Abstract
Ageing populations with multiple chronic conditions challenge low-, middle-, and high-income countries. Older adults frequently depend on complex medication regimens and polypharmacy, both of which can lead to potentially devastating and debilitating medication-related problems and to subsequent far-reaching public health, social, and economic effects. This perspectives article provides an overview of the current state of medication management, reflects on its relevance among polymedicated home-dwelling older adults living with multiple chronic conditions, and proposes patient-centered approaches for optimizing medication management and preventing medication-related problems.
Ageing Populations with Multiple Chronic Conditions Challenge Low-, Middle-, and High-Income Countries
Ageing populations represent one of the most significant current challenges to the long-term sustainability and efficiency of the world’s healthcare and social services systems.Citation1 Despite increases in life expectancy, older adults are not experiencing better health than previous generations.Citation2 Worldwide, the prevalence of multimorbidity in older adults ranges from 55–98%Citation3 In Switzerland, 25.2% of adults aged from 65–79 years old, and 41.3% of those aged 80 or more, live at home with multimorbidity.Citation4 Three major operational definitions of multimorbidity co-exist in the literature: co-occurrence of at least two diseases in the same individual; cumulative indices considering both the number and severity of concurrent diseases; and the simultaneous presence of not only diseases but also their associated symptoms and physical and cognitive dysfunctions.Citation3 To properly cover the heterogeneity and complexity of older adults’ health statuses, this paper uses the term multiple chronic conditions to encompass all three definitions.Citation5 Older adults living with multiple chronic conditions present a poorer quality of life, declines in functional ability and mobility,Citation3 and shorter life expectancy, particularly those with cognitive impairment and/or cardiovascular disease.Citation6 The concept of multiple chronic conditions is also associated with increased psychological distress and repeated and prolonged hospitalizations.Citation3 Although the expanding number of patients with multiple chronic conditions is considered a public health concern, prevalence often remains unclear, especially given the absence of any consensual definition in ongoing epidemiological investigations. Nonetheless, regardless of the definition, multiple chronic health conditions among home-dwelling older adults have been strongly associated with polypharmacy and medication-related problems (MRPs) in multiple observational and epidemiological studies.Citation7,Citation8
Polypharmacy and Medication-Related Problems
Older people with multiple chronic conditions—particularly those with cognitive impairment and/or psychiatric disorders—frequently depend on complex medication regimens. A recent Swiss study reported that more than 80% of home-dwelling older adults took at least one drug daily, with some taking up to 17.Citation9 Indeed, 27% had a daily intake of five or more drugs, with numbers increasing with age: 18% of those aged 69–74, rising to 38% of those aged 85 or more. However, nearly 50% of older adults took at least one medication that was not medically required.Citation9
Although the use of multiple medicines or polypharmacy may be clinically appropriate in many cases, it is imperative to identify those older adults with inappropriate polypharmacy prescriptions that may put them at a greater risk of MRPs and adverse health outcomes.Citation10,Citation11 To distinguish between appropriate and inappropriate polypharmacy, Masnoon et al (2017) conducted a systematic literature review to explore the different definitions of polypharmacy.Citation12 They found 138 definitions of polypharmacy and associated terms. Although the most commonly used definition of polypharmacy is taking five or more medicines,Citation12 the variety of definitions could confuse clinicians in practice and make it difficult to assess the safety and appropriateness of a medication therapy in clinical settings. There is an urgent need for an international consensus definition of polypharmacy, including how to assess inappropriate polypharmacy, in order to optimize medication management and clinical follow-up and to enable precisely comparable criteria in research.
Regardless of polypharmacy’s definition, polymedicated older adults are more susceptible to MRPs, including adverse drug reactions, medication errors, and non-adherence, which often result in emergency department visits and hospitalizations.Citation10,Citation11 Up to 25% of emergency department visits by home-dwelling older adults with multiple chronic conditions are attributable to an MRP.Citation13 Nonetheless, 60% of MRPs in older patients visiting emergency departments with non-specific signs and symptoms (such as weakness) may go undiagnosed as such, whereas 83% of those MRPs may be accountable for acute morbidity.Citation13 MRPs also frequently result in readmission: in one study following older patients for six months after hospital discharge, they were the most frequent cause.Citation14 Evidence suggests that the risk of an MRP increases not only with age and the number of comorbidities but also with the number of medications prescribed and with certain classes of drugs, such as medicines for cardiovascular diseases and diabetes.Citation11,Citation13 Thus, MRPs can lead to a degradation in the patient’s clinical condition, physical and cognitive decline, an exacerbation of chronic medical conditions, and avoidable health costs.Citation13,Citation15 MRPs can be devastating and debilitating for older people, and they can have far-reaching public health, social, and economic impacts.
