Abstract
Objective
This review aims to summarize the current literature on patient-reported outcomes (PROs) in spondyloarthritis (SpA).
Patients and methods
We performed a systematic literature review to identify studies (original articles and narrative and systematic reviews) regarding PROs (health-related quality of life [HRQoL], satisfaction, preferences, adherence/compliance, and persistence) in SpA patients published in the European Union through December 2016. International databases (Medline/PubMed, Cochrane Library, ISI Web of Knowledge, Scopus) were searched using keywords in English. The methodological quality of the studies was assessed using the Oxford Centre for Evidence-Based Medicine criteria.
Results
A total of 26 publications met the inclusion criteria. Generally, studies indicated that SpA has a negative impact on patients’ HRQoL. In patients with ankylosing spondylitis, physical domains were more affected than emotional ones, whereas for psoriatic arthritis, both physical and psychological factors were strongly affected by the disease. Data indicated that biological agents (BAs) greatly contributed to improvement in HRQoL in both ankylosing spondylitis and psoriatic arthritis patients. Findings on compliance with BAs were heterogeneous. However, persistence rates exceeded 50% irrespective of the BA administered. Results on preferences indicated that most SpA patients prefer being involved in decisions regarding their treatment and that besides efficacy and safety, frequency and route of administration may influence patients’ preferences for BAs.
Conclusion
Implementing management programs for SpA patients focuses on the physical, emotional, and social consequences of the disease, in addition to assessing and including patient preferences in the treatment decision-making process, could be crucial to improve patients’ HRQoL and ensure their satisfaction and compliance with treatment.
Introduction
Spondyloarthritis (SpA) refers to a group of interrelated inflammatory diseases that share some features, including articular and extra-articular manifestations.Citation1 SpA affects 1%–3% of the general population. In European countries, the reported prevalence varies between 0.3% and 1.9%.Citation2 Ankylosing spondylitis (AS) and psoriatic arthritis (PsA) are the most frequent types of SpA. AS mainly affects the spine and sacroiliac joint and to a lesser extent the peripheral joints and entheses. PsA is characterized by the involvement of both peripheral and/or spinal joints and skin manifestations.Citation2,Citation3 The European prevalence of AS is 0.03%–1.8%, while prevalence is 0.05%–0.42% for PsA.Citation4
PsA causes joint damage that leads to loss of articular function; specifically, a high percentage of PsA patients have more than one deformed joint and about 20% develop a very destructive disabling form of arthritis.Citation5 As a consequence, progression of PsA leads to a reduction in patients’ functional capacity, affecting their social and working lives.Citation6 Various studies have suggested that SpA has a negative impact on functional status and patients’ health-related quality of life (HRQoL),Citation7–Citation9 and it is associated with an increased risk of death.Citation5
AS patients typically present axial skeleton and sacroiliac joint involvement, resulting in structural and functional impairment. Additionally, many extra-articular features may also occur in AS patients, including uveitis, osteoporosis, bowel disease, and cardiac, pulmonary, skin (psoriasis), and kidney involvement.Citation10 The incidence of cardiovascular disease and mortality is also increased in AS patients.Citation5 Adults with AS may thus have significantly reduced HRQoL, in addition to limitations in physical functioning and comorbidities that are strongly associated with decreased work productivity.Citation7
In view of the clinical and social implications of SpA, management of SpA patients should aim to prevent structural damage and preserve their functional status, in order to optimize HRQoL.Citation11–Citation13 With this aim, new therapies, such as biological therapies, have been developed, and new treatment strategies, eg, treat to target, have been adopted over the last decade.Citation14 The implementation in routine-practice of biological agent (BA) therapyCitation11–Citation13 has led to a significant improvement in clinical outcomes, including the physical functioning of patients with rheumatic disease.Citation15 However, poor adherence to medication in SpA patients remains a challenge in clinical practice.Citation16 New BAs involve different routes of administration and different toxicity, and are sometimes associated with higher drug costs, all of which may influence patient adherence and preference for medication.Citation17 In view of the new scenario, a more patient-centered approach to decision making is needed. In fact, assessing and including patients’ preferences within routine clinical practice are related to an increase in medication adherence, as well as improved treatment outcomes. This work reviews and summarizes the current literature on patient-reported outcomes (PROs) in patients with SpA (AS and PsA) in the European Union (EU).
