Abstract
Background
Insulin analogs are regarded as more convenient to use than human insulin; however, they require a different administration scheme due to their unique pharmacokinetic and pharmacodynamic properties. This study aimed to assess difficulties with adherence to treatment with insulin analogs in patients with type 2 diabetes mellitus (T2DM), who had previously been treated with human insulin. The associations between difficulties with adherence and clinical, demographic, and psychological characteristics were also evaluated.
Patients and methods
The study was conducted on 3,467 consecutively enrolled patients with T2DM (54.4% women), mean age 63.9 years (SD =9.57), who had recently undergone a physician-directed change in treatment from human insulin to insulin analogs. The questionnaires addressed difficulties with switching the therapy, coping styles, well-being, and perception of self-influence on the disease.
Results
No adherence problems in switching therapy were reported in 56.6% of patients. Specific moderate difficulties were reported in 10.4%–22.1% of patients, major difficulties in 0.7%–6.9% of patients, and very significant difficulties in 0.03%–1.3% of patients. Overall, remembering to modify the insulin dose in the case of additional meals was the most frequently reported difficulty, and problems with identifying hypoglycemic symptoms were the least frequently reported. The increased risk of difficulties was moderately related to low perception of self-influence on diabetes and poor well-being. The intensity of problems was higher among those who were less-educated, lived in rural areas, had complications, and/or reported maladaptive coping styles.
Conclusion
Switching from human insulin to an insulin analog did not cause adherence problems in more than half of the patients. In the remaining patients, difficulties in adherence correlated with maladaptive coping styles, low perception of self-influence on disease course, and depressive symptoms.
Introduction
The World Health Organization (WHO) defines adherence as “the extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes – corresponds with agreed recommendations from a health care provider”.Citation1 Patient adherence is a derivative of educational initiatives provided by medical staff, but the influence of a patient’s psychosocial profile cannot be overlooked.Citation2 Indeed, the biopsychosocial model of glycemic control in diabetes includes relationships among stress, coping, and regimen adherence.Citation3 Furthermore, the model indicates that the coping style employed in response to diabetes depends on the perceived degree of control over the disease. KokoszkaCitation4 and Kokoszka et al,Citation5 introduced this concept of perception of self-influence on the disease and defined it as “the extent of belief about one’s own abilities to shape the disease course”. While the psychosocial problems and barriers related to diabetes mellitus management have been studied extensively, there is scarce information on adherence problems that occur when switching from human biphasic insulin to biphasic insulin analogs. This switch in therapy requires changes in the administration scheme due to significant differences in the pharmacodynamic and pharmacokinetic profiles between human insulin and insulin analogs. Little is also known about the factors influencing patient adherence during the change in therapy.
The aim of the present study was to assess difficulties with adherence to insulin analogs in patients with type 2 diabetes mellitus (T2DM) previously treated with human insulin. The associations between difficulties with adherence and clinical, demographic, and psychological data (including well-being, coping style, and perception of self-influence on the disease) were examined.
Patients and methods
In this observational study, 343 physicians from Poland enrolled consecutive patients with T2DM, who were switched from human biphasic insulin to an analog of biphasic insulin. Diabetes was diagnosed according to the Diabetes Poland guidelines published in 2010, ie, symptoms of hyperglycemia and random blood glucose concentration ≥200 mg/dL (≥11.1 mmol/L) or fasting glucose ≥126 mg/dL (≥7.0 mmol/L, based on two measurements on separate occasions) or blood glucose at 120 minutes during an oral glucose tolerance test (OGTT) ≥200 mg/dL (≥11.1 mmol/L).Citation6 The patients were selected using the code for diabetes (E11) of the International Statistical Classification of Diseases and Related Health Problems (ICD-10).Citation7 The decision to change treatment was at the discretion of treating physicians; it was separated from patients’ enrollment to the study and was based on the individual patient’s clinical needs. The implemented therapy was treatment with either a biphasic insulin analog only (conventional insulin therapy) or a biphasic insulin analog in combination with a rapid-acting insulin analog (conventional intensified insulin therapy). The inclusion criteria were age >30 years, treatment with biphasic insulin, and change in therapy from human insulin to insulin analog 7–61 days prior to the visit during which the questionnaire was completed.
