skipped a dose of my medicine” and “I could have done a better job following my health professionals’ recommendations for taking my medicine” were items on the medication adherence scale. The seventh item (percentage of recommended medications taken exactly as directed) ranged from 1= “0%–24%” to 5= “100%.” In a prior study,Citation29 the subscale had an acceptable internal consistency (Cronbach’s α=0.77) and test–retest reliability of 0.60. The Cronbach’s alpha was 0.87 in the current study. Higher scores indicated greater adherence.
Statistical analyses
Univariate analyses were conducted to characterize the sample and variables of interest. Pearson correlation (bivariate analysis) was used to examine the associations among study variables. A linear regression was conducted to examine the direct effects of information, motivation, and behavioral skills on vasculitis medication adherence. The regression controlled for patients’ demographic and clinical characteristics included age, gender, education, race/ethnicity, insurance status, self-reported vasculitis type, disease duration, relapse status, and perceived vasculitis severity. P-values <0.05 were considered to be significant. All analyses were conducted using Statistical Package for Social Sciences software, version 22.0.
A bootstrapping approach was used to run a mediation model to explore whether behavioral skills mediated the effects of information and motivation on medication adherence.Citation30,Citation31 The mediation model controlled for age, gender, education, race/ethnicity, insurance status, disease duration, relapse status, and perceived vasculitis severity. Multiple reasons are presented below as to why bootstrapping was conducted rather than causal steps to test for mediation. First, bootstrapping is a nonparametric test that does not impose the constraint of multivariate normality; therefore, it is robust for situations where data are skewed. Vasculitis patients are relatively adherent;Citation29 thus, the mediation approach that we used is less affected by skewness offering advantages. Second, bootstrapping calculates an overall point estimate and confidence interval for each mediated (indirect) effect by generating a sampling distribution from 5,000 samples (with replacement) from the full data set reducing type I error rates.Citation31 Third, bootstrapping produces contrasts to test the relative strength of each mediated effect; yet, multiple mediators cannot be contrasted using a conventional causal steps approach.Citation32 Finally, bootstrapping with bias-corrected confidence intervals has more power (exceeds 0.80 for samples of 250) to detect significant specific indirect effects.Citation33 Bias-corrected 95% confidence intervals were used to determine whether the point estimates for each indirect effect were significant; confidence intervals that contained zero were considered non-significant. Participants with missing data were omitted from the analysis.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Results
Univariate analyses
A total of 228 individuals with vasculitis participated in the study (). Overall, participants reported high levels of information (M=4.0; SD=0.68), moderate levels of motivation (M=2.7; SD=1.00), high levels of behavioral skills (M=4.1; SD=0.74), and high levels of medication adherence (M=4.3; SD=0.69).
Bivariate analyses
presents the bivariate associations among study variables. Better vasculitis medication adherence was associated with more adherence-related information (r=0.23, P<0.01), higher motivation scores (r=0.33, P<0.01), more behavioral skills (r=−0.48, P<0.01), older age (r=0.23, P<0.01), and female gender (r=−0.16, P<0.05).
Table 2 Correlations of all study variables
Greater behavioral skills were associated with more adherence-related information (r=0.43, P>0.01), higher motivation scores (r=0.43, P>0.01), older age (r=0.21, P>0.01), lower perceived vasculitis severity (r=−0.20, P>0.01), currently–relapsing vasculitis status (r=0.18, P>0.01), and female gender (r=−0.16, P>0.05).
Regression analyses
presents linear regression results that examined the direct effects of information, motivation, and behavioral skills on medication adherence (adjusted R2=0.25). Only behavioral skills (B=0.38; P<0.001) were significantly associated with patient medication adherence; high levels of behavioral skills were related to high levels of medication adherence. The beta value of 0.38 indicates that a change of one standard deviation in the predictor variable (behavioral skills) would result in a change of 0.38 standard deviations in vasculitis medication adherence. None of the covariates were significantly related to medication adherence including attitudes and beliefs (motivation). A mediation analysis was then conducted to assess whether the non-significant effects of information and motivation were mediated by behavioral skills. Preacher and Hayes suggest that there are some circumstances in which an indirect mediation effect can occur without the presence of a significant direct effect.Citation30,Citation31
Table 3 Unstandardized beta (B) coefficients and P-values for linear regression predicting vasculitis medication adherence
Mediation analysis
presents the summary of the mediation analysis for the direct and indirect effect of information and motivation on medication adherence with behavioral skills as the mediating variable. As shown in , an examination of indirect effects revealed that motivation and information were positively related to behavioral skills, and behavioral skills were significantly associated with higher medication adherence.
