Abstract
Medication adherence is an important challenge while treating chronic illnesses, such as ulcerative colitis (UC), that require a long-term management to induce and maintain clinical remission. This review provides an overview of the role that medication adherence plays in the routine management of UC, with a focus on the results of a recent Italian study reporting the perception of patients with UC regarding adherence to treatment. A literature analysis was conducted on topics, such as measurement of adherence in real practice, causes, risk factors and consequences of non-adherence and strategies, to raise patients’ adherence. Most of the data refer to adherence to 5-aminosalicylic acid, and standard of care for the induction and maintenance of remission in UC. The adherence rate to 5-aminosalicylic acid is low in clinical practice, thus resulting in fivefold higher risk of relapse, likely increased risk of colorectal cancer, reduced quality of life and higher health care costs for in- and outpatient settings. There are various causes affecting non-adherence to therapy: forgetfulness, high cost of drugs, lack of understanding of the drug regimen – which are sometimes due to insufficient explanation by the specialist – anxiety created by possible adverse events, lack of confidence in physicians’ judgment and complex dosing regimen. The last aspect negatively influences adherence to medication both in clinical trial settings and in real-world practice. Regarding this feature, mesalamine in once-daily dosage may be preferable to medications with multiple doses per day because the simplification of treatment regimens improves adherence.
Introduction
Medication adherence is an important challenge in the treatment of chronic illnesses, such as ulcerative colitis (UC), that require a long-term management to induce and maintain clinical remission. Indeed, the course of this disease is generally marked by the alternance of periods of quiescence and symptomatic relapses, which sometimes need hospitalization.Citation1,Citation2
The World Health Organization (WHO) recognizes that adherence in chronic diseases is one of the key factors that contribute to the efficient use of therapies.Citation3 The success of a therapy does not only depend on correct diagnosis and choice of treatment by the physician but also patient’s adherence to therapy is critical, as well as their ability to follow the instructions given during the therapy course. Non-adherence may impact the effectiveness of a cure and determine the worsening of health conditions, the need of examinations or implementation of drugs, and the increase in morbidity and mortality.Citation4–Citation6
According to the WHO definition, the term “adherence” is the extent to which a person’s behavior – taking medication, following a diet and/or executing lifestyle changes – corresponds to agreed recommendations from a health care provider.Citation7,Citation8
In routine clinical practice, therapeutic adherence plays a critical role in the management of UC; therefore, the decision-making process should also include a thorough assessment of risk factors associated with non-adherence, and of patients’ concerns and beliefs.
Physicians have to consider patients’ judgment of their personal need for therapy and their concerns about treatment can be a significant barrier to adherence.Citation9–Citation11 In this setting, interventions should be considered to facilitate adherence to medical treatment among inflammatory bowel disease (IBD) subjects in order to overcome such perceptual barriers.
This non-systematic review provides an overview of the role of medication adherence in the routine management of UC, with a focus on the results of a recent Italian study reporting the perception of patients with UC regarding adherence to treatment. For this purpose, we performed a Medline search for full publications, using the search terms “adherence”, “adherence and ulcerative colitis”, “adherence and inflammatory bowel disease” and “adherence and 5-ASA”. We included only those citations that discussed the impact of adherence on UC.
Burden and measuring adherence in real practice
Most of the data in the literature refer to adherence to 5-aminosalicylic acid (5-ASA), and the standard of care for the induction and maintenance of remission in UC. Different adherence rates were reported according to the study setting in UC patients treated with 5-ASA, also known as mesalamine,Citation4 commonly considered the first-line treatment of mild-to-moderate disease.Citation12
Adherence levels are much lower in community-based studiesCitation13,Citation14 than in clinical trialsCitation15,Citation16 (40%–60% vs more than 80%), in which participants are generally closely observed and monitored.