A possible explanation for high numbers of MRPs is that most clinical guidelines and intervention care models were designed using short-term randomized controlled trials involving single health conditions. This contrasts with the current reality of the multiple, chronic, and often interacting health conditions affecting older people. Trying to implement multiple clinical guidelines for a single disease among older adults with multiple chronic conditions may result in contradictory and potentially harmful recommendations.Citation16 The pathophysiological processes, clinical features, and interactions of age-related conditions must be disentangled, as much as possible, in order to personalize medication and its management and to realign older adults, caregivers, and healthcare systems so as to prevent MRPs.
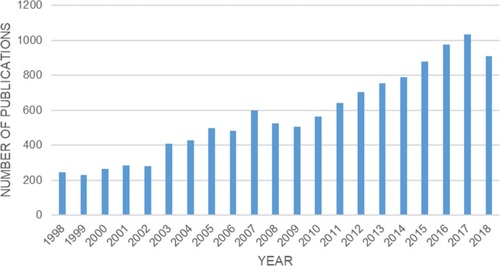
Due to the high prevalence of polypharmacy and MRPs, together with their impact on older adults’ quality of life and public healthcare expenditure, medication management has emerged as a priority in clinical settings. Its necessity among older adults has also become the focus of considerable research interest and media attention over the last decade (). However, the mechanisms behind poor medication management are not well defined.
Figure 1 Papers referenced in Pubmed over the last 20 years on medication management among older adults.
The present paper provides a timely addition to the burgeoning body of evidence offering new perspectives on our understanding of medication management—well beyond the act of medical prescription itself—among polymedicated home-dwelling older adults with multiple chronic conditions.
Optimizing Medication Use Among Older Adults with Multiple Chronic Conditions
MRPs are a reflection of the complexity of dealing with polypharmacy and age-related multiple chronic conditions; they are causally underpinned by interacting and often unclear pathophysiological, pharmacodynamic, and pharmacokinetic processes. Furthermore, the signs of a normal ageing process are not always easy to tell apart from the potential pathophysiological deviations induced by underlying chronic conditions.Citation17,Citation18 The occurrence of MRPs is strongly affected by a broad range of factors and determinants, which are not confined to single biological systems or human health domains.Citation17 Environmental and social factors also substantially influence MRPs.Citation11
MRPs are nonetheless preventable with appropriate, well-coordinated primary care.Citation11,Citation13,Citation19 For example, 20–30% of avoidable older adult readmissions have been directly related to non-adherence.Citation20 Some of the current evidence-based strategies for medication safety and the prevention of MRPs include medication reconciliation, systematic review of prescribed medications, deprescribing, and electronic medication management systems.Citation21,Citation22
Medication reconciliation is a well-documented good practice corresponding to the process of creating and updating a single list of an older adult’s medication;Citation23 this ensures a systematic, comprehensive review of all the patient’s current medicines. Prior research has shown that discharge letters received by primary care professionals are frequently inaccurate and lack key information.Citation24 Regular medication reconciliation reduces medication errors by consistent communication across transitions of care, including changes in the clinical setting, medical practitioner, or level of care.Citation25
Regularly and systematically reviewing prescribed medications is a straightforward, effective means of reducing inappropriate prescribing and, therefore, a preventive strategy for avoiding MRPs. Inappropriate prescribing includes potentially inappropriate medications and potential prescribing omissions. Existing screening tools—such as the STOPP/START criteria (Screening Tool of Older Persons’ Prescriptions/Screening Tool to Alert to Right Treatment) —recognize the dual nature of inappropriate prescribing by including a list of potentially inappropriate medications (STOPP criteria) and potential prescribing omissions (START criteria).Citation26 Complementary to this, the American Geriatrics Society Beers Criteria is a list of potentially inappropriate medications that it is preferable for older adults to avoid in most situations or particular health conditions.Citation27
Deprescribing attempts to balance the potential benefits and harms of tapering or ceasing inappropriate medication with the aim of managing polypharmacy and improving outcomes.Citation28 Deprescribing is particularly relevant among frail older adults with multiple chronic conditions, as they face high risks of MRPs, hospitalization, and early death.Citation21
Electronic medication management systems are recent digital developments covering prescriptions, administration, pharmacy reviews, medication administration using barcodes, and all the electronic devices devoted to medication management processes.Citation22 Electronic medication management systems contribute to reducing medication errors and enhancing interprofessional collaboration and patient safety by using red flag strategies.Citation29,Citation30 In recent years, smartphone applications for optimizing medication use have also emerged. However, older adults, who can experience the greatest benefits from more electronic support to improve their medication use, are also the least accustomed to using them.Citation21
Integrating Older Adults’ Preferences into Medication Management