Methods
We performed a systematic literature review to identify studies on PROs in SpA (AS and PsA) patients. Studies assessing HRQoL, satisfaction, adherence/compliance, or persistence with treatment and patients’ preferences for treatment in SpA populations published in the EU through December 2016 were selected. As recommended by the Cochrane Handbook for Systematic Reviews of Interventions,Citation18 publicly accessible international databases (Medline/PubMed, Cochrane Library, ISI Web of Knowledge, Scopus) were searched using keywords in English joined by the Boolean operators “OR” and “AND” ().
Table 1 Search terms and search strategies
Inclusion criteria
We included original articles, narrative reviews, and systematic reviews in English and Spanish that evaluated PROs (HRQoL, satisfaction, adherence/compliance, or persistence with treatment and patients’ preferences) in SpA patients in EU setting.
Exclusion criteria
We excluded studies conducted in non-EU countries, letters to the editor, editorials, experts’ opinions, case studies, congress proceedings, mixed-population studies, those that focused on only one explanatory factor, and studies related to specific medical interventions.
Selection of studies
Following removal of duplicates and irrelevant publications, two independent researchers screened the remaining studies based on preset inclusion and exclusion criteria. Discrepancies were resolved by consensus. The methodological quality of the studies was assessed using Oxford Centre for Evidence-Based Medicine criteria.Citation19
Results
Studies selected
The database searches yielded a total of 8,954 titles. Of these, 8,864 were excluded as irrelevant to study purposes (4,748, 53%) or duplicates (3,916, 43.7%). Following full-text reading and application of the inclusion/exclusion criteria, 26 of the remaining 290 publications were included in the review (). Most publications reviewed (n=16, 61.5%) were cross-sectional studies examining HRQoL in SpA patients, while a lower proportion evaluated other PROs such as persistence, satisfaction, or preferences ().
Figure 1 Flowchart of study selection according to PRISMA.
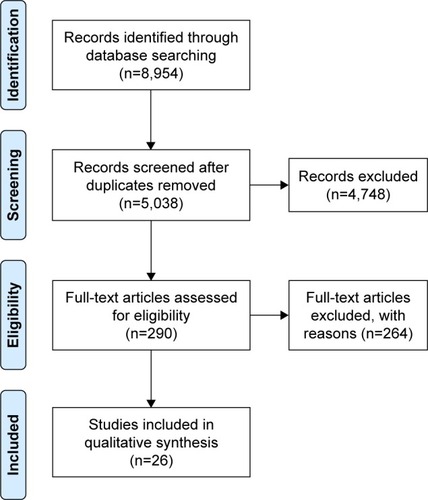
Table 2 Description of studies reviewed
HRQoL in SpA patients
Of the 18 publications examining HRQoL in SpA patients, 13 (72.5%) employed generic HRQoL instruments, while only four used disease-specific questionnaires, alone or in combination with generic ones ( and ).
Table 3 Characteristics of HRQoL-related studies reviewed
HRQoL in SpA patients compared with other rheumatological disorders and the general population
Salaffi et alCitation20 revealed that inflammatory rheumatic diseases, including SpA, have a negative impact on patients’ HRQoL, affecting both physical (physical component summary [PCS]) and mental (mental component summary [MCS]) dimensions. PCS was more affected in AS, whereas both physical and emotional well-being deteriorated in patients with PsA.
Correlation between clinical variables and HRQoL in SpA
Of the studies selected, twoCitation20,Citation21 sought to identify explanatory clinical factors for HRQoL in SpA. In particular, Salaffi et alCitation20 showed that for inflammatory rheumatic diseases, high disease-activity score, chronic comorbidity, and radiographic damage negatively affected PCS, while the severity of psoriatic lesions (Psoriasis Area and Severity Index) was significantly associated with poor MCS in PsA patients. In the same line, Jajić et alCitation21 observed that for AS patients, clinical variables correlated mainly with PCS, whereas in PsA patients both PCS and MCS were affected by the disease. Functional status, measured by the Bath Ankylosing Spondylitis Functional Index (BASFI), had the strongest impact on PCS in both diseases.