All patients completed the following assessments during their visit (completed by the physician and/or the patient):
Physician questionnaire – developed for the purpose of the study to collect patient demographic and auxological information, data on the history of diabetes, current metabolic control, and treatment with insulin analogs. Body mass index (BMI) was calculated based on height and weight data extracted from patient medical files.
Questionnaire on possible difficulties at the time of switch from human insulin to insulin analogs () – a set of five questions about the level of difficulty in implementing treatment with insulin analogs. These five specific problems were identified based on the patient reports provided by treating clinicians. Each of the possible responses (five-point Likert scale: no problem, insignificant problem, moderate problem, major problem, and very significant problem) corresponded to a score of 0–4. The final score was calculated as the sum of ratings for all answers. The scale showed high reliability (Cronbach’s alpha =0.83), and all items correlated highly with the scale (from 0.6 to 0.7). The questionnaire also contained information on the frequency of adherence errors (having a snack between main meals, injecting a biphasic insulin analog much earlier before a meal, forgetting about changing the analog biphasic insulin dose after eating a snack, and experiencing hypoglycemia). The frequency of errors was reported since the patient’s previous visit, using the five-point Likert scale (never, once, a few times, up to five times, and more than five times). For the purpose of the analysis, the data were dichotomized as one to five times and more than five times.
The coping styles were assessed using two questions related to health and social problems from the Brief Method of Evaluating Coping with Disease.Citation5,Citation8 The full version of the questionnaire includes descriptions of four stressful situations (related to health, social, financial, and interpersonal problems); however, for the purpose of this study, only questions related to health and social problems were used. Based on the responses, the patient’s coping style was determined as either task-oriented, best solution-oriented, emotion-oriented, avoidance-oriented, or a combination of the aforementioned styles.
WHO-5 well-being index – initially used for the diagnosis of depression in the general elderly population.Citation9 Recently, it has been validated as a screening tool for depression in patients with diabetes.Citation10 The questionnaire contains five positive statements about well-being, and patients indicate on the scale (0 [at no time] to 5 [all of time]) for how long over the preceding 2 weeks he/she has been feeling this way. The score is a sum of individual responses, where 0 represents the worst and 25 the best well-being. Patients with a total score of <13 points or those who answered 0 or 1 to any of the five items need further diagnosis. According to more recent guidelines, a total score of <7 points suggests a high probability of depression.Citation11 This tool has adequate internal and external reliability. The questionnaire proved to be sufficiently homogenous (Loevinger’s coefficient 0.47; Mokken’s coefficient >0.3 in nearly all elements).Citation9 In the present study, the Polish version of the index, available on the WHO website, was used.Citation12 The index reliability evaluated on the basis of the trial turned out to be high (Cronbach’s alpha coefficient 0.877).
Assessment of perception of self-influence on the disease course was performed by the physician using the Likert scale based on criteria for the assessment of the validity of the “Brief measure to assess perception of self-influence on the disease course. Version for diabetes”.Citation4,Citation5 The score ranged from 0 to 4, with 0 indicating the lowest and 4 the highest influence on the disease course.
Ethical statement
The study was approved by the Bioethics Committee of the Medical University of Warsaw. All patients were provided with oral and written information about the study, before signing an informed consent form.