Figure 1 Modeling the indirect effects of information and motivation on vasculitis medication adherence (n=208).
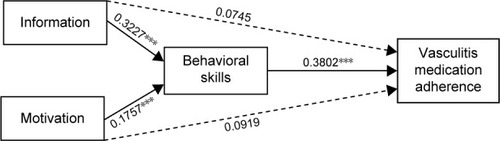
Table 4 Summary of mediation results for the direct and indirect effect of information and motivation on medication adherence with behavioral skills as the mediating variable (n=208)Table Footnotea
Discussion
We examined whether the IMB model could be applied to explain medication adherence among patients living with a rare chronic disease. The authors hypothesized that higher levels of information, motivation, and behavioral skills would be significantly associated with higher vasculitis medication adherence among patients and that the effects of information and motivation on adherence would be mediated by increased behavioral skills. After conducting a mediation analysis, we found support for the IMB-hypothesized relationships between information, motivation, behavioral skills, and medication adherence in our sample. Moreover, we found, as predicted by the IMB model, that behavioral skills mediated the effects of information and motivation on medication adherence.
Results revealed that behavioral skills significantly mediated the effects of information and motivation on medication adherence. These findings are similar with previous studies, which have also found that behavioral skills were associated with higher medication adherence among patients with an infectious diseaseCitation16,Citation17,Citation19,Citation20 and that behavioral skills mediated the effects of information and motivation on medication adherence.Citation34,Citation35 Although the IMB was developed to explain medication adherence in HIV patients, it is also applicable for patients living with a chronic rare disease such as vasculitis. Thus, our findings were comparable to other studies in that more positive motivation scores indicated higher behavioral skills.
Although these findings highlight the importance of the IMB model for promoting medication adherence, additional research is needed to explain what types of information are important to vasculitis patients. Additionally, qualitative studies are warranted to examine how to best address patients’ attitudes toward their medications in order to increase their motivation. Information and motivation are both key components for vasculitis patients’ medication adherence because they increase behavioral skills including self-efficacy. If vasculitis patients are experiencing medication adherence issues then health care providers may want to directly address these issues by providing credible adherence-related information and verify that patients have the skills necessary to properly adhere, including having accurate knowledge of how to take medications and incorporate medication-taking in their daily schedules. By implementing these recommendations, providers could potentially improve patient’s behavioral skills.
Limitations
Findings should be interpreted in light of the study’s limitations. First motivation, behavioral skills, and medication adherence were all measured at the 3-month data collection time point, which limits our ability to truly test whether mediation occurred. However, our results are consistent with the IMB model and previous studies. Second, the study sample is a convenience sample which is not representative of the larger vasculitis population; thereby, limiting generalizability. Future research should attempt to recruit a diverse sample (ie, race/ethnicity, gender, and education). Third, selection bias is present in the study because patient’s self-reported medication adherence (ie, relatively high adherence with low variance). Fourth, the information, motivation, and behavioral skills measures were limited because of the removal of items, although all measures had an acceptable Cronbach alpha. The authors removed certain items from the LW-IMB-AAQ questionnaire because those items were not relevant to patients with vasculitis or performed poorly on factor analysis. Lastly, this sample does not demonstrate the direct effects of information and motivation on medication adherence that have been seen in previous research among patients living with HIV. The results of the regression analysis indicated that only behavioral skills were a significant predictor of medication adherence.