Depression, anxiety, and HRQoL in SpA
Kotsis et alCitation22 and Hyphantis et alCitation23 investigated the prevalence of major depressive disorders in SpA and rheumatoid arthritis (RA) and their association with HRQoL. Both studies showed that psychological factors were strongly associated with HRQoL in PsA patients. In particular, both anxiety and concern about bodily symptoms were independent correlates of the physical domain of HRQoL.Citation22 On the other hand, only cognitive variables were important correlates of HRQoL in AS patients, with illness concern being the only significant independent correlate of physical HRQoL.Citation23
HRQoL and work productivity in SpA patients
Two studies evaluated the relationship between HRQoL and productivity loss in SpA patients. Chorus et alCitation24 showed a positive association between work and HRQoL PCS; however, no association was found with MCS. Kawalec et alCitation25 observed that patients’ HRQoL, expressed as utility scores, was negatively correlated with absenteeism, presenteeism, and indirect costs, suggesting that higher HRQoL was associated with higher productivity and lower indirect costs. Disease-activity score was positively correlated with indirect costs and negatively correlated with HRQoL. Therefore, the greater the disease activity, the lower the utility and the larger the indirect cost.
Compliance and HRQoL in SpA patients
Hromadkova et alCitation26 assessed the relationship between drug compliance and HRQoL in patients with different rheumatic disorders, including SpA. A significantly negative correlation between compliance and HRQoL PCS was found in SpA patients, suggesting that patients with worse HRQoL might be more compliant with treatment.
Influence of biological therapies on SpA-patient HRQoL
Three of the studies investigated the impact of BAs on HRQoL in SpA patients in the clinical practice setting. Saad et alCitation27 reported a significant improvement in all Short Form (SF)-36 subscales after 6 months of therapy with BAs, with greatest improvements observed in PCS. Sieper et alCitation28 found that in nonradiographic axial SpA (nr-axSpA) patients, treatment with BAs was associated with improved clinical outcomes (pain, remission, acute episodes) compared to BA-naïve patients. Furthermore, BA-naïve patients reported greater presenteeism, overall work impairment, and activity impairment than BA-treated patients. In line with previous studies, Wallman et alCitation29 showed that following BA treatment, both HRQoL (EuroQoL 5D utility and visual analog scale) and clinical outcomes (pain, erythrocyte-sedimentation rate and CRP) improved rapidly in both nr-axSpA and AS patients.
HRQoL in AS patients
Factors influencing HRQoL in AS patients
Kucharz et alCitation30 observed that almost two-thirds of AS patients considered pain a very important risk factor in their HRQoL. In addition, around 50% of patients indicated that the need for assistance in activities of daily living (ADL) and impairment in family life potentially influenced their HRQoL. Young male patients were more concerned by the risk of losing their jobs than older ones, while impairment of sexual life due to the disease was more important to males than to females. Management of the disease (treatment or frequent hospitalization) was not considered a significant factor impairing their HRQoL.
Patient-reported measures and HRQoL in AS
Mobility and physical function are the most important end points for AS patients, and several instruments have been developed to evaluate disease activity from patient perspectives (BAS Disease Activity Index [BASDAI]) and physical functioning (BASFI and BAS Metrology Index). A correlation between physical function (BASFI) and HRQoL in AS patients was established by Ariza-Ariza et al,Citation31 showing that BASFI score presented an independent association with HRQoL. This association was confirmed by de las Peñas et al.Citation32 These authors observed that function (BASFI) and disease activity (BASDAI) were correlated with HRQoL (physical function, pain, and vitality domains). In the same vein, Ariza-Ariza et alCitation33 found that physical function (BASFI) and disease activity (BASDAI) were the main determinants of health-state utility values in AS patients. Finally, a recent study published by O’Dwyer et alCitation34 confirmed that adults with AS show a significant reduction in physical fitness compared to age- and sex-matched healthy controls. The AS group demonstrated significantly lower cardiorespiratory fitness, flexibility, muscular strength, and increased body fat compared to controls. All components of physical fitness were associated with physical function (BASFI), while only aerobic capacity was associated with HRQoL (ASQoL).
HRQoL in PsA patients
Patient-reported measures and HRQoL inPsA patients
Tälli et alCitation35 showed that patient global assessment (PGA) in PsA was determined mainly by physical but also physiological aspects of the disease. In particular, coping, pain, work, leisure activities, and anxiety were identified as the main explanatory factors for PGA scores. Skin lesions seemed to have a lower impact on PGA than joint involvement, which had a larger effect on PsA patients’ HRQoL. Similarly, Puyraimond-Zemmour et alCitation36 established an association between pain and coping with patient-acceptable symptom state, showing that less pain and better coping were correlated with better level of acceptability of disease status.