Statistical analysis
The SPSS statistical package (version 17) was used for all data analyses. The normality of the distribution of variables was tested using two tests: the Kolmogorov–Smirnov test and the Shapiro–Wilk test. As the data were not normally distributed, nonparametric tests were applied. To compare differences in the severity of difficulties with adherence to the therapy among groups with differing levels of education, place of residence, or BMI, the chi-square test was used for nominal variables, while the Mann–Whitney U test and the Kruskal–Wallis H test were used for ordinal variables. The Kruskal–Wallis H test (including the chi-square test) is a rank-based nonparametric test that can be used to determine if there are statistically significant differences between two or more groups of an independent variable on a continuous or ordinal dependent variable. It is considered the nonparametric alternative to the one-way analysis of variance to allow the comparison of more than two independent groups. To assess correlations between severity of the difficulties and variables such as age and BMI, the Spearman’s rank correlation coefficient was calculated. The Spearman’s rho correlation coefficient is the non-parametric equivalent of Pearson’s r coefficient. A significance level of 0.05 was used in all tests. To minimize the probability of misclassification of data originating from patients with type 1 diabetes mellitus, only patients ≥30 years of age were included in the analysis dataset.
Results
In total, 4,041 sets of completed questionnaires were collected. Among the included patients, 91.2% started treatment with insulin analogs 7–61 days before inclusion into the study (mean =21.0; SD =9.23 days). After excluding patients younger than 30 years, 3,467 patients were included in the analysis.
Characteristics of the studied group
The sample consisted of 1,887 (54.4%) women and 1,580 (45.6%) men. The age of the patients ranged from 32 to 93 years (mean =63.9; SD =9.57 years), height from 1.46 to 1.97 m (mean =1.7; SD =0.86 m), and weight from 41 to 182 kg (mean =82.8; SD =13.35 kg). In total, 25.2% of patients reported “village” as their place of residence, 40.2% reported “town”, and 34.6% reported “city”. Regarding education, 35.5% of patients reported they had basic education, 52.6% reported secondary education, and 11.9% reported that they had completed a university degree. The mean duration of T2DM was 10.2 (SD =6.17) years, and the mean duration of the previous therapy with human insulin was 4.8 (SD =3.72) years. The following long-term diabetes complications were reported: macroangiopathy in 1,519 patients (43.8%), retinopathy in 1,136 (32.8%), neuropathy in 892 (25.7%), and nephropathy in 360 (10.4%).
Difficulties related to changing treatments from human insulin to an insulin analog
Switching from human insulin to a biphasic insulin analog posed no difficulties in adherence for more than half of the patients (56.6%). Whereas, major and very significant problems with adherence to modified therapy were reported by 1.3% and 0.1% of patients, respectively. The most frequently reported difficulties (on each level of difficulty) were remembering to adjust the dose of the biphasic insulin analog in the case of an extra meal and skipping snacks between main meals. The data indicate that not needing to wait 30 minutes for a meal following injection was not a problem or at most a moderate problem for 99% of patients. Less than 2% of patients reported difficulties with identifying hypoglycemic symptoms as major or very significant. The details are presented in .
Table 1 Level of difficulty caused by a switch from human biphasic insulin to a biphasic insulin analog as experienced by patients
The patient-reported difficulties in adherence to the therapy were reflected in the frequency of adherence errors defined in the Questionnaire on possible difficulties at the time of switch from human insulin to insulin analogs. The most common lack of adherence was snacking between meals, and the least common was hypoglycemia ().
Table 2 Frequency of adherence errors after changing from human biphasic insulin to a biphasic insulin analog reported by the patients
Severity of difficulties in adherence was positively correlated with age (rho =0.11; P<0.001), with the level of education (chi-square =92.73; df=2; P=0.0001), and with the place of residence (P=0.0001) but was not related to gender. With regard to education, patients who had completed a higher level of education reported fewer problems, and those with only a basic level of education reported the most severe difficulties. The more significant difficulties in adherence were seen in patients dwelling in rural areas than those who resided in big cities. Furthermore, small but statistically significant correlations were observed between the severity of difficulties and HbA1c (data not shown).
