Abstract
Background
It has been documented that aerobic exercise may increase pulmonary functions and aerobic capacity, but limited data has evaluated a child’s satisfaction and pediatric quality of life (PQoL) with exercise training.
Objectives
This study aimed to investigate the effects of moderate-intensity exercise training on asthmatic school-aged children.
Subjects and methods
This study included 38 school-aged children with asthma (23 males and 15 females) aged between 8–12 years. They were randomly assigned to two groups, aerobic exercise (AE) and conventional treatment (Con ttt) groups. The AE group received a program of moderate-intensity aerobic exercise for 10 weeks with asthma medications and the Con ttt group received only asthma medications without exercise intervention. A home respiratory exercise was recommended for the two groups. Aerobic capacity was investigated using maximal oxygen uptake (VO2max), 6-minute walk test (6MWT), and fatigue index. PQoL was evaluated using Pediatric Quality of Life Questionnaire (PQoLQ). Also, pulmonary function tests were performed, and the results recorded.
Results
The findings of this study showed significant improvements in pulmonary functions and VO2max in the two groups; however, this improvement was significantly higher in the AE group than in the Con ttt group (p<0.05). The 6MWT and fatigue index improved in the AE group (p<0.05) but not in the Con ttt group (p>0.05). All dimensions of PQoL significantly improved in the AE group (p<0.05), but there was no significant improvement in the Con ttt group after the 10-week intervention period (p>0.05).
Conclusion
Ten weeks of physical exercise had beneficial effects on pulmonary functions, aerobic capacity, and PQoL in school-aged children with asthma. Effort and awareness should be dedicated to encouraging the active lifestyle among different populations, especially asthmatic children.
Background
Asthma is a common cause of chronic disorder and disability in pediatric population. It is considered to have a negative impact on the daily life activity of children, leading to exercise limitations. Asthmatic children, especially those suffering from limited disease control, show lesser activity than normal children.Citation1,Citation2
Children with asthma are inclined to have an inactive lifestyle when compared to healthy children. During exercise, they exhibit low endurance resulting from shortness of breath, termed as exercise-induced bronchoconstriction, and activity barriers according to healthy recommendation and advise.Citation3
Less aerobic capacity and asthma are manifested by difficulty in breathing, wheezing, and coughing, which in turn affect a child physically, socially, educationally, and emotionally.Citation4
Health-related quality of life (HRQoL) is lowered in asthmatic children when compared to their peers.Citation5 Previous studies advocated that asthma can be controlled and managed by undergoing regular exercise training and participating in sport activities.Citation6
Pulmonary rehabilitation has been highly recommended for chronic pulmonary diseases, particularly bronchial asthma in adult patients. The exercise intervention has been demonstrated to improve functional capacity, lower asthma symptoms, decrease health care resource utilization, and enhance HRQoL.Citation7,Citation8
In contrast, there have been few studies on rehabilitation in children suffering from chronic pulmonary diseases. These studies approved the positive influences of exercise on lung function and cardiopulmonary fitness, but data regarding the impacts of exercise training and physical activity on HRQoL in asthmatic school-aged children were poorly represented.Citation6
Asthmatic children were instructed to receive physical exerciseCitation9 and when asthma was controlled with medication, asthmatic children were able to carry out the physical exercise smoothly.Citation10 The greater physical activity is related to the greater quality of life (QoL) and psychological function; the more it enhanced the aerobic capacity, the more was the reduction in morbidity rate.Citation9–Citation11 Ninety percent of untreated asthmatic children would suffer from asthma symptoms during vigorous exercise, termed as exercise-induced bronchoconstriction.Citation12
An improved cardiorespiratory fitness may have positive effects for asthmatic children by improving exercise capacity and tolerance, the outcome being inhibition of exercise-induced bronchoconstriction.Citation13 The fitness level of exercise may be improved after exercise training in asthmatic children,Citation1,Citation9 an improvement in maximal oxygen uptake up to 20% was also noticed.Citation14 But, according to the previous reports, different methods of exercise training, varying in duration, mood, frequency, and intensity of exercise, were adapted based on the severity level of asthma.Citation15
Some intervention reports do not provide sufficient details about the exercise program, including types, intensity level, and structure of exercise.Citation3,Citation4 Some studies reported that children performed exercise program insufficiently.Citation4,Citation13,Citation14 Only one study approved that children enjoyed exercise training,Citation3 but there was no report on qualitative extensive examination combined with other physical measures.