Preventability and an understanding of risk factors are crucial to co-constructing interventions to minimize MRPs.Citation11,Citation19 However, research about MRPs and medication management currently focuses on healthcare professionals’ perspectives, to which the perspectives and experiences of patients and informal caregivers are often secondary. Research into medication management has evolved with little consideration of the perspectives and preferences of older adults themselves. Further studies—using qualitative or mixed research designs—will be essential to identify the logic which home-dwelling older adults with multiple chronic conditions apply to the management of their daily medication and how they integrate it into the rhythm of their daily lives and home environments.Citation14,Citation19 Shared decision-making must be promoted, notably via operational tools providing information on the benefits and risks of medicines in a format which older adults can embrace more easily.Citation31 Even though empowering patients to participate in their medication management has beneficial effects—particularly in medication adherenceCitation32—the concept of older adult empowerment and self-management of complex medication regimens, along with their impact on MRPs, has been poorly investigated. Quasi-experimental studies and randomized controlled trials will be essential for any adequate exploration of the effectiveness of innovative interventions aiming to empower older adults’ medication management, improve their competences, and enhance shared decision-making with healthcare professionals.
The Roles and Accountability of Healthcare Professionals
The complexity of care required by home-dwelling older adults with multiple chronic conditions leads them to be significant users of healthcare services and to consult many different healthcare professionals.Citation33 Medication management among this population consequently requires interprofessional collaboration across different healthcare and social services providers and organizations.Citation16 Besides prescribers, usually general practitioners and different specialist physicians, pharmacists, nurses, and other allied health professionals may be involved in and accountable for medication management.Citation16 In Australia, collaborative home medicines reviews (involving a general practitioner and a pharmacist) have demonstrated their effectiveness in detecting, preventing, and resolving MRPs among home-dwelling older adults with multiple chronic conditions.Citation16 Furthermore, adherence to prescribed medication can also be improved by pharmacist- and nurse-led interventions.Citation34–Citation37 However, the higher the number of healthcare professionals consulted by home-dwelling older adults with multiple chronic conditions, the greater the chance that care may be fragmented and uncoordinated.Citation16 This can be explained by the different treatment preferences of different healthcare professionals. Home-dwelling older adults with multiple chronic conditions often fail to receive the efficient, effective, and coordinated care that they could gain so much from.Citation38,Citation39 Failure to coordinate care for home-dwelling older adults with multiple chronic conditions undeniably increases the risk of MRPs.Citation16 Those who consult three or more healthcare professionals report receiving conflicting advice, which makes it difficult for them to know which guidance they should follow. Inadequate explanations about medication result in omissions and incorrect dosages, but also in anxiety and confusion in older adults.Citation40 Healthcare professionals should feel accountable for optimizing medication management among home-dwelling older adults, particularly during their transitions home from acute care settings. Implementing effective primary care management should be a priority among home-dwelling older adults with multiple chronic conditions in order to prevent adverse health outcomes and to promote autonomy in their daily lives. Older adults at a high risk of MRPs should systematically be assigned a primary care manager whose aim is to meet their needs with regards to prevention and chronic conditions. By using planned interactions and ensuring appropriate follow-up, primary care managers can contribute significantly to the prevention of hospital admissions, rehospitalizations, institutionalization in nursing homes, and early death.Citation41,Citation42
The Role of Informal Caregivers
In addition to healthcare professionals’ contributions to medication management, informal caregivers help to ensure safe, appropriate medication use at home by older adults with multiple chronic conditions, notably among those who may also have cognitive impairment.Citation43–,Citation45 Although the role of informal caregivers in medication management is very relevant, various constraints have been reported regarding the time required, anxiety about making mistakes, and the uncollaborative behavior of older adults.Citation46 They also face difficulties maintaining continuous supplies of medicines, supporting administrative work, making clinical decisions, and handling conflicts or disagreements with the older adult,Citation46 or even with healthcare professionals in regards to ineffective medicinal practices.Citation43,Citation46 Although several studies have furthered understanding about the daily challenges faced by informal caregivers managing medication for older adults, there has been less insight into any educational or training interventions aimed at improving caregivers’ medication management competences. More studies are required to explore how to efficiently support informal caregivers in their roles as medication managers. Psychoeducation, digital applications, or specialized counselling services provided by pharmacists or advanced practice nurses should also be considered.Citation44,Citation45,Citation47 Cooperating with informal caregivers and integrating their experiences of shared decision-making should be one of the tasks assigned to primary healthcare professionals. To make this a reality, they could receive backing from their hierarchies and perhaps even financial incentives to support informal caregivers in the optimization of medication management. More research will be needed to analyze the effectiveness of such incentives.