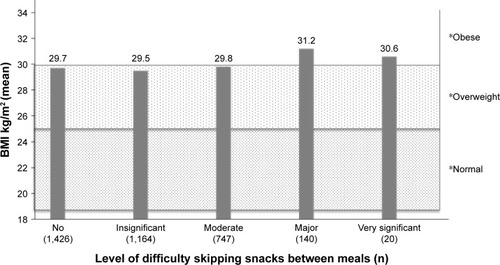
Impact of BMI
The mean BMI in the study population was 29.7 kg/m2 (SD =4.45). Differences in mean BMI between patient subgroups stratified by the degree of difficulty in skipping snacks between main meals were observed (P=0.0001; ), with greater problems reported by patients with a higher BMI than by those with lower BMI.
Coping styles
In the studied population, the most common coping style was the mixed/undifferentiated style (26.9%), and the least common was an emotion-oriented style (9.1%). The greatest difficulties (mean rank of difficulties in adherence) were observed in patients who used an emotion-oriented coping strategy and the lowest in those who used an adaptive mixed coping style, specifically seeking the best solution and focused on task-oriented coping strategies (chi-square =159.87; P=0.000l). The detailed data are presented in .
Table 3 Difficulties in adherence to the therapy for persons with different coping styles (the severity of difficulties is presented as the value of mean rank)
Well-being and risk of depression
The mean WHO-5 scale score in the entire study population was 15.1 (SD =4.77). A result of <13 points or an answer of 0 to 1 to any of the five items was noted for 913 patients (26.3%) and a result of <7 points on the WHO-5 scale was recorded for 256 patients (7.4%).
A negative correlation between the results of the WHO-5 scale and problems with adherence to therapy was observed (Spearman rho =−0.295; P<0.0001). A higher incidence of difficulties with adherence was reported by patients with low scores on the WHO-5 scale.
Perception of self-influence on the disease course
The mean score in the entire study population was 2.5 (SD =0.96). Severity of difficulties in adherence to the recommendations during treatment with insulin analogs was negatively correlated with the degree of the perception of self-influence on the course of the diabetes (Spearman rho =−0.295; P<0.01). A lower intensity of problems with adherence was observed in patients with a higher level of perception of self-influence on the course of the disease.
Discussion
In the present study, patient adherence following a physician-directed switch from human insulin to an insulin analog was evaluated. Modification of therapy is usually postponed both by patients and physicians because it is associated with a sacrifice of time and the need for additional education; however, in the present study more than half of the patients had no problem adjusting to the new regimen. This ease of transition is probably due to the good safety profile and simple dosage scheme of insulin analogs, which make them a more effective and convenient therapy in comparison with human insulin.Citation3,Citation13–Citation15 The results of the IMPROVE study indicate that intensifying the basal insulin (both human insulin and insulin analogs) regimens to the biphasic insulin regimen positively affects the outcomes of therapy. The authors observed improved glycemic control, reduced risk of hypoglycemia, no significant change in weight, and increased patient satisfaction after such change in the therapy.Citation16 These treatment benefits may result from better pharmacokinetic and pharmacodynamic properties of the biphasic insulin analog and the fact that it could be dosed immediately before or after a meal.Citation16–Citation18 In the present study, the most frequently reported, but not severe, difficulties were the need to adjust the dose of the biphasic insulin analog in the case of an extra meal and to forego snacking between main meals. Consequently, snacking between main meals and forgetting to adjust the insulin analog dose were the most frequent types of errors. We performed indirect analysis and assessment of the relationship between the level of difficulties in abstaining from the snacks and BMI. As expected, patients with higher BMI had greater problems with snacking between main meals than patients with normal weight. This finding may have clinical implications because higher basal BMI is a negative predictor of success in diabetes treatment,Citation19 and obesity is associated with worsened glycemic control in patients with T2DM treated with insulin.Citation20
Glycemic control influenced by adherence is dependent on many factors, including patient coping strategies.Citation3 Previous work has proven that positive coping styles (more approach-oriented and those focused on dealing with the stressor itself) are associated with better glycemic control.Citation3,Citation21–Citation23 Conversely, avoidant and emotional strategies (dealing with the emotional response to a stressor) are associated with adjustment problems and regimen nonadherence.Citation3,Citation21–Citation23 Similar observations were made in our study – the most severe difficulties were reported by patients with an emotion-oriented coping strategy and the lowest in those using an adaptive mixed strategy where they applied the best solution and task-oriented coping strategies. According to the psychological “goodness of fit” hypothesis, the coping mechanism is related to the controllability of a stressor.Citation24 When dealing with a controllable agent, people are more likely to use a problem-focused coping strategy,Citation24–Citation26 though a patient’s selection of coping style also depends on the severity and duration of disease, with the impact of patient experiences, including emotional and cognitive factors, influencing the decision.Citation23,Citation27 Nonetheless, any application of problem-solving strategies requires the perception of the possibility of gaining control over the stressful problem.