In a cohort study of 92 patients with clinically inactive disease who were followed up for more than 48 weeks with appointments occurring every 12 weeks, only 43% of patients were found to be 100% adherent.Citation17 A study that involved 94 UC patients in remission, examining their prescription refill information as a measure of adherence, showed that only 40% of patients were adherent, and the median amount of medication consumed was 71% of the prescribed dose.Citation14 A recent European online survey conducted across six countries showed that 60% of patients with UC (from a total of 372 respondents) had a low adherence based on the Morisky scale, and that only 7% of them had high adherence.Citation18
Low adherence, noticed in the real-world setting, could attenuate benefits of 5-ASA therapy, affect the clinical course of UC and lead to poorer long-term outcomes, with a considerable impact on patients’ quality of life and significant additional costs to society in terms of increased utilization of health care services.Citation14
There are several ways to measure adherence; however, there is not an accepted standard method and it is important to estimate correctly. Direct methods of assessment, including the patient’s observation and the measurement of drug levels or metabolites in blood or urine, are the most accurate ways of estimating medication consumption both in controlled clinical trials and in real clinical practice, even if the tests are not always available. Alternative methods include patient self-report (patient interviews or self-report surveys), the use of electronic monitoring systems of prescription claims or refill history and pill counts.Citation2,Citation19–Citation21
Non-adherence: cause and risk factors
The WHO classifies the determinants of non-adherence to medical plans into five dimensions: social and economical, health system-related, therapy-related, condition-related and patient-related.Citation7,Citation22
In UC, neither clinical nor community studies have consistently identified the same groups of patients as being at high risk for poor adherence.Citation23 Nonetheless, in several studies the factors that appear to affect adherence include younger age, single status, heavy pill burden, perception of lack of benefit and shortage of information about the effect of medication.Citation24
The Manitoba Inflammatory Bowel Disease Cohort Study showed how men with UC were significantly more likely to have poor adherence than those with Crohn’s disease (odds ratio [OR] 4.42, 95% confidence interval [CI]: 1.66–11.75), and that age was a predictive factor for adherence in women: younger women were less adherent than older women (under 30 vs over 50 years: OR 3.64, 95% CI: 1.41–9.43; under 30 vs 40–49 years: OR 2.62, 95% CI: 1.07–6.42).Citation25
Kane et al showed that males were twice as likely as females to be non-adherent with their UC treatment;Citation14,Citation26 in particular, younger men were the least adherent.Citation23,Citation27
Adherence rates are particularly low among patients in symptomatic remission because of the fact that some of them are unable to express their need for medication during periods of symptoms’ quiescence.Citation26,Citation28 In this condition, rather than continuing with the prescribed regimen, patients often forget to take their drugs at the scheduled time; Kane suggested that this forgetfulness may be linked to a form of disease denial: they are in remission and do not wish to be reminded that they have a disease when they feel well.Citation23
In this case, the physician should reassure and instruct the patient on the importance of a continued therapy even in periods of well-being in order to prevent exacerbations.
Lack of medical supervision, concomitant medications, side effects and cost of prescriptions were frequent reasons for treatment non-adherence cited by patients in a North American study.Citation4 However, the most cited factor was the inconvenient dosage schedule of 5-ASA medications, which required a large number of tablets per day.Citation4
Other factors contributing to poor adherence were related to the drugs: the cost (reported by 25% of patients), the concept of therapy as a reminder of illness (13%), the undesirable side effects (13%) and the lack of belief in the effectiveness of the medication (12%).Citation25
The complexity of administration regimen could have a relevant impact on patients’ adherence. Inconvenient and intrusive drug delivery formulations (eg, rectal therapies), pill burden and multiple-daily dosing of oral medications have been shown to be associated with poor levels of therapeutic adherence.Citation4 A literature review conducted by Greenberg has shown that once-daily and twice-daily dosing regimens significantly improve adherence rates (73% and 70%, respectively) than three-times (52%) and four-times-daily dosing (42%) regimensCitation29 Shale and Riley’s studyCitation13 demonstrated that three-times-daily dosing and full-time employment were independent predictors of partial non-adherence in patients taking delayed-release mesalamine.