Disease severity and HRQoL in PsA patients
Brodsky et alCitation37 found strong correlations between both generic (EuroQol 5D) and specific HRQoL (PsAQoL) instruments and disease severity assessed by Health Assessment Questionnaire (HAQ) disability score, patient-pain visual analog scale, PGA, and BASDAI. However, disease duration and psoriasis correlated weakly with these HRQoL instruments.
Compliance and persistence in SpA patients
According to the definition of adherence/compliance (extent to which patient acts in accordance the prescribed interval and dose of dosing regimen) and persistence (duration of time from initiation to discontinuation of therapy),Citation38 five studies evaluated persistence to BA therapy in SpA patients, one assessed compliance with BA treatment, while the remaining publication was a systematic review ().
Table 4 Characteristics of adherence/persistence-related observational studies reviewed
The systematic reviewCitation39 reported great variability in the operational definition and measurement of adherence/compliance among studies. Most studies focused on persistence, measured by survival time, retention, or continuation rates, while fewer publications assessed adherence based on proportion of days covered or medication-possession ratio. The results suggested better compliance with biological therapy in SpA compared to RA. Age, female sex, comorbidity, poor clinical condition, and number of previous BAs were identified as explanatory factors for patient compliance.
Results of persistence in SpA patients were heterogeneous among the studies reviewed. Lyu et alCitation40 observed that among AS and PsA patients who were initiating biological treatment, persistence at 12 months was relatively low (48%–58%). Nonetheless, Saad et alCitation41 reported a higher survival rate on their index BA (75.5%) for patients with PsA after 12 months of follow-up. In line with these results, Kristensen et alCitation42 showed drug-survival rates at 12 and 24 months of 86% and 78% for peripheral arthritis patients and 74% and 68% for patients with isolated AS starting biological therapy. Likewise, Wallman et alCitation29 showed a high proportion of patients with nr-axSpA (70%) and AS (77%) remaining on BA therapy after three years follow up. For long-term persistence, Favalli et alCitation43 reported cumulative 8-year retention of 57.2% for axSpA and 51.9% for PsA. Finally, related to compliance, Hromadkove et alCitation26 reported that only 38.3% of patients with AS were compliant with BA treatment, as indicated by Compliance Questionnaire Rheumatology score 80).
Satisfaction with decision making
Renzi et alCitation44 examined PsA patients’ preferences about their role in the decision-making process, as well as their satisfaction with both their care and their knowledge about PsA therapies (). Overall, the majority of PsA patients (72.7%) wanted to be involved in decision making, although 40.6% preferred that their doctors make the final decision after considering their opinion; 65.5% of PsA patients reported being completely or fairly satisfied with their care and information. Multivariate analysis showed that information on both treatment side effects and treatment options was significantly associated with overall satisfaction, confirming that improving patient–doctor communication may improve patients’ satisfaction with their care.
Table 5 Characteristics of studies of satisfaction and preferences for treatment that were reviewed
Patient preferences for SpA treatments
Two publications examined patient preferences for treatment characteristics (). Nolla et alCitation45 assessed the relative importance given by patients with rheumatic diseases (RA, AS, and PsA) and rheumatologists to attributes of BAs. For these patients, although efficacy (pain relief and improvement in functional capacity) and safety (risk of adverse events) were key aspects, both the frequency (time until perceiving the need for a new dose) and method of administration played an important role as attributes of BAs. Rothery et alCitation46 observed that PsA patients conferred the greatest importance to eliminating severe side effects of sickness/nausea and the least importance to a change in risk of relapse. Patients were willing to accept a large increase in the risk of relapse in order to reduce the side effects of sickness/nausea.
Discussion
This review reports current knowledge on PROs in SpA patients in the EU. To date, the evidence indicates that similar to other rheumatic conditions,Citation47 SpA patients report poorer HRQoL compared to the general population. For AS patients, physical domains were more impaired than emotional well-being, whereas for PsA patients both physical and psychological factors were strongly affected by the disease. Indeed, prevalence of depressive symptoms was higher in PsA than in AS and particularly high in patients with polyarthritis. In PsA, anxiety symptoms and concern about somatic symptoms were independently correlated with HRQoL, while in AS patients only impairment of cognitive function was found to be associated with HRQoL deterioration.