In turn, the perception of having control of the diabetes requires the perception of self-influence on the course of the disease. The concept of self-influence relates only to coping with the disease and so is consequently narrower than the perceived self-efficacy, which determines how a person feels, thinks, self-motivates, and behaves.Citation28 Hence, perception of self-influence is related to disease management and is therefore more precise.Citation5 In our study, a higher level of perception of self-influence on the course of the disease was related to a lower intensity of problems with adherence. Similarly, Sarkadi et alCitation29 observed that patients belonging to the “active” category of their self-perceived role in diabetes management have better outcomes compared to those having a “passive” attitude. Indeed, perceived control of diabetes was found to be a significant predictor of engagement in diabetes and desirable health behaviors that strongly influence adherence to the therapy.Citation30,Citation31
The presence of diabetes almost doubles the risk of comorbid depression. In turn, it is well documented that depression and low well-being are related to nonadherence to treatment,Citation32–Citation34 and patients with depression usually have poorer glycemic control.Citation35 As ~30% of patients with diabetes have depressive symptoms and ~12%–18% meet the criteria of major depression,Citation36,Citation37 it is a serious problem. A similar relationship was observed in the present study: patients who received a low score on the WHO-5 scale, an indicator for depression, had worse adherence, as measured by mean higher incidences of difficulties with the therapy. Our results indicate that there is a need for screening for depression symptoms in patients with diabetes and that treating depression may enhance diabetes control by improving patient adherence.
Study limitations
As the present study relies on patient-reported data, it is important to remember that the time elapsed from the implementation of insulin analog to the time of this study varied widely from patient to patient. For this reason, it is possible that patients who started insulin analog therapy earlier might not have recalled all the initial difficulties as easily as those who had started treatment more recently. Furthermore, a certain degree of selection bias may impact the results. The study population consisted of consecutive patients switching therapy and not consecutive patients on human insulin. Therefore, patients who accepted this new therapy were likely expecting to benefit from the switch and, therefore, showed strong adherence. The author also acknowledges that the psychological measures used in the present study do not have strong psychometric proprieties; however, they are useful, commonly used tools applied by the physician during a regular medical visit. In summary, these results should be interpreted with caution, keeping in mind the limitations discussed earlier and also those inherent to the nature of observational studies, such as recall bias, missing data, and sporadically observed lower data quality.
Conclusion
Overall, switching from human biphasic insulin to bipha-sic insulin analogs did not cause significant problems in adherence for the majority of patients. However, a subset of patients did report difficulties with treatment adherence, typically those who presented with emotion-oriented coping strategies, low perception of self-influence on disease, or depressive symptoms. It is therefore reasonable to suggest that the approach to treatment of diabetic patients should be biopsychosocial rather than simply biomedical.
Acknowledgments
The author would like to acknowledge Rafał Radzio, PhD from SWPS University of Social Sciences and Humanities, for help in statistical analysis, and Proper Medical Writing Sp. z o.o., in particular Karolina Beda-Maluga, PhD, and Maria Kołtowska-Häggström, MD, PhD, for their help in editing and structuring the paper, and Ashley Cooper, BSc (Hons 1)/BJ for linguistic corrections of the manuscript. The study and the paper preparation were fully sponsored by a grant from Novo Nordisk Poland; the grant was given to the Foundation for the Development of Psychiatry and Psychotherapy.