Another study mentioned that the elucidation of shortness of breath throughout the physical exercise intervention has induced a risky manifestation of asthma, which may prevent children from exercise training.Citation16 Previous studies have documented that aerobic exercise may increase pulmonary functions and aerobic capacity, but limited data have evaluated the child’s satisfaction and pediatric quality of life (PQoL) with exercise training.Citation8–Citation11 The hypothesis of the current study was that 10-week moderate-intensity aerobic exercise may improve pulmonary function, aerobic capacity, and HRQoL in asthmatic children.
Objectives
This study aimed to evaluate the effect of 10-week aerobic exercise on pulmonary functions, aerobic capacity, and PQoL in school-aged children with asthma.
Subjects and methods
Subjects
Between June and September 2017, 38 asthmatic school-aged children between 8 and 12 years (23 males and 15 females) were recruited in this study. All children were referred by a chest physician to the outpatient Physical Therapy Department, Cairo University Children Hospital. All children were diagnosed with moderate persistent asthma (forced expiratory volume in 1 second [FEV1]=60%–80% predicted); were receiving long-acting β2-agonist and corticosteroid medications; and were suffering from dyspnea or wheezing, night cough, and airway obstruction in the last 6 months (based on pulmonary function tests). Thirty-eight children were randomly assigned to two groups with 19 children in each group. The first group received medical treatment with a program of moderate-intensity aerobic exercise three times/week for 10 weeks (aerobic exercise [AE] group), and the second group received only medical treatment without any exercise program (conventional treatment group [Con ttt]). All children of both groups were instructed to perform home breathing exercise. Any child that had post-bronchodilator FEV1 <60%, a severe medical illness such as uncontrolled heart disease, neuromuscular limitations, orthopedic problems, and endocrine disorders were excluded from the study, as these conditions could affect their capacity to perform physical exercise. This study was approved by the ethical committee of Physical Therapy Department, Cairo University Children Hospital, Cairo University. Written informed consent was obtained from parents or caregivers of all the children who participated in the study.
Randomization
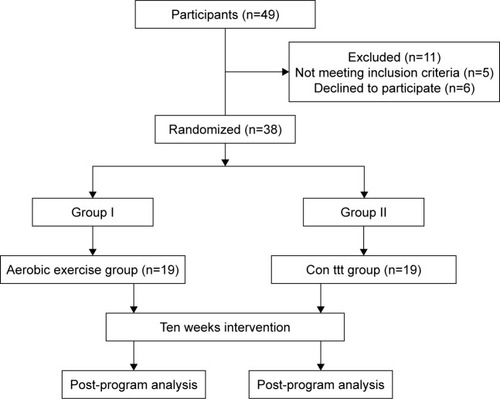
From among the 49 asthmatic children, 38 children participated in this study. Five children did not meet the inclusion criteria of the study, and six children declined to participate in the study without any registered cause. Randomization of 38 children was performed using sealed envelopes by an investigator who was not involved in the assessment, diagnosis, and treatment. The sealed envelopes contained an equal number of slips with either letter A or B indicating which child was in the study group or the control group. The letter A was assigned to AE group, and letter B was assigned to the Con ttt group. This allocation was performed before the initial assessment. The flow diagram showing the study protocol is presented in .
Instruments
Body weight, height, and body mass index (BMI) were measured for all children using weight and height scale. Treadmill (RT-103i, Revo Fitness, Lahore, Pakistan) was used for warming up exercise and measuring maximal oxygen uptake (VO2max); pulmonary functions were measured using a digital spirometer (Contec: SP10; Contec Medical Systems Co., Hebei Province, China); and child’s QoL and asthma control in asthmatic children were evaluated using Pediatric Quality of Life Questionnaire (PQoLQ).
Procedure
Baseline evaluation
All children were evaluated for the pulmonary functions (forced vital capacity [FVC], FEV1), aerobic capacity (VO2max, 6-minute walk test [6MWT], and fatigue index), and PQoL before the intervention (pre-program) and at the end of 10 weeks of intervention (post-program) by the previous investigator who was blinded concerning the group to which each patient was appointed.