Work disability is a major problem for SpA patients. Indeed, these diseases tend to occur in the working-age population, and studies have suggested that the ability to work and to perform ADL positively influence patients’ perceptions of their physical performance. In a cross-sectional study conducted in the US,Citation7 limitations in ADL were significantly associated with lower PCS scores in patients with AS whereas for PsA patients ADL limitations were associated with both lower PCS and MCS scores, which supports results from EU reports in this review.
The PCS in AS patients is important. In these patients, physical restrictions in joint mobility, particularly of the spine,Citation48,Citation49 in addition to reductions in aerobic capacityCitation50,Citation51 and loss of skeletal muscle,Citation52,Citation53 are frequent. We found that physical function measured by the BASFI was highly correlated with HRQoL, indicating that functional impairment associated with AS can cause a significant impact on patients’ HRQoL, with important limitations on their daily activities. Conversely, PsA is a heterogeneous disease that is greatly influenced by psychological and social aspects of the disease. The most affected aspects of HRQoL in PsA patients were coping with a chronic disease, limitations on work and/or leisure time, and anxiety or depression. Interestingly, joint symptoms had a greater effect on PsA patients’ lives than skin symptoms.
Overall, SpA treatment has changed dramatically with the development of BAs.Citation11–Citation13 Substantial improvements in the signs and symptoms of PsA patients have been reported for these agents, although all BAs are similar in terms of efficacy and safety.Citation54 The current evidence suggests that routine clinical use of BAs contributes greatly to the improvement of HRQoL in SpA patients. Significantly, the greatest improvements were found in the PCS, with smaller but still significant improvements in the MCS.
However, the potential clinical benefits demonstrated by BAs in clinical trials may be reduced by poor adherence and early discontinuation of treatment in clinical practice, thereby increasing medical costs and resulting in the need for more aggressive treatments.Citation55–Citation57 Results on compliance with biological treatment of SpA patients were heterogeneous in real-life situations; nonetheless, all rates of persistence at 12 months were >50% of the population, with no significant differences between PsA and AS patients and irrespective of the individual BA administered. A recent retrospective cohort studyCitation58 conducted in 53,477 BA-naïve patients with rheumatic conditions in the US reported that the majority of patients remained persistent in the first year of BA therapy; however, they observed lower adherence ratios when 12-month medication-possession ratios were measured. Overall, in line with our results, patient characteristics, such as male sex, high disease activity, or peripheral arthritis, and treatment characteristics, such as concomitant methotrexate use, positively influence treatment persistence. Interestingly, higher HRQoL and a lower rate of functional disability were associated with lower compliance with treatment. According to Calip et al,Citation58 young adults were less likely to be treatment-compliant, resulting in more comorbidities, hospitalizations, or visits to the emergency department.
In rheumatic diseases, assessing and including patient preferences in the decision-making process have been found to contribute to increased medication adherence, improved treatment outcomes, reduced health care costs, and enhanced patient satisfaction.Citation59–Citation61 The available evidence suggests that European SpA patients attach great importance to outcomes (pain relief and improvement of functional capacity, low risk of adverse events); however, process attributes, such as self-administration at home or longer time between doses, were also considered important attributes for BAs. Preferences varied depending on the PsA-disease states: low-disease-state patients were more concerned about the side effects of sickness/nausea than about the risk of relapse.
Results on PsA patients confirm that most patients want to be involved in decision making about their treatment. Satisfaction was associated with doctors providing treatment information and actively involving patients in decision making. In line with these results, Nota et alCitation62 reported that most patients with rheumatic disease preferred to be involved in decisions about their medication and especially preferred more participation in decision making regarding their first treatment, which most commonly occurs in newly diagnosed patients.
Limitations
Possible limitations of this review include the heterogeneity of the articles retrieved in terms of patients, treatments, or methodology. Regarding the design, all studies assessing HRQoL in SpA were cross-sectional, and it is important to take into account that cross-sectional design might limit comparisons among SpA patients and with other diseases and does not allow the drawing of final conclusions about the factors associated with HRQoL and their cause–effect relationship. On the other hand, there may be relevant publications in languages other than English and Spanish or that are indexed in different databases than those searched that we have not identified in this review.