Supplementary material
Table S1 Questionnaire on possible difficulties at the time of switch from human insulin to insulin analogs (completed by the physician and the patient)
Any change in treatment may present potential challenges for patients. A switch from human insulins to insulin analogs may also pose such risk. Therefore, I am asking you to assess whether – and if so to what extent – this change in treatment makes a problem in the context of the following issues. Please, rate, whether each of the problems mentioned in the following questions caused: no problem, insignificant problem, moderate problem, major problem, or very significant problem.
You may find answering these questions easier if you look at the questionnaire together with me.
Disclosure
AK, as a principal investigator of the study received honorarium from the Foundation for Development Psychiatry and Psychotherapy.
Novo Nordisk Poland sponsored participation of AK in meetings of Psychosocial Aspects of Diabetes (PSAD) Study Group an official Study Group of the European Association for the Study of Diabetes (EASD).
References
- SabateEAdherence to Long-Term Therapies: Evidence for ActionGenevaWHO2003
- CampbellRKRecommendations for improving adherence to type 2 diabetes mellitus therapy–focus on optimizing insulin-based therapyAm J Manag Care2012183 supplS55S6122558943
- PeyrotMMcMurryJFJrKrugerDFA biopsychosocial model of glycemic control in diabetes: stress, coping and regimen adherenceJ Health Soc Behav199940214115810467761
- KokoszkaAKrótka metoda oceny poczucia wpływu na przebieg choroby: opis wersji dla osób z cukrzycą [Brief measure to assess perception of self-influence on the disease course. Version for diabetes]Przegl Lek200562874274516521488
- KokoszkaAJodko-ModlińskaAObrębskM[webpage on the Internet]Psychodiabetic kit and its application in clinical practice and researchMasuoKType 2 Diabetes Available from: http://www.intechopen.com/books/type-2-diabetes/psychodiabetic-kit-and-its-application-in-clinical-practice-and-researchAccessed September 18, 2010
- Polish Diabetes AssociationClinical recommendations for the management of patients with diabetesClin Diabetol20105suppl AA1A76
- ICD10Data.com [webpage on the Internet]ICD-10-CM Diagnosis Code Available from: http://www.icd10data.com/ICD10CM/Codes/E00-E89/E08-E13/E11-/E11Accessed November 12, 2016
- KokoszkaARadzioRKotWBrief method of evaluating coping with disease: versions for men and womenDiabet Prakt20089111
- BonsignoreMBarkowKJessenFHeunRValidity of the five-item WHO Well-Being Index (WHO-5) in an elderly populationEur Arch Psychiatry Clin Neurosci2001251suppl 2II27II3111824831
- HajosTRPouwerFSkovlundSEPsychometric and screening properties of the WHO-5 well-being index in adult outpatients with Type 1 or Type 2 diabetes mellitusDiabet Med2013302e63e6923072401
- SnoekFJKerschNYEldrupEMonitoring of individual needs in diabetes (MIND): baseline data from the cross-national diabetes attitudes, wishes, and needs (DAWN) MIND studyDiabetes Care201134360160321266654
- Psychiatric Research Unit, WHO Collaborating Centre in Mental HealthWHO-5 Questionnaires Available from: http://www.psykiatri-regionh.dk/who-5/Documents/WHO5_Polish.pdfAccessed September 20, 2010
- BoehmBOVazJABrondstedLHomePDLong-term efficacy and safety of biphasic insulin aspart in patients with type 2 diabetesEur J Intern Med200415849650215668084
- McNallyPGDeanJDMorrisADWilkinsonPDCompionGHellerSRUsing continuous glucose monitoring to measure the frequency of low glucose values when using biphasic insulin aspart 30 compared with biphasic human insulin 30: a double-blind crossover study in individuals with type 2 diabetesDiabetes Care20073051044104817277042