Ways to Bridge the Gap
Optimal medication management is one of the basic preconditions for home-dwelling older adults with multiple chronic conditions to be able to remain at home and preserve their quality of life.Citation7,Citation48 Improving medication management for them not only requires regular monitoring of MRPs and reviewing of prescriptions to eliminate unnecessary medication but also coordinated care by different healthcare and social services providers.Citation49 This calls for an integrated, multi-stakeholder model to optimize medication management among home-dwelling older adults with multiple chronic conditions. Such a medication management model should be rigorously structured using a care model process embracing development, implementation, and sustainability milestones.Citation50 It should also consider the quadruple aim of enhancing the patient’s experience, improving population health, reducing costs, and improving healthcare professionals’ working lives.Citation51 Indeed, both these frameworks underpin the ongoing mixed-methods research by Pereira et al, which brings together retrospective and prospective findings to promote medication management and prevent MRPs.Citation52 Such a model should be able to more adequately capture the biological, clinical, psychosocial, and pharmacological complexities of multiple chronic conditions and polypharmacy. A robust, integrated, multi-stakeholder model that embeds care in the context of where and how older adults with multiple chronic conditions live needs to be developed to prevent the onset and/or progression of MRPs.
Disclosure
This work was supported by the Swiss National Science Foundation’s National Research Programme 74 [407440_183434/1]. Prof. Dr. Armin von Gunten reports grants from the National Research Foundation, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- European Innovation Partnership on Active and Healthy Ageing. ACTION PLAN on ‘Innovation for Age-friendly buildings, cities & environments' Brussels: European Commission; 2012.
- World Health Organization. Global Strategy and Action Plan on Ageing and Health. Geneva: World Health Organization;2017 978-92-4-151350-0.
- Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10:430–439. doi:10.1016/j.arr.2011.03.00321402176
- Bachmann N, Burla L, Kohler D, et al. La santé en Suisse-Le point sur les maladies chroniques: rapport national sur la santé. Retrieved from Berne: & older people’s experiences of medicine changes on leaving hospital. Res Social Adm Pharm. 2015;10:791–800.
- Valderas JM, Starfield B, Sibbald B, Salisbury C, Rloand M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7:357–363. doi:10.1370/afm.98319597174
- Caughey GE, Ramsay EN, Vitry AI, et al. Comorbid chronic diseases, discordant impact on mortality in older people: a 14-year longitudinal population study. J Epidemiol Community Health. 2010;64:1036–1042. doi:10.1136/jech.2009.08826019854745
- Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13:57–65. doi:10.1517/14740338.2013.82766024073682
- Díez-Manglano J, Giménez-López M, Garcés-Horna V, et al. Excessive polypharmacy and survival in polypathological patients. Eur J Clin Pharmacol. 2015;71:733–739. doi:10.1007/s00228-015-1837-825911439
- Renard D, Fustinoni S, Seematter-Bagnoud L, Santos-Eggimann B. Médicaments chez les seniors vaudois à domicile : nombre et composition [Medicines for senior citizens of Vaud at home: number and composition]. Lausanne: Centre d’Observation et d’Analyse du Vieillissement; 2015. French.
- Monégat M, Sermet C. La polymédication définitions, mesures et enjeux: revue de la littérature et tests de mesure [Polymedication definitions, measures and issues: literature review and measurement tests. Health economics issues]. Questions d'économie de la santé. 2014;204. French.