At the commencement of the study, all children were instructed about the methods, procedure, and benefits of the study. Randomly, the children were assigned to two groups, with 19 children in each group. AE group (Group I) received a program of moderate-intensity aerobic exercise three times/week for 10 weeks in addition to asthma medications (combination of long-acting β2-agonists and corticosteroids), and Con ttt group (Group II) received only medications of asthma without any exercise program. Chest X-ray evaluation was carried out for all children regularly in the department of radiology and was abided by a pulmonologist to assess any lung abnormalities during the study period after their parental consent. The results of pulmonary functions, aerobic capacity, and PQoL were recorded at the beginning and at the end of the study.
Intervention
In the AE group, each child participated in the moderate-intensity aerobic exercise program (exercise training at 50%–70% of the maximum heart rate [HRmax]) for 10 weeks, three times per week, with each exercise session lasting for 40 minutes in the morning. Each child was instructed to inhale a bronchodilator before the exercise session and not to eat for 2 hours before the exercise session to avoid exercise-induced airway obstruction.
The exercise training program was in the form of walking on a treadmill with firmly grasping the rails to maintain balance, after the child had been accustomed to walk on the treadmill. The exercise session started with a 5-minute warm up which involved walking with no resistance and no inclination at the walkway of treadmill, followed by 30 minutes of walking with 5 degrees inclination at the walkway of the treadmill and adjusted speed to reach 50%–60% of the HRmax in the first 5 weeks of the study. Then the inclination was increased to 10 degrees and the speed was increased up to 60%–70% HRmax in the second 5 weeks of the study. The session ended with 5 minutes of recovery in which the intensity of the exercise was reduced to the level of the warm up.
All the children of the two groups were instructed to receive asthma medications regularly. Home breathing exercise was recommended for both groups: study and control groups.
Final evaluation
After the 10-week intervention period, pulmonary functions, aerobic capacity, and PQoLQ were reassessed in the AE and Con ttt groups.
Sample size
Sample size for this study was calculated using the VO2max measure. A previous study has approved that the aerobic exercise showed a significant mean difference in VO2max measure (5.3 mL/kg/min) with standard deviation (4.5 mL/kg/min).Citation2 According to this difference and ability to achieve a power of 80% (α=0.05) our study required 16 children in each group. A dropout rate of 20% was assumed in the study; therefore, 19 children were recruited in each group to ensure that at least 16 children completed the study.
Data analysis
Descriptive statistics were applied in mean and standard deviation form. The normality of the data was tested using the Kolmogorov–Smirnov test. Inferential statistics assessed alterations of all measurements using unpaired t-test between AE and Con ttt groups, and paired t-test was applied to measure changes within the group. SPSS version 20.0 (SPSS, Chicago, IL, USA) was used for data analysis with a significance level of p<0.05 for all statistical measurements.
Results
Baseline characteristics
As demonstrated in , there were no significant differences between the AE and Con ttt groups at the beginning of the study in regard to their gender, age, BMI, FVC, FEV1, VO2max, 6MWT, fatigue index, and PQoLQ (p>0.05).
Table 1 Baseline characteristics of all children participating in this study
Pulmonary functions
There was no significant difference in FVC and FEV1 between the two groups before the intervention (p>0.05), as presented in . However, the post-treatment outcomes showed significant differences in favor of the AE group (p<0.05), as presented in . Comparison of the pre-and post-treatment mean values of the pulmonary functions in both AE and Con ttt groups reported significant changes (p<0.05), as presented in .
Table 2 Pre- and post-treatment mean differences of BMI, lung functions, aerobic capacity, and HRQoL within each group
Table 3 Mean differences of BMI, lung functions, aerobic capacity, and HRQoL between the two groups pre- and post-treatment
Aerobic capacity
As demonstrated in , comparison of the mean pretreatment values of VO2max, 6MWT, and fatigue index between aerobic and conventional groups indicated non-significant differences (p>0.05). At the end of the study, the two groups showed significant improvement in VO2max (p<0.05), as presented in . Comparison of the pre- and post-treatment mean values of VO2max indicated significant differences between the aerobic and conventional groups (p<0.05) in favor of the AE group. On the other hand, the 6MWT and fatigue index improved significantly in the AE group (p<0.05) when compared to the Con ttt group (p>0.05) at the end of the study. Comparing of the pre-and post-treatment mean values of the 6MWT and fatigue index indicated significant differences between the aerobic and conventional groups (p<0.05) in favor of the aerobic exercise program, as presented in .