- WolnikBLukaszewiczMTreatment intensification with insulin analogs in type 2 diabeticsDiabet Prakt20089209219
- GumprechtJBenroubiMBorziVIntensification to biphasic insulin aspart 30/70 (BIAsp 30, NovoMix 30) can improve glycaemic control in patients treated with basal insulins: a subgroup analysis of the IMPROVE observational studyInt J Clin Pract200963696697219504715
- HermansenKColomboMStorgaardHOstergaardAKolendorfKMadsbadSImproved postprandial glycemic control with biphasic insulin aspart relative to biphasic insulin lispro and biphasic human insulin in patients with type 2 diabetesDiabetes Care200225588388811978685
- JacobsenLVSogaardBRiisAPharmacokinetics and pharmacodynamics of a premixed formulation of soluble and protamine-retarded insulin aspartEur J Clin Pharmacol200056539940311009049
- da VicoLMonamiMBiffiBTargeting educational therapy for type 2 diabetes: identification of predictors of therapeutic successActa Diabetol201350330931722350098
- WatsonLWilsonBPAlsopJKumarSWeight and glycaemic control in type 2 diabetes: what is the outcome of insulin initiation?Diabetes Obes Metab201113982383121481128
- Garay-SevillaMEPorrasJSMalacaraJMCoping strategies and adherence to treatment in patients with type 2 diabetes mellitusRev Invest Clin201163215516121714436
- KarlsenBIdsoeTHanestadBRMurbergTBruEPerceptions of support, diabetes-related coping and psychological well-being in adults with type 1 and type 2 diabetesPsychol Health Med200495370
- WilloughbyDFKeeCCDemiAParkerVCoping and psychosocial adjustment of women with diabetesDiabetes Educ200026110511210776102
- LazarusRSFolkmanSStress, Appraisal and CopingNew York, NYSpringer1984
- MacrodimitrisSDEndlerNSCoping, control, and adjustment in Type 2 diabetesHealth Psychol200120320821611403218
- ZeidnerMSaklofskeDHAdaptive and maladaptive copingZeidnerMEndlerNSHandbook of Coping: Theory, Research and ApplicationsNew York, NYWiley1996505531
- AljasemLIPeyrotMWissowLRubinRRThe impact of barriers and self-efficacy on self-care behaviors in type 2 diabetesDiabetes Educ200127339340411912800
- BanduraASelf-efficacyRamachaudranVSEncyclopedia of Human Behavior4New York, NYAcademic Press19947181
- SarkadiAVegARosenqvistUThe influence of participant’s self-perceived role on metabolic outcomes in a diabetes group education programPatient Educ Couns200558213714516009289
- RubinRRPeyrotMQuality of life and diabetesDiabetes Metab Res Rev199915320521810441043
- WatkinsKWConnellCMFitzgeraldJTKlemLHickeyTIngersoll-DaytonBEffect of adults’ self-regulation of diabetes on quality-of-life outcomesDiabetes Care200023101511151511023145
- CampayoAde JongePRoyJFDepressive disorder and incident diabetes mellitus: the effect of characteristics of depressionAm J Psychiatry2010167558058820123914
- DucatLPhilipsonLHAndersonBJThe mental health comorbidities of diabetesJAMA2014312769169225010529
- GonzalezJSPeyrotMMcCarlLADepression and diabetes treatment nonadherence: a meta-analysisDiabetes Care200831122398240319033420
- LustmanPJAndersonRJFreedlandKEde GrootMCarneyRMClouseREDepression and poor glycemic control: a meta-analytic review of the literatureDiabetes Care200023793494210895843
- AndersonRJFreedlandKEClouseRELustmanPJThe prevalence of comorbid depression in adults with diabetes: a meta-analysisDiabetes Care20012461069107811375373
- LiCFordESStrineTWMokdadAHPrevalence of depression among U.S. adults with diabetes: findings from the 2006 behavioral risk factor surveillance systemDiabetes Care200831110510717934145