Abstract
Purpose
Medication nonadherence is one of the most significant obstacles to tuberculosis (TB) control worldwide. Identification of the factors associated with medication nonadherence is important. However, few related studies have been carried out in Tibet. This study aimed to explore factors influencing medication nonadherence to pulmonary TB (PTB) treatment in Tibet, China, from the patient perspective.
Patients and Methods
In this qualitative study, seventeen PTB patients in Tibet were recruited by purposive and maximum variation sampling methods. In-depth semistructured interviews were conducted to collect data on factors influencing medication nonadherence, and Colaizzi’s seven-step method was used to analyze the data.
Results
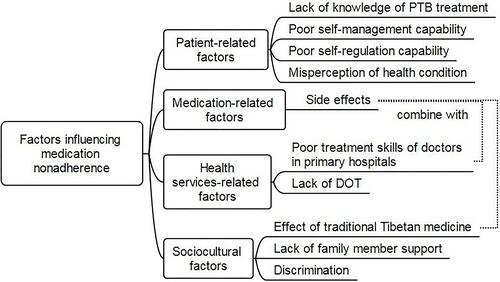
The medication nonadherence of PTB patients in Tibet was influenced by one or a combination of the following four factors. First, patient-related factors included a lack of knowledge of PTB treatment, poor self-management capability, poor self-regulation capability and misperception of health condition. Second, a medication-related factor was medication side effects. Third, health service-related factors included the poor treatment skills of doctors in primary hospitals and a lack of directly observed treatment (DOT). Last, sociocultural factors included the effect of traditional Tibetan medicine, lack of family member support and discrimination.
Conclusion
Multiple interplaying factors influenced medication nonadherence during PTB treatment in Tibet, and the main influencing factors were a lack of knowledge about PTB treatment, poor self-management capability, and the effect of traditional Tibetan medicine. TB health workers in Tibet should provide permanently viewable PTB treatment knowledge materials to PTB patients when oral health education is conducted, find feasible alternative strategies to DOT and establish links to traditional Tibetan medicine hospitals.
Introduction
Although the incidence and mortality rates of tuberculosis (TB) are slowly decreasing globally, TB remains a major challenge for public health, with an estimated 10 million new cases and 1.24 million deaths worldwide in 2018.Citation1 China is one of the 30 countries with the highest TB burdens. In 2018, there were 866,000 new cases of TB in China, which was the second highest number of new cases in the world, and 37,000 patients died.Citation1 In the Tibet Autonomous Region, located in Southwest China, the prevalence rate of pulmonary TB (PTB) was 758 per 100,000 in 2014, which is almost twice the national average.Citation2
However, TB treatment is an arduous undertaking for patients. Standard TB treatment requires the regular use of complex combined drugs for 6 to 8 months or longer.Citation3 Such long-term, strict regimens lead to nonadherence to prescribed drugs. Therefore, directly observed treatment (DOT), which requires patients to take medicine under the observation of health workers or family members, is the key strategy recommended by the World Health Organization (WHO) to improve medication adherence in TB patients.Citation3 The DOT short course (DOTS) strategy has been implemented in China since 1991 and had begun to be implemented throughout the whole country by 2005.
Nevertheless, because of difficulties in carrying out DOT in many parts of China, over half of TB patients now take drugs by themselves.Citation5 The national TB survey reported that 25.3% of TB patients missed more than one dose of anti-TB drugs.Citation6 In Shigatse, a city in the Tibet Autonomous Region, the rate of default from TB treatment was 28% in 2016,Citation7 which was higher than the WHO recommendation of less than 10%.Citation8 Medication nonadherence has been an important driver of TB drug resistance in Tibet and has resulted in treatment failure, disease relapse, prolonged infection, and even death.Citation4,Citation7,Citation9 It is also one of the most significant obstacles to TB control worldwide.Citation10
Different studies have shown that there are many factors influencing medication nonadherence among PTB patients. A study conducted in five provinces of China reported that a lack of DOT and adverse effects were associated with medication nonadherence.Citation11 However, studies carried out in other provinces and cities in China found that not only adverse effects but also financial burdens and social stigma led to medication nonadherence.Citation12–Citation14 Studies implemented in Shandong Province and Shenzhen City showed that being older, being depressed, lacking knowledge on TB treatment, having a longer treatment time and having a longer travel time to the nearest community health center were also related to medication nonadherence.Citation15,Citation16 Studies conducted in Iran and Ethiopia reported other patient-related factors, such as low self-efficacy, lack of a perceived threat, lack of perceived benefits, perceived barriers and forgetfulness.Citation17,Citation18 Social risk factors, such as social deprivation, vulnerable housing, mental health concerns or other comorbidities, also contributed to medication nonadherence.Citation19
Taken together, the above studies indicate that different factors are related to medication nonadherence in different regions. Hence, identifying specific factors that contribute to medication nonadherence to PTB treatment in different settings is important to design appropriate interventions to improve adherence. However, few related studies have been carried out in the Tibet Autonomous Region.
Thus, this qualitative study was conducted as an initial attempt to explore factors influencing medication nonadherence to PTB treatment from the patient perspective in Tibet, China, and to provide a basis for formulating targeted measures to improve medication adherence in the region and similar locations in low- and middle-income countries with a high TB burden.
Methods
Study Design
Using a phenomenological approach of the qualitative research, in-depth semistructured interviews were conducted to collect data on factors influencing medication nonadherence. Medication nonadherence was defined as missing more than 10% of prescribed anti-TB drug doses according to the National Tuberculosis Control Program implementation guide in China.Citation3
Study Setting
The Tibet Autonomous Region is located in Southwest China and contains seven cities. Over 90% of the residents of the Tibet Autonomous Region are ethnic Tibetans whose mother language is Tibetan