Pediatric Quality of Life Questionnaire
As demonstrated in , comparison of the mean pretreatment values of overall QoL, activities, symptoms, and emotion scores between both groups indicated nonsignificant differences (p>0.05). In addition, the post-treatment comparison indicated significant differences of all finding measures in favor of the study group (p<0.05). As demonstrated in , comparison of the pre- and post-treatment mean values of overall QoL, activities, symptoms, and emotion scores indicated significant differences in the AE group (p<0.05). But, the Con ttt group showed nonsignificant improvement in all dimensions of PQoL at the end of the study period (p>0.05).
Attendance rate
In this study, there was a high rate of satisfaction and fun among the children, which was evident by the rate of attendance which was 97.7%. Thirteen children regularly attended 30 sessions of the intervention program. Two children did not attend three sessions, three children did not attend two sessions, and one child missed only one session.
Gender differences
As demonstrated in , there were nonsignificant differences between males and females at the beginning of the study within each group. After 10-week intervention, the AE group showed significant improvements in all variables in both genders with nonsignificant differences between the two genders. While the Con ttt group showed significant improvement in FEV1, FVC, and VO2max in the two genders, there were nonsig-nificant differences in fatigue index, 6MWT, and all dimensions of PQoL in the two genders. Also, the mean post-treatment values of all variables indicated nonsignificant differences between males and females within each group (p>0.05).
Table 4 Gender differences in the pre- and post-treatment mean values of BMI, lung functions, aerobic capacity, and HRQoL in the AE and Con groups
Discussion
The major findings of this study showed that asthmatic children participating in aerobic exercise training showed improved pulmonary functions, aerobic capacity, and PQoL. These findings were obtained through a program involving moderate-intensity exercise. The asthmatic children had a satisfied participating program without asthma restrictions or attacks, and they discerned that their pulmonary functions and aerobic capacity had increased. Also, PQoL had improved post-treatment compared with pre-treatment record. The children who participated in the aerobic exercise program appreciated being acknowledged as competent, and the treatment was nominated considering any child having asthma is a normal. The examiners confirmed that the exercise was moderate intensity and approved satisfaction while joining the exercise that it was comfortable and easy to perform; they also confirmed equitable competition and used satisfactions to participate in the exercise program.
Many previous studies investigated the effect of exercise in asthmatic children with different exercise modes including running,Citation13,Citation17 cycling,Citation18,Citation19 and swimming,Citation14,Citation20 which were highly applied regularly. These studies did not determine whether the children were feeling satisfied and experiencing fun within these exercise programs or which interactions the children felt most pleasurable. The current study assessed the child’s satisfaction and enjoyment.
This study presumes that the fulfillment and pleasure experienced by the children inspired them to participate in the moderate-intensity aerobic exercise and contributed to the high attendance during these training sessions. Previously, only two studies determined the perspectives of children during an exercise program. One study showed that the children’s fulfillment and enjoyment inspired them to participate in an exercise intervention at a high intensity, contributing to the high attendance rate and no absences during exercise training intervention.Citation1 Second study explained that the perception of children showed the heightened capability to control asthma throughout the exercise intervention.Citation11 Unfortunately, the exercise types and devotion have not been clarified.
The attendance rates and absence during an exercise program may indicate that the children are motivated and in favor of participating in different exercise modes. In asthmatic children interventions, absence rates of 22% in the 6-week individuated cycle Ergometer trainingCitation19 and 13% in the 4-month running training programCitation17 have been informed.