Practical implications
Poor medication adherence among vasculitis patients can result in morbidity, mortality, and high health care expenses. Providers and public health professionals are in an essential position to increase vasculitis patients’ information, motivation, and behavioral skills when taking their medications. Our findings indicate that patients with higher levels of behavioral skills have better medication adherence. For this reason, providers may want to increase awareness of adverse events of medication non-adherence among vasculitis patients and propose practical strategies for increasing medication adherence. For example, physicians could possibly teach patients how to incorporate their medication into their daily schedule, assist the patient in finding an accessible pharmacy within close proximity of their home environment, or having the patient repeat the medication directions and proper storage of the medication during the office visit, which are all specific behavioral skills that could lead to better medication adherence.Citation36,Citation37 Also, our findings demonstrate that positive attitudes and beliefs were related to better medication adherence among our sample. It may be helpful to the patient if the provider asked about the patient’s personal and cultural beliefs when prescribing medications. This will not only help to assess the patients’ views of their medications but also help to build a trusting relationship among patients and health care providers. In addition, patients with negative attitudes and beliefs may benefit from a support groupCitation38,Citation39 to increase social support among vasculitis patients who may possibly feel alienated from family members and friends.
Conclusion
In conclusion, we found support for the applicability of the IMB model in explaining medication adherence for vasculitis patients. IMB model-based efforts could include strategies for health care providers to assist patients in increasing their information, motivation, and behavioral skills to promote medication adherence. Future studies should evaluate these efforts to demonstrate improvement in self-care behaviors including information quality to promote medication adherence among patients with vasculitis.
Acknowledgments
This research was supported by the Renal Epidemiology Predoctoral Traineeship at the UNC Kidney Center and the ACR REF/Abbott Health Professional Graduate Student Research Preceptorship (grant no T32DK007750).
Supplementary material
Table S1 Rotated factor loadings of IMB items: 3-factor solution
Disclosure
The authors report no conflicts of interest in this work.
References
- American College of RheumatologyVasculitis Available from: https://www.rheumatology.org/Practice/Clinical/Patients/Diseases_And_Conditions/Vasculitis/Accessed August 22, 2015
- RaimundoKFarrAMKimGDunaGClinical and economic burden of antineutrophil cytoplasmic antibody-associated vasculitis in the United StatesJ Rheumatol201542122383239126523026
- CarpenterDMHoganSLDevellisRFPredictors of medication non-adherence for vasculitis patientsClin Rheumatol201332564965723314654
- Cleveland ClinicCenter for Vasculitis Care and Research Available from: http://my.clevelandclinic.org/orthopaedics-rheumatology/departments-centers/rheumatic-immunologic-diseases/vasculitis.aspxAccessed August 22, 2015
- PepperJKCarpenterDMDeVellisRFDoes adherence-related support from physicians and partners predict medication adherence for vasculitis patients?J Behav Med201235211512322350097
- CarpenterDMDeVellisRFFisherEBDeVellisBMHoganSLJordanJMThe effect of conflicting medication information and physician support on medication adherence for chronically ill patientsPatient Educ Couns201081216917620044230
- AbularrageCJSlidellMBSidawyANKreishmanPAmdurRLAroraSQuality of life of patients with Takayasu’s arteritisJ Vasc Surg200847113113618178464
- Bernabe’EMarcenesWMatherJPhillipsCFortuneFImpact of Behcet’s syndrome on health-related quality of life: influence of the type and number of symptomsRheumatology (Oxford)201049112165217120675710
- CarpenterDMKadisJADeVellisRFHoganSLJordanJMThe effect of medication-related support on the quality of life of patients with vasculitis in relapse and remissionJ Rheumatol201138470971521285174
- CarpenterDMMeadorAEElstadEAHoganSLDevellisRFThe impact of vasculitis on patients’ social participation and friendshipsClin Exp Rheumatol2012301 Suppl 70S15S2122325346
- ErtamIKitapciogluGAksuKQuality of life and its relation with disease severity in Behcet’s diseaseClin Exp Rheumatol2009272 Suppl 531822
- ClarkNMBeckerMHJanzNKLorigKRakowskiWAndersonLSelf-management of chronic disease by older adults: a review and questions for researchJ Aging Health199131327