Conclusion
SpA has a negative impact on patients’ HRQoL. The physical aspects of HRQoL, especially functioning limitations and pain, are severely affected in both AS and PsA patients. In PsA patients, the impact of disease on emotional well-being is considerable. In both disease, BA therapy is associated with improvements in both physical and emotional status. However, these potential improvements may be reduced by poor adherence. Even though there are inconsistent findings, persistence rates in SpA patients are >50%, irrespective of the individual BA administered. Finally, results on preferences showed that most SpA patients preferred to be involved in decisions regarding their treatment, and although efficacy and safety are both considered essential, frequency and methods of administration also play a role as preference attributes for BA. These findings suggest that implementing management programs for SpA patients focused on the physical, emotional, and social consequences of the disease, in addition to assessing and including patient’s preferences in the treatment decision-making process, could be crucial in improving patients’ HRQoL and ensuring their satisfaction and compliance with treatment.
Acknowledgments
The abstract was presented at ISPOR Congress 2016. The full details of the reference are: Blanch C, Comellas M, de Paz HD, Lizan L. Patient reported outcomes in spondyloarthritis patients in Europe: a systematic review of the literature. Value Health; 19(7):A543.
Disclosure
This study was funded by Novartis Farmacéutica SA. CB works for Novartis Farmacéutica SA. MC and LL work for an independent research entity that received remuneration for development of the original research and writing this manuscript. The remaining authors report no conflicts of interest in this work.
References
- National Institute for Health and Care ExcellenceSpondyloarthritis in Over 16s: Diagnosis and ManagementLondonNICE2017
- RaychaudhuriSPRaychaudhuriSKMechanistic rationales for targeting interleukin-17A in spondyloarthritisArthritis Res Ther20171915128270233
- WendlingDTreating to target in axial spondyloarthritis: defining the target and the arrowExpert Rev Clin Immunol201511669169325905676
- StolwijkCBoonenAvan TubergenAReveilleJDEpidemiology of spondyloarthritisRheum Dis Clin North Am201238344147623083748
- GladmanDDAntoniCMeasePCleggDONashPPsoriatic arthritis: epidemiology, clinical features, course, and outcomeAnn Rheum Dis200564Suppl 2ii14ii1715708927
- LiuJTYehHMLiuSYChenKTPsoriatic arthritis: epidemiology, diagnosis, and treatmentWorld J Orthop20145453754325232529
- SinghJAStrandVSpondyloarthritis is associated with poor function and physical health-related quality of lifeJ Rheumatol20093651012102019369461
- LozaEJoverJARodriguezLCarmonaLMultimorbidity: prevalence, effect on quality of life and daily functioning, and variation of this effect when one condition is a rheumatic diseaseSemin Arthritis Rheum200938431231918336872
- al MainiMAdelowoFal SalehJThe global challenges and opportunities in the practice of rheumatology: white paper by the World Forum on Rheumatic and Musculoskeletal DiseasesClin Rheumatol201534581982925501633
- el MaghraouiAExtra-articular manifestations of ankylosing spondylitis: prevalence, characteristics and therapeutic implicationsEur J Intern Med201122655456022075279
- SmolenJSLandewéRBreedveldFCEULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 updateAnn Rheum Dis201473349250924161836
- BraunJvan den BergRBaraliakosX2010 Update of the ASAS/EULAR recommendations for the management of ankylosing spondylitisAnn Rheum Dis201170689690421540199
- GossecLSmolenJSGaujoux-VialaCEuropean League Against Rheumatism recommendations for the management of psoriatic arthritis with pharmacological therapiesAnn Rheum Dis201271141221953336
- SchoelsMKnevelRAletahaDEvidence for treating rheumatoid arthritis to target: results of a systematic literature searchAnn Rheum Dis201069463864320237123
- KavanaughACohenSCushJJThe evolving use of tumor necrosis factor inhibitors in rheumatoid arthritisJ Rheumatol200431101881188415468347
- HillJAdherence with drug therapy in the rheumatic diseases – part one: a review of adherence ratesMusculoskeletal Care200532617317041995
- BartonJLPatient preferences and satisfaction in the treatment of rheumatoid arthritis with biologic therapyPatient Prefer Adherence2009333534420016797
- HigginsJPGreenSCochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0LondonCochrane Collaboration2011
- Centre for Evidence-Based Medicine [homepage on the Internet] Available from: https://www.cebm.netAccessed March 26, 2018
- SalaffiFCarottiMGaspariniSIntorciaMGrassiWThe health-related quality of life in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis: a comparison with a selected sample of healthy peopleHealth Qual Life Outcomes200972519296831
- JajićZRajnprehtIKovačićNWhich clinical variables have the most significant correlation with quality of life evaluated by SF-36 survey in Croatian cohort of patient with ankylosing spondylitis and psoriatic arthritis?Rheumatol Int201232113471347922065069
- KotsisKVoulgariPVTsifetakiNAnxiety and depressive symptoms and illness perceptions in psoriatic arthritis and associations with physical health-related quality of lifeArthritis Care Res (Hoboken)201264101593160122556134
- HyphantisTKotsisKTsifetakiNThe relationship between depressive symptoms, illness perceptions and quality of life in ankylosing spondylitis in comparison to rheumatoid arthritisClin Rheumatol201332563564423329349
- ChorusAMMiedemaHSBoonenAvan der LindenSQuality of life and work in patients with rheumatoid arthritis and ankylosing spondylitis of working ageAnn Rheum Dis200362121178118414644855
- KawalecPMalinowskiKPPilcADisease activity, quality of life and indirect costs of psoriatic arthritis in PolandRheumatol Int20163691223123027339273
- HromadkovaLSoukupTVlcekJQuality of life and drug compliance: their interrelationship in rheumatic patientsJ Eval Clin Pract201521591992426083391
- SaadAAAshcroftDMWatsonKDImprovements in quality of life and functional status in patients with psoriatic arthritis receiving anti-tumor necrosis factor therapiesArthritis Care Res (Hoboken)201062334535320391480
- SieperJHolbrookTBlackCMWoodRHuXKachrooSBurden of illness associated with non-radiographic axial spondyloarthritis: a multiperspective European cross-sectional observational studyClin Exp Rheumatol201634697598327749215
- WallmanJKKapetanovicMCPeterssonIFGeborekPKristensenLEComparison of non-radiographic axial spondyloarthritis and ankylosing spondylitis patients: baseline characteristics, treatment adherence, and development of clinical variables during three years of anti-TNF therapy in clinical practiceArthritis Res Ther201517137826703005
- KucharzEJKotulskaAKopeć-MędrekMWiduchowskaMOpinion of patients with ankylosing spondylitis on risk factors impairing their quality of lifeRheumatol Int201333112899290122983136
- Ariza-ArizaRHernández-CruzBNavarro-SarabiaFPhysical function and health-related quality of life of Spanish patients with ankylosing spondylitisArthritis Rheum200349448348712910553
- de las PeñasCFBlancoCAPérezAAPageJCRelationship among mobility, functionality and quality of life in subjects presenting with ankylosing spondylitisFisioterapia2006283143151
- Ariza-ArizaRHernández-CruzBLópez-AntequeraGNavarro-SarabiaFVariables related to utility in patients with ankylosing spondylitisClin Rheumatol200928220721118825472
- O’DwyerTO’SheaFWilsonFDecreased health-related physical fitness in adults with ankylosing spondylitis: a cross-sectional controlled studyPhysiotherapy2016102220220926119877
- TälliSEtchetoAFautrelBPatient global assessment in psoriatic arthritis: what does it mean? An analysis of 223 patients from the Psoriatic Arthritis Impact of Disease (PsAID) studyJoint Bone Spine201683333534026677994
- Puyraimond-ZemmourDEtchetoAFautrelBAssociations between five important domains of health and the patient acceptable symptom state in rheumatoid arthritis and psoriatic arthritis: a cross-sectional study of 977 patientsArthritis Care Res (Hoboken)201769101504150927998030
- BrodszkyVPéntekMBálintPComparison of the Psoriatic Arthritis Quality of Life (PsAQoL) questionnaire, the functional status (HAQ) and utility (EQ-5D) measures in psoriatic arthritis: results from a cross-sectional surveyScand J Rheumatol201039430330920166848
- CramerJARoyABurrellAMedication compliance and persistence: terminology and definitionsValue Health2008111444718237359
- López-GonzálezRLeónLLozaERedondoMde YébenesMJCarmonaLAdherence to biologic therapies and associated factors in rheumatoid arthritis, spondyloarthritis and psoriatic arthritis: a systematic literature reviewClin Exp Rheumatol201533455956925602291