An Italian studyCitation15 confirmed all these results: non- adherence was significantly associated with age less than 40 years (43% vs 34%, P=0.041) and the most common reasons for non-adherence versus adherence were as follows: forgetfulness (61% vs 44%, P<0.001), disease remission (25% vs 10%, P<0.001), recent diagnosis (24% vs 15%, P<0.001) and full-time employment (55% vs 26%, P<0.001). Topical therapy with enemas was associated with significantly more non-adherence (68% of users) than oral therapy (40% of users; P=0.001, OR 0.25, CI: 0.11–0.60). Moreover, a significant interaction was found for adherence and patients <40 years who had a good relationship with their doctors. Therefore, good communication with the physician might improve adherence.
Many patients with IBD deliberately decide to stop treatment. A Spanish study on 40 IBD patients has shown that up to 35% of patients are intentionally non-adherent compared with 67% who are unintentionally non-adherent.Citation30 A greater association was found between patients who are intentionally non-adherent and patients who had high depression scores, in patients with long-standing IBD, subjects with high patient–physician discordance and patients who did not consider themselves to be adequately informed about their treatment.Citation30
In , we have summarized the principle causes of non-adherence.
Table 1 Factors of non-adherence in UC
Consequences of non-adherence
The clinical outcomes of non-adherence can be harmful to patients.
In a cohort of 99 patients with UC in remission, Kane et al prospectively measured clinical outcomes. Non-adherent patients experienced more than a fivefold increased risk of disease relapse compared to those who were adherent (hazard ratio 5.5, 95% CI: 2.3–13, P<0.001).Citation27
In the same way, in a retrospective study, Robinson et al showed that non-adherent subjects had a significantly greater risk of relapse than adherent patients (relative risk =1.44, 95% CI =1.08–1.94; P=0.014).Citation31
Moreover, Moody et al showed a correlation between non-adherence to or discontinuation of sulfasalazine therapy and increased risk of colon cancer; 5 of 152 adherent patients and 5 of 16 non-adherent patients developed colorectal cancer (P<0.001).Citation32 This finding was supported by Eaden et al, who showed in a case-controlled study among 102 cases of colorectal cancer with UC that the risk of colorectal cancer was reduced by 81% in patients receiving regular mesalamine therapy (≥1.2 g/day) compared with those receiving no treatment (P=0.006).Citation33
In addition, poor adherence was associated with a two-to threefold increase in costs for non-hospitalized cases and a 20-fold increase in costs for hospitalized cases compared to quiescent cases of IBD.Citation33 In this study, conducted in the United Kingdom, the authors showed that patients’ costs ranged from £73 to £33.254, with a mean 6-month cost of £1.256 (95% CI: £988, £1.721) per UC subject.Citation34
Strategies to raise patients’ adherence
Patients’ decision to not take medication is a common issue that physicians may not fully understand because many subjects are reluctant to discuss or to give accurate representations of their adherence levels.Citation19 The simplest and most practical suggestion for physicians is to ask patients non-judgmentally how often they miss doses. Patients usually want to please their physicians, so that they say what they think their doctor wants to hear. It can be reassuring to the patient when the physician tells them, “I know it must be difficult to take all your medications regularly. How often do you miss taking them?” This approach makes most patients feel comfortable in telling the truth and facilitates the identification of poor adherence.Citation8
According to some studies, pill burden and multiple-daily dose administration are often associated with non-adherence, and formulations that require less frequent and/or fewer doses may improve patients’ adherence.Citation21 A recent systemic review of interventions to enhance adherence to medications in chronic illnesses found that the only consistent success rates have been with those that aim to simplify dose administration regimen.Citation35 Furthermore, data from an interactive survey of patients with UC showed that, from patients’ perspective, an ideal therapy would have less frequent dosing regimen.Citation36
As stated earlier, once-daily and twice-daily dosing lead to better medication adherence rates than three- or four-times-daily dosing regimens.Citation29