Lower drop-out rates were mentioned in a 3 month program of frequent exercise training with various activities in the indoor rehabilitation gym and home program about 4%Citation3 and decreased 3% in eight-week training basketball program.Citation4 These two studies did not mention the causes of absence, however, it was concluded that these studies involved mutual patient support. Peer support has been exhibited to be related to the high-intensity physical exercise regardless asthma.Citation21
According to the current study results, the rate of attendance was very high (97.7%) during the study program. Similar results were reported in the previous studiesCitation1,Citation22 that reported highest attendance rate in the active play program. The intervention program conducted training sessions in nearby areas, which might have contributed to increased attendance rate.Citation22 Also, a study including a small sample size would ensure that all the participants attended the intervention session, when compared to the studies which included a large number of patients.Citation1 In the present study, the participants’ home was close to the study place and also, a small number of study participants had led to an increase in the rate of attendance. On the other hand, a previous study reported the attendance rate of 68% in their study, which evaluated the effects of running exercise on 10 asthmatic children. Asthmatic children may feel running exercise with various interventions as fun when compared with indoor training, performed in the present study.Citation23 A review study reported that intensity was the most prominent factor than the mode of aerobic exercise for increasing aerobic capacity after an exercise training.Citation9
In one study, children’s reports revealed that aerobic exercise and satisfaction are vital in improving the activity and adequate intensity. In healthy children, high-intensity anaerobic exercise caused higher enhancements in aerobic capacity than low-intensity exercise.Citation24
In the current study, asthmatic children received moderate-intensity aerobic exercise (70% HRmax). Generally, the intensity of exercise has been lowered during each session as the short active periods is required to recognize the exercise program, including adapting and fitting the monitors of heart rate. Aerobic capacity improved significantly in the AE group than in the Con ttt group after the intervention program when compared with the baseline measurements. The fatigue index was reduced in the AE group and increased in the Con ttt group, but the changes were nonsignificant, which could be ascribed to improvement in respiratory muscle strength. Our study provided an explanation for the increased capability of managing aerobic exercise, as well as improved discerned ability or increased feeling of competence.
The consequence of perceived ability and normality for the asthmatic children and the fitting of children to sociable standards is advantageously reported.Citation25 This study showed that examiners can produce satisfaction, fun, and extreme aerobic capacity with great attendance rate by concentrating on self-reliance and normality of children, and by enhancing, clarifying, and identifying all social standards in the children’s study. It might be to suggest that the examiners role and the aerobic exercise program are just as important as the clinical organization comprising of planning, scheduling, guiding, and designing the exercise. Previous studies have indicated that incentive and obligation in exercise training were dependent on guidance; the construction provided; and the fundamental psychological requirement for independence, connectedness, and capability.Citation26
The present study design of moderate-intensity aerobic exercise appeared to improve expertise, satisfaction, and enjoyment together with the examiner’s discussion on the establishment of equitable contest and focus on expertise, fun, society, and handling the children that are well qualified. The findings of the restrictions induced by asthma away from the treatment scene and the children’s desire to be normal despite having asthma may suggest the experiences and interaction within the exercise program. The examiners’ deliberate emphasis on treating asthmatic children as normal competent subjects may thus have appeared to these asthmatics as motivating them to exercise and enjoy the exercise training despite the obvious presence of asthma. Physical exercise barriers may be encountered either due to physiological restrictions resulting from a disorder or due to pitiable psychological adaptation to the disorder.Citation10
The outcomes of the current study show that the restrictions of physical exercise depend on the situation and may change with the social background. Asthmatic children may endure aggravation, confusion, and less self-trust resulting from disease-related restrictions.Citation25,Citation27 Asthmatic children may leave physical exercise training due to the fear of parents and defensiveness.Citation16 In the current study, participants appeared to overcome those obstacles and restrictions, and the parents or caregivers provided the children independence by staying away during the aerobic exercise sessions.
The reports of children experiencing reported enhancements in aerobic capacity and exercise tolerance, contentment, and manifestations of asthma, emphasize the positive effects of producing various social conditions and standards for treatment of asthmatic children. Furthermore, the child’s improvement of VO2max, 6MWT, and especially QoL, support the possibility that the treatment program can cause change in children with increased age, partake in low initiated aerobic exercise by themselves, and have a lowered QoL compared with conventional group.Citation28
The current treatment may be perceived as a required resource. Nevertheless, aerobic exercise is related to many beneficial findings in asthma sufferersCitation11 and can result in savings of expenses related to mortality and morbidity, while aiding in reduction of good-health expense disbursements, which cost from 1% to 2% of total health care expenses in developed countries.Citation29
Conclusion
According to the study findings, improving the level of physical activity among the asthmatic children has a positive effect on the pulmonary functions, aerobic capacity, and PQoL. Effort and awareness should be dedicated to encouraging the active lifestyle among different populations, especially asthmatic children.