- LyuRGovoniMDingQTreatment persistence among patients with rheumatoid disease (RA, AS, PsA) treated with subcutaneous biologics in GermanyRheumatol Int201636114315326314368
- SaadAAAshcroftDMWatsonKDPersistence with anti-tumour necrosis factor therapies in patients with psoriatic arthritis: observational study from the British Society of Rheumatology Biologics RegisterArthritis Res Ther2009112R5219356232
- KristensenLEKarlssonJAEnglundMPeterssonIFSaxneTGeborekPPresence of peripheral arthritis and male sex predicting continuation of anti-tumor necrosis factor therapy in ankylosing spondylitis: an observational prospective cohort study from the South Swedish arthritis treatment group registerArthritis Care Res (Hoboken)201062101362136920506310
- FavalliEGSelmiCBeccioliniAEight-year retention rate of first-line tumor necrosis factor inhibitors in spondyloarthritis: a multi-center retrospective analysisArthritis Care Res (Hoboken)201769686787427696735
- RenziCDi PietroCTabolliSParticipation, satisfaction and knowledge level of patients with cutaneous psoriasis or psoriatic arthritisClin Exp Dermatol201136888588821790723
- NollaJRodríguezMMartin-MolaEPatients’ and rheumatologists’ preferences for the attributes of biological agents used in the treatment of rheumatic diseases in SpainPatient Prefer Adherence2016101101111327382258
- RotheryCBojkeLRichardsonGA discrete choice experiment to explore patients’ willingness to risk disease relapse from treatment withdrawal in psoriatic arthritisClin Rheumatol201635122967297427796664
- SokkaTKautiainenHHannonenPPincusTChanges in Health Assessment Questionnaire disability scores over five years in patients with rheumatoid arthritis compared with the general populationArthritis Rheum200654103113311817009231
- van EchteldICiezaABoonenAIdentification of the most common problems by patients with ankylosing spondylitis using the international classification of functioning, disability and healthJ Rheumatol200633122475248317013999
- CarterRRiantawanPBanhamSWSturrockRDAn investigation of factors limiting aerobic capacity in patients with ankylosing spondylitisRespir Med1999931070070810581658
- OzdemyrOInaniciFHasçelikZReduced vital capacity leads to exercise intolerance in patients with ankylosing spondylitisEur J Phys Rehabil Med201147339139721364507
- HalvorsenSVøllestadNKFongenCPhysical fitness in patients with ankylosing spondylitis: comparison with population controlsPhys Ther201292229830922095208
- MarcoraSCasanovaFWilliamsEJonesJElamanchiRLemmeyAPreliminary evidence for cachexia in patients with well-established ankylosing spondylitisRheumatology200645111385138816603581
- ToussirotEMichelFWendlingDBone density, ultrasound measurements and body composition in early ankylosing spondylitisRheumatology (Oxford)200140888288811511757
- SaadAASymmonsDPMNoycePRAshcroftDMRisks and benefits of tumor necrosis factor-α inhibitors in the management of psoriatic arthritis: systematic review and metaanalysis of randomized controlled trialsJ Rheumatol200835588389018381787
- CurkendallSPatelVGleesonMCampbellRSZagariMDuboisRCompliance with biologic therapies for rheumatoid arthritis: so patient out-of-pocket payments matter?Arthritis Rheum200859101519152618821651
- HarleyCRFrytakJRTandonNTreatment compliance and dosage administration among rheumatoid arthritis patients receiving infliximab, etanercept, or methotrexateAm J Manag Care200396 SupplS136S14314577718
- BorahBJHuangXZarotskyVGlobeDTrends in RA patients’ adherence to subcutaneous anti-TNF therapies and costsCurr Med Res Opin20092561365137719425902
- CalipGSAdimadhyamSXingSRinconJCLeeWJAnguianoRHMedication adherence and persistence over time with self-administered TNF-alpha inhibitors among young adult, middle-aged, and older patients with rheumatologic conditionsSemin Arthritis Rheum201747215716428410817
- LizánLComellasMPazSPovedaJLMeleticheDPolancoCTreatment adherence and other patient-reported outcomes as cost determinants in multiple sclerosis: a review of the literaturePatient Prefer Adherence201481653166425525341
- van den BemtBJZwikkerHEvan den EndeCHMedication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literatureExpert Rev Clin Immunol20128433735122607180
- KravitzRLMelnikowJEngaging patients in medical decision makingBMJ2001323731358458511557690
- NotaIDrossaertCHTaalEVonkemanHEvan de LaarMAPatient participation in decisions about disease modifying anti-rheumatic drugs: a cross-sectional surveyBMC Musculoskelet Disord20141533325281209