In order to demonstrate improved adherence with a smaller pill burden, a pilot study compared once-daily with conventional dosing of mesalamine.Citation37
The authors observed a significant difference in patients’ adherence between once-daily versus conventional dosing of the drug (respectively, 100% vs 70%): once-daily dosing had the same rate of disease relapse as the conventional dosing group. When a phase III clinical trial demonstrated that once-daily MMX® mesalamine, a new formulation characterized by a polymeric matrix, was effective in inducing remission of active UC, it provided hope that this regimen might also be effective in maintaining disease quiescence: this would combine the benefits of clinical efficacy and ease of use for long-term therapy. The study showed that 96% of patients enrolled were adherent to their medication regimen, as they took more than 80% of their prescribed medication.Citation38
Lachaine et al also reported that the proportion of adherent patients was significantly higher with once-daily mesalamine delayed/extended-release tablets than with any other oral treatments (P<0.001). Therefore, they suggested that
a once daily oral treatment with an extended drug release could be a therapeutic option to improve adherence in UC patients and then to maintain therapy leading to better outcomes and to prevent relapses and complications.Citation26
In the same way, in a randomized trial of maintenance therapy with mesalamine granules 2 g/day in 362 patients, the remission rate after 1 year was significantly higher in the group receiving a single daily dose than in the one receiving 1 g twice daily (74% vs 64%, P=0.024). There was evidence from patients’ questionnaires that adherence was higher in the once-daily group, and this may, in part, explain the unexpected difference, as the trial was designed to show non-inferiority of the once-daily regimen.Citation39
Recently, a meta-analysis evaluated the efficacy, safety and adherence to once-daily and multiple-daily dosing of mesalamine for the induction and the maintenance of remission in mild-to-moderate UC.Citation40 With respect to adherence, no difference was noted between the two doses of 5-ASA.
Another cause of non-adherence is the use of topical therapy; patients often do not accept enemas, which represent the standard of care in case of involvement of the distal colon.Citation12 D’Incà et al showed that topical therapy with foams, suppositories or enemas, is more likely to be associated with non-adherence than oral therapyCitation15 because of discomfort during treatment (68% vs 40%, P=0.001, OR 0.25, CI: 0.11–0.60). A preliminary multicenter trial in patients with left-sided active UC showed that 5-ASA MMX® was comparable to the 5-ASA enema in inducing remission after 8 weeks of treatment (60% vs 50%; 95% CI for the difference, −12 to +32), with a compliance of 97% for oral and 87.5% for topical therapy.Citation16 The authors themselves suggested the need of a larger multicentric trial to confirm these results.
Moreover, in order to improve adherence, some authors use web-based follow-up and patients’ education, considering that the majority of subjects are young.Citation41–Citation43
Pedersen et al studied for 3 months 95 patients with UC receiving mesalamine therapy.Citation41 Once a week, patients registered fecal calprotectin on a web application and completed the simple clinical colitis activity index. A total of 82 (86%) patients were adherent to web therapy, and from week 0 to week 12 subjects experienced clinical and biochemical improvement, thus allowing a reduction in mesalamine dosing due to improved adherence to treatment.
Elkjaer et al evaluated 333 patients with mild/moderate UC in Denmark and Ireland, subjected to treatment with 5-ASA, who were randomized to either a web-group receiving disease-specific education and self-treatment via web or a control group continuing the usual care for 12 months.Citation42 Adherence to 4 weeks of acute treatment was increased by 31% in Denmark and 44% in Ireland compared to the control groups. The number of acute and routine visits to the outpatient clinic was lower in the web than in the control group, resulting in a saving of 189 euro/patient/year.
Moshkovska et alCitation43 organized a tailored approach, consisting of motivational and educational components plus options including simplified dosing regimens and practical reminders, such as pill dispensers. Seventy-one people completed the study. At follow-up, adherence in subjects included in the “tailored” group was 44% greater than in the control group (76% vs 32%, P=0.001).