Acknowledgments
The authors would like to thank the parents for allowing their children to participate in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
- WestergrenTFegranLNilsenTHaraldstadKKittangOBBerntsenSActive play exercise intervention in children with asthma: a pilot studyBMJ Open20166e009721
- MeyerAGuntherSVolmerTTaubeKBaumannHJA 12-month, moderate intensity training program improves fitness and quality of life in adult with asthma: a controlled trialBMC Pulm Med2015155625947010
- van VeldhovenNHVermeerABogaardJMChildren with asthma and physical exercise: effects of an exercise programClin Rehab200115360370
- BasaranSGuler-UysalFErgenNEffects of physical exercise capacity and pulmonary function in children with asthmaJ Rehab Med200638130135
- JuniperEFHow important is quality of life in pediatric asthma?Pediatr Pulmonol1997151721
- RamFSRobinsonRMBlackPNEffects of physical training in asthma: a systematic reviewBr J Sports Med20003416216710854014
- CooperCBExercise in chronic pulmonary disease: limitations and rehabilitationMed Sci Sports Exer200133S643S646
- BTS Statement. Pulmonary rehabilitationThorax20015682783411641505
- CrosbieAThe effect of physical training in children with asthma on pulmonary function, aerobic capacity and health-related quality of life: a systematic review of randomized control trialsPediatr Exerc Sci20122447248922971562
- MosqueraRASamuelsCFloresGFamily language barriers and special-needs childrenPediatrics2016138e2016032127638932
- CarsonKVChandratillekeMGPicotJBrinnMPEstermanAJSmithPJPhysical training for asthmaCochrane Database Syst Rev20139171
- McFaddenERJrGilbertIAExercise-induced asthmaN Engl J Med1994330136213678152449
- VarrayALMercierJGPrefautCGIndividualized training reduces excessive exercise hyperventilation in asthmaticsInt J Rehabil Res1995182973128748052
- VarrayALMercierJGTerralCMPrefautCGIndividualized aerobic and high intensity training for asthmatic children in an exercise readaptation program: is training always helpful for better adaptation to exercise?Chest1991995795861995211
- WanrooijVHWilleboordseMDompelingEvan de KantKDGExercise training in children with asthma: a systematic reviewBr J Sports Med2014481024103123525551
- WilliamsBHoskinsGPowJNevilleRMukhopadhyaySCoyleJLow exercise among children with asthma: a culture of over protection? A qualitative study of experiences and beliefsBr J Gen Pract201060577e319e32620822682
- OrensteinDMReedMEGroganFTJrCrawfordLVExercise conditioning in children with asthmaJ Pediatr19851065565603981308
- FanelliACabralALNederJAMartinsMACarvalhoCRExercise training on disease control and quality of life in asthmatic childrenMed Sci Sports Exerc2007391474148017805077
- CounilFPVarrayAMateckiSTraining of aerobic and anaerobic fitness in children with asthmaJ Pediatr200314217918412584541
- MatsumotoIArakiHTsudaKEffects of swimming training on aerobic capacity and exercise induced bronchoconstriction in children with bronchial asthmaThorax19995419620110325893
- GomesELCarvalhoCRPeixoto-SouzaFSActive video game exercise training improves the clinical control of asthma in children: randomized controlled trialPLoS One201510e013543326301706
- Graff-LonnevigVBevegardSErikssonBOKraepelienSSaltinBTwo years’ follow-up of asthmatic boys participating in a physical activity programmeActa Paediatr Scand1980693473527376860
- FitchKDBlitvichJDMortonARThe effect of running training on exercise-induced asthmaAnn Allergy19865790943740562
- BaquetGvan PraaghEBerthoinSEndurance training and aerobic fitness in young peopleSports Med2003331127114314719981
- ProtudjerJLKozyrskyjALBeckerABMarchessaultGNormalization strategies of children with asthmaQual Health Res2009199410418997151
- CurranTHillAPNiemiecCPA conditional process model of children’s behavioral engagement and behavioral disaffection in sport based on self-determination theoryJ Sport Exerc Psychol201335304323404877
- GroverCArmourCVan AsperenPPMolesRJSainiBMedication use in Australian children with asthma: user’s perspectiveJ Asthma201350231241
- PawlowskiCSThomsenTTSchipperijnJTroelsenJBarriers for recess physical activity: a gender specific qualitative focus group explorationBMC Public Health20141463964824958158
- TurnerSPredicting and reducing risk of exacerbations in children with asthma in the primary care setting: current perspectivesPragmat Obs Res20167333927822136