- MayberryLSOsbornCYEmpirical validation of the information-motivation-behavioral skills model of diabetes medication adherence: a framework for interventionDiabetes Care20143751246125324598245
- CarpenterDMThorpeCTLewisMDevellisRFHoganSLHealth related quality of life for patients with vasculitis and their spousesArthritis Rheum200961225926519177525
- CarpenterDMDevellisRFHoganSLFisherEDevellisBMJordanJMUse and perceived credibility of medication information sources for patients with a rare illness: differences by genderJ Health Commun201116662964221476166
- AlexanderDSHoganSLJordanJMDevellisRFCarpenterDMThe relationship between peer support, medication adherence, and quality of life among patients with vasculitisClin Exp Rheumatol2015332 Suppl 89185186
- FisherJDFisherWAThe information-motivation-behavioral skills modelDiClementeRCrosbyRKeglerMEmerging Theories in Health Promotion Practice and ResearchJossey-Bass, CAJohn Wiley & Sons20024070
- AmicoKRBartaWKonkle-ParkerDJThe information-motivation-behavioral skills model of ART adherence in a Deep South HIV+ clinic sampleAIDS Behav20091316675
- FisherJDFisherWAAmicoKRHarmanJJAn information-motivation-behavioral skills model of adherence to antiretroviral therapyHealth Psychol200625446247316846321
- HorvathKJSmolenskiDAmicoKRAn empirical test of the information-motivation-behavioral skills model of ART adherence in a sample of HIV-positive persons primarily in out-of-HIV-care settingsAIDS Care201426214215123724908
- KalichmanSCCherryJCainDNurse-delivered antiretroviral treatment adherence intervention for people with low literacy skills and living with HIV/AIDSJ Assoc Nurses AIDS Care2005165315
- MannheimerSBMorseEMattsJPTerry Beirn Community Programs for Clinical Research on AIDSSustained benefit from a long-term antiretroviral adherence intervention. Results of a large randomized clinical trialJ Acquir Immune Defic Syndr200643Suppl 1S41S4717091022
- HochbaumGMPublic Participation in Medical Screening Programs: A Socio-Psychological StudyWashington, DCU.S. Dept. of Health, Education, and Welfare1958
- FishbeinMAjzenIBelief, Attitude, Intention, and Behavior: An Introduction to Theory and ResearchReading, MAAddison-Wesley1975
- ProchaskaJODiClementeCCStages and processes of self-change of smoking: toward an integrative model of changeJ Consult Clin Psychol19835133903956863699
- FisherWAFisherJDHarmanJJThe information-motivation-behavioral skills model: a general social psychological approach to understanding and promoting health behaviorSulsJWallstonKSocial Psychological Foundations of Health and IllnessMalden, MABlackwell Publishing Ltd200382106
- The LifeWindows Project TeamThe LifeWindows Information Motivation Behavioral Skills ART Adherence Questionnaire (LW-IMB-AAQ) Center for Health, Intervention, and PreventionCT, USAUniversity of Connecticut2006
- BernardRSocial Research Methods: Qualitative and Quantitative Approaches2nd edThousand Oaks, CASage Publications2013
- ThorpeCTDevellisRFLewisMABlalockSJHoganSLDevellisBMDevelopment and initial evaluation of a measure of self-management for adults with antineutrophil cytoplasmic antibody-associated small-vessel vasculitisArthritis Rheum20075771296130217907222
- PreacherKHHayesAFSPSS and SAS procedures for estimating indirect effects in simple mediation modelsBehav Res Methods Instrum Comput200436471773115641418
- PreacherKJHayesAFAsymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator modelsBehav Res Methods200840387989118697684
- BaronRMKennyDAThe moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerationsJ Pers Soc Psychol1986516117311823806354
- BriggsNEEstimation of the standard error and confidence interval of the indirect effect in multiple mediator models [Dissertation Abstracts International]OH, USAThe Ohio State University3720064755B
- AmicoKRToro-AlfonsoJFisherJDAn empirical test of the information, motivation and behavioral skills model of antiretroviral therapy adherenceAIDS Care200517666167316036253
- StaraceFMassaAAmicoKRFisherJDAdherence to antiretroviral therapy: an empirical test of the information-motivation-behavioral skills modelHealth Psychol200625215316216569106
- JimmyBJoseJPatient medication adherence: measures in daily practiceOman Med J201126315515922043406
- SiminoffLAIncorporating patient and family preferences into evidence-based medicineBMC Med Inform Decis Mak201313Suppl 3S6
- FisherEBBoothroydRICoufalMMPeer support for self-management of diabetes improved outcomes in international settingsHealth Aff (Millwood)201231113013922232103
- MoskowitzDThomDHHesslerDGhorobABodenheimerTPeer coaching to improve diabetes management: which patients benefit most?J Gen Intern Med201328793894223404203