Patient perception of medication adherence
A recent Italian survey on medication adherence, published as abstract, involved more than 1,000 UC patients with the aim of evaluating the perception of patients with UC regarding adherence to treatment.Citation44
Patients from five regions of Italy (Campania, Lazio, Liguria, Lombardy and Piedmont) were surveyed with a 16 items questionnaire distributed by clinicians of Italian specialized centers. The questionnaire, not validated, consisted of two parts: the first regarding the characteristics of participants (age, sex, marital status and employment status) and the second concerning adherence of the patient to treatment (drugs, visits and family support). A total of 1,045 patients were recruited (male 54%), with a mean age of 48 years (range 5–90 years) and a median duration of disease of 8 years (50% <10 years and 35% <5 years). The extension of the disease was classified as proctitis in 14%, left-sided colitis in 51% and pancolitis in 34% of patients. At the time of compilation, 68% of patients were in remission; 50% of patients assumed mesalamine while 31% were treated with MMX® mesalamine.Citation44
A question was particularly relevant for the assessment of self-perceived adherence of the patients:
Numerous studies show that patients who need continued therapy sometimes do not take medications as prescribed. Is this also true in your case?
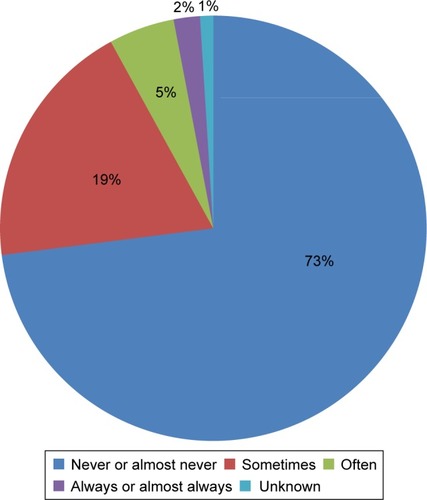
To this question, 73% replied that this “never or almost never” had been the case: the perception of the adequate intake of therapy was almost total, with 19% of patients who reported that it had occurred “sometimes”, 5% “often” and 2% “always or almost always” (). These adherence rates appear to be higher than those expected and reported by previous studies on patients’ adherence in UC.Citation4,Citation22,Citation45
About the type of formulation, the patients did not find any concerns in taking tablets (even if 13% of respondents declared not to take them because they were too busy at work); different attitudes emerged about enemas and suppositories. The main reason for non-adherence to therapy with enemas was “I feel uncomfortable” (29%). In particular, the percentage of this type of response was higher in the active phase of the disease (45%) compared to that of patients in remission (26%). The same applies to suppositories, even if with a lower percentage (about 20% of patients declared “I feel uncomfortable”).
According to the literature, the main reason for non-adherence to treatment, regardless of the formulation prescribed, remains forgetfulness (48%) followed by physical well-being (20%). In case of patients’ forgetfulness, partners have the function of caregivers and serve as reminder therapy, as shown in the study by Kane et al.Citation14
Summary
Even if in the absence of a validated way of assessing adherence, the percentage of adherence detected in this study was greater than those observed in other studies based on objective methods, such as the medication possession ratio.Citation4,Citation6
Conclusion
Adherence to therapy is a key factor in the treatment of chronic illnesses like UC, and most of the data in the literature refer to adherence to 5-ASA, and the standard of care for the induction and maintenance of remission in UC. Since adherence rates to this drug are higher in controlled trials and community setting, it is difficult to apply the data derived from multicentric studies into clinical practice. In the daily management of patients with UC, adherence is low, thus resulting in fivefold higher risk of relapse, reduced quality of life and higher health care costs for both in- and outpatient settings.Citation6,Citation23 For these reasons, the decision-making process should include a thorough assessment of risk factors associated with non-adherence and patients’ concerns, in order to ensure a proper and shared treatment.
According to patients’ judgment, the burden of a complex dosing regimen negatively influences adherence to medication. Therefore, even if in the absence of a strong literature, based on prospective studies in non-adherent patients, several educational (eg, verbal and written) as well as behavioral interventions (reminders, calendar blister packs and dosage implication) have been shown to improve adherence.
Disclosure
The survey was supported by an unrestricted grant of Takeda. The authors report no other conflicts of interest in this work.