- Al Hamid A, Ghaleb M, Aljadhey H, Aslanpour Z. A systematic review of hospitalization resulting from medicine-related problems in adult patients. Br J Clin Pharmacol. 2014;78:202–217. doi:10.1111/bcp.2014.78.issue-224283967
- Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17:1–10. doi:10.1186/s12877-017-0621-228049446
- Nickel CH, Ruedinger JM, Messmer AS, et al. Drug - related emergency department visits by elderly patients presenting with non-specific complaints. Scand J Trauma Resusc Emerg Med. 2013;21:15. doi:10.1186/1757-7241-21-1523497667
- Bonnet-Zamponi D, D’Arailh L, Konrat C, et al. Drug-related readmissions to medical units of older adults discharged from acute geriatric units: results of the optimization of medication in AGEd multicenter randomized controlled trial. J Am Geriatr Soc. 2013;61:113–121. doi:10.1111/jgs.2013.61.issue-123252914
- Fallis BA, Dhalla IA, Klemensberg J, Bell CM. Primary medication non-adherence after discharge from a general internal medicine service. PLoS One. 2013;8(5):e61735. doi:10.1371/journal.pone.006173523658698
- Gilbert A, Roughead L, McDermott R, et al. Multiple chronic health conditions in older people: implications for health policy planning, practitioners and patients; 2013 Available from: https://www.unisa.edu.au/siteassets/episerver-6-files/global/health/sansom/documents/qumprc/multiple-chronic-health-conditions.pdf. Accessed 1129, 2019.
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–762. doi:10.1016/S0140-6736(12)62167-923395245
- Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397. doi:10.1016/j.jamda.2013.03.02223764209
- Pellegrin KL, Lee E, Uyeno R, Ayson C, Goo R. Potentially preventable medication-related hospitalizations: a clinical pharmacist approach to assessment, categorization, and quality improvement. J Am Pharm Assoc. 2017;57:711–716. doi:10.1016/j.japh.2017.06.019
- Tang VL, Halm EA, Fine MJ, Johnson CS, Anzueto A, Mortensen EM. Predictors of rehospitalization after admission for pneumonia in the veterans affairs healthcare system. J Hosp Med. 2014;9:379–383. doi:10.1002/jhm.v9.624648401
- Molokhia M, Majeed A. Current and future perspectives on the management of polypharmacy. BMC Fam Pract. 2017;18:1–9. doi:10.1186/s12875-017-0642-028073347
- Pearce R, Whyte I. Electronic medication management: is it a silver bullet? Aust Prescr. 2018;41(2):32–33. doi:10.18773/austprescr.2018.01229670307
- Almanasreh E, Moles R, Chen TF. The medication reconciliation process and classification of discrepancies: a systematic review. Br J Clin Pharmacol. 2016;82(3):645–658. doi:10.1111/bcp.v82.327198753
- Mekonnen AB, McLachlan AJ, Brien JA. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: a systematic review and meta-analysis. BMJ Open. 2016;6(2):e010003. doi:10.1136/bmjopen-2015-010003
- IHI. How-To Guide: Prevent Adverse Drug Events by Implementing Medication Reconciliation. Cambridge, MA: Institute for Healthcare Improvement; 2011.