References
- BernickSJKaneSOptimizing use of 5-ASA in the treatment of ulcerative colitis: focus on patient compliance and adherencePatient Relat Outcome Meas20101576322915953
- KhanNAbbasAMBazzanoLAKolevaYNKrousel-WoodMLong-term oral mesalazine adherence and the risk of disease flare in ulcerative colitis: nationwide 10-year retrospective cohort from the veterans affairs healthcare systemAliment Pharmacol Ther201236875576422882428
- SerupJLindbladAKMarotiMTo follow or not to follow dermatological treatment – a review of the literatureActa Derm Venereol200686319319716710573
- KaneSVSystematic review: adherence issues in the treatment of ulcerative colitisAliment Pharmacol Ther200623557758516480396
- HawthorneABRubinGGhoshSReview article: medication non-adherence in ulcerative colitis – strategies to improve adherence with mesalazine and other maintenance therapiesAliment Pharmacol Ther200827121157116618384664
- KaneSShayaFMedication non-adherence is associated with increased medical health care costsDig Dis Sci20085341020102417934828
- SabateEAdherence To Long-Term Therapies: Evidence For ActionGenevaWorld Health Organization2003 Available from: http://www.who.int/chp/knowledge/publications/adherence_report/en/Accessed August 25, 2016
- OsterbergLBlaschkeTAdherence to medicationN Engl J Med2005353548749716079372
- HorneRParhamRDriscollRRobinsonAPatients’ attitudes to medicines and adherence to maintenance treatment in inflammatory bowel diseaseInflamm Bowel Dis200915683784419107771
- KimSBKimKOJangBIDaegu-Gyeongbuk Gastrointestinal Study Group (DGSG)Patients’ beliefs and attitudes about their treatment for inflammatory bowel disease in KoreaJ Gastroenterol Hepatol201631357558026313162
- SelingerCPEadenJJonesDBModifiable factors associated with nonadherence to maintenance medication for inflammatory bowel diseaseInflamm Bowel Dis201319102199220623899547
- DignassALindsayJOSturmASecond European evidence-based consensus on the diagnosis and management of ulcerative colitis part 2: current managementJ Crohns Colitis2012610991103023040451
- ShaleMJRileySAStudies of compliance with delayed-release mesalazine therapy in patients with inflammatory bowel diseaseAliment Pharmacol Ther200318219119812869079
- KaneSVCohenRDAikensJEHanauerSBPrevalence of nonadherence with maintenance mesalamine in quiescent ulcerative colitisAm J Gastroenterol200196102929293311693328
- D’IncàRBertomoroPMazzoccoKVettoratoMGRumiatiRSturnioloGCRisk factors for non-adherence to medication in inflammatory bowel disease patientsAliment Pharmacol Ther200827216617217949472
- PranteraCViscidoABianconeLFrancavillaAGiglioLCampieriMA new oral delivery system for 5-ASA: preliminary clinical findings for MMxInflamm Bowel Dis200511542142715867580
- RileySAManiVGoodmanMJLucasSWhy do patients with ulcerative colitis relapse?Gut19903121791832311975
- VavrickaSHofmannRGuillaumeXPrevalence and reasons for drug non-adherence in a European cohort of ulcerative colitis patients: the UCandME surveyJ Crohns Colitis20159Suppl 1S327
- NeiheiselMBWheelerKJRobertsMEMedication adherence part one: understanding and assessing the problemJ Am Assoc Nurse Pract2014261495524382862
- LamWYFrescoPMedication adherence measures: an overviewBiomed Res Int2015201521704726539470
- LeeJKGraceKAFosterTGHow should we measure medication adherence in clinical trials and practice?Ther Clin Risk Manag20073468569018472991
- CostaEGiardiniASavinMInterventional tools to improve medication adherence: review of literaturePatient Prefer Adherence201591303131426396502
- KaneSVOvercoming adherence issues in ulcerative colitisGastroenterol Hepatol (N Y)200731079579921960790
- KaneSVStrategies to improve adherence and outcomes in patients with ulcerative colitisDrugs200868182601260919093702
- EdigerJPWalkerJRGraffLPredictors of medication adherence in inflammatory bowel diseaseAm J Gastroenterol200710271417142617437505
- LachaineJYenLBeaucheminCHodgkinsPMedication adherence and persistence in the treatment of Canadian ulcerative colitis patients: analyses with the RAMQ databaseBMC Gastroenterol2013132323363459
- KaneSHuoDAikensJHanauerSMedication nonadherence and the outcomes of patients with quiescent ulcerative colitisAm J Med20031141394312543288
- LevyRLFeldADIncreasing patient adherence to gastroenterology treatment and prevention regimensAm J Gastroenterol19999471733174210406229
- GreenbergRNOverview of patient compliance with medication dosing: a literature reviewClin Ther1984655925996383611
- San RomanALBermejoFCarreraEPérez-AbadMBoixedaDAdherence to treatment in inflammatory bowel diseaseRev Esp Enferm Dig (Madrid)2005974249257
- RobinsonAHankinsMWisemanGJonesMMaintaining stable symptom control in inflammatory bowel disease: a retrospective analysis of adherence, medication switches and the risk of relapseAliment Pharmacol Ther20133853153823834298
- MoodyGAJayanthiVProbertCSMac KayHMayberryJFLong-term therapy with sulphasalazine protects against colorectal cancer in ulcerative colitis: a retrospective study of colorectal cancer risk and compliance with treatment in LeicestershireEur J Gastroenterol Hepatol1996812117911838980937
- EadenJAbramsKEkbomAJacksonEMayberryJColorectal cancer prevention in ulcerative colitis: a case-control studyAliment Pharmacol Ther2000142145153
- BassiADoddSWilliamsonPBodgerKCost of illness of inflammatory bowel disease in the UK: a single centre retrospective studyGut200453101471147815361497
- KripalaniSYaoXHaynesRBInterventions to enhance medication adherence in chronic medical conditions: a systematic reviewArch Intern Med2007167654055017389285
- LoftusEVJrA practical perspective on ulcerative colitis: patients’ needs from aminosalicylate therapiesInflamm Bowel Dis200612121107111317119384
- KaneSHuoDMagnantiKA pilot feasibility study of once daily dosing versus conventional dosing mesalamine for maintenance of ulcerative colitisClin Gastroenterol Hepatol20031317017315017487
- KammMALichtensteinGRSandbornWJRandomized trial of once- or twice-daily MMX mesalazine for maintenance of remission in ulcerative colitisGut200857789390218272546
- DignassAVeermanHOnce versus twice-daily mesalazine (Pentasa) granules for the maintenance of remission in ulcerative colitis: results from a multinational randomised controlled trialGut200857Suppl 1A118268063
- LiWZhanZMJiangXLOnce daily vs multiple daily mesalamine therapy for mild to moderate ulcerative colitis: a meta-analysisColorectal Dis2016187O214O22327214762
- PedersenNThielsenPMartinsenLeHealth: individualization of mesalazine treatment through a self-managed web-based solution in mild-to-moderate ulcerative colitisInflamm Bowel Dis201420122276228525248002
- ElkjaerMShuhaibarMBurischJE-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided ‘Constant-care’ approachGut201059121652166121071584
- MoshkovskaTStoneMASmithRMBankartJBakerRMayberryJFImpact of a tailored patient preference intervention in adherence to 5-aminosalicylic acid medication in ulcerative colitis: results from an exploratory randomized controlled trialInflamm Bowel Dis20111791874188121830265
- CastiglioneFColomboGLValentinoMCDi MatteoSBrunoGMPatients’ perception of adherence to therapy in ulcerative colitis: results of a survey to specialized centersValue Health2015187A629
- MitraDHodgkinsPYenLDavisKLCohenRDAssociation between oral 5-ASA adherence and health care utilization and costs among patients with active ulcerative colitisBMC Gastroenterol20121213223006789