- O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–218. doi:10.1093/ageing/afu14525324330
- Fick DM, Semla TP, Steinman M, et al. American geriatrics society 2019 updated ags beers criteria(R) for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–694.30693946
- Page AT, Potter K, Clifford R, Etherton-Beer C. Deprescribing in older people. Maturitas. 2016;91:115–134. doi:10.1016/j.maturitas.2016.06.00627451330
- Kallio S, Kumpusalo-Vauhkonen A, Järvensivu T, Mäntylä A, Pohjanoksa-Mäntylä M, Airaksinen M. Towards interprofessional networking in medication management of the aged: current challenges and potential solutions in Finland. Scand J Prim Health Care. 2016;34:368–376. doi:10.1080/02813432.2016.124905527822968
- Shah K, Lo C, Babich M, Tsao NW, Bansback NJ. Bar code medication administration technology: a systematic review of impact on patient safety when used with computerized prescriber order entry and automated dispensing devices. Can J Hosp Pharm. 2016;69(5):394–402. doi:10.4212/cjhp.v69i5.159427826157
- Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–1367.22618581
- Náfrádi L, Nakamoto K, Schulz PJ. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS One. 2017;12:10. doi:10.1371/journal.pone.0186458
- Roughead EE, Vitry AI, Caughey GE, Gilbert AL. Multimorbidity, care complexity and prescribing for the elderly. Aging Health. 2011;7:695–705. doi:10.2217/ahe.11.64
- Mehuys E, Dupond L, Petrovic M, et al. Medication management among home-dwelling older patients with chronic diseases: possible roles for community pharmacists. J Nutr Health Aging. 2012;16:721–726. doi:10.1007/s12603-012-0028-x23076515
- Willis JS, Hoy RH, Jenkins WD. In-home medication reviews: a novel approach to improving patient care through coordination of care. J Community Health. 2011;36:1027–1031. doi:10.1007/s10900-011-9405-321499935
- Verloo H, Chiolero A, Kiszio B, Kampel T, Santschi V. Nurse interventions to improve medication adherence among discharged older adults: a systematic review. Age Ageing. 2017;46:747–754. doi:10.1093/ageing/afx07628510645
- Hannou S, Voirol P, Pannatier A, et al. Pharmacist intervention acceptance for the reduction of potentially inappropriate drug prescribing in acute psychiatry. Int J Clin Pharm. 2017;39:1228–1236. doi:10.1007/s11096-017-0513-828905171
- Salisbury C, Salisbury C, Johnson L, et al. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011. doi:10.3399/bjgp11X548929
- Boyd CM, Fortin M. Future of multimorbidity research: how should understanding of multimorbidity inform health system design? Public Health Rev. 2010;32(2):451.
- Knight DA, Thompson D, Mathie E, Dickinson A. Seamless care? Just a list would have helped!’Older people and their carer’s experiences of support with medication on discharge home from hospital. Health Expectations. 2013;16:277–291. doi:10.1111/hex.2013.16.issue-321838834
- Parsons M, Senior H, Kerse N, et al. Should care managers for older adults be located in primary care? A randomized controlled trial. J Am Geriatr Soc. 2012;60(1):86–92. doi:10.1111/jgs.2012.60.issue-122239292
- Available from: <Chapter 38_medication reconciliation.pdf>. Accessed 1129, 2019.
- O’Quin KE, Semalulu T, Orom H. Elder and caregiver solutions to improve medication adherence. Health Educ Res. 2015;30:323–335. doi:10.1093/her/cyv00925725500
- Gillespie R, Mullan J, Harrison L. Managing medications: the role of informal caregivers of older adults and people living with dementia. A review of the literature. J Clin Nurs. 2014;23:3296–3308. doi:10.1111/jocn.2014.23.issue-23pt2424354583
- Look KA, Stone JA. Medication management activities performed by informal caregivers of older adults. Res Social Adm Pharm. 2017.
- Reinhard SC, Levine C, Samis S. Home alone: family caregivers providing complex chronic care. BMJ. 2012:41.
- Pohontsch NJ, Loffler A, Luck T, et al. Informal caregivers’ perspectives on health of and (potentially inappropriate) medication for (relatively) independent oldest-old people - a qualitative interview study. BMC Geriatr. 2018;18(1):169. doi:10.1186/s12877-018-0849-530045689
- Williams GC, Patrick H, Niemiec CP, et al. Reducing the health risks of diabetes. Diabetes Educ. 2009;35:484–492. doi:10.1177/014572170933385619325022
- Höpflinger F, Bayer-Oglesby L, Zumbrunn A. La dépendance des personnes âgées et les soins de longue durée. Cahier de l’Observatoire suisse de la santé. 2011;135 Höpflinger F, Bayer-Oglesby L, Zumbrunn A. La dépendance des personnes âgées et les soins de longue durée [Elderly dependency and long-term care]. Bern: Observatoire Suisse de la Santé; 2011. French.
- ACI. Understanding the Process to Develop a Model of Care: An ACI Framework. Chatswood: Agency for Clinical Innovation; 2013.
- Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. doi:10.1370/afm.171325384822
- Pereira F, Roux P, Santiago-Delefosse M, et al. Optimising medication management for polymedicated home-dwelling older adults with multiple chronic conditions: a mixed-methods study protocol. BMJ Open. 2019;9(10):e030030. doi:10.1136/bmjopen-2019-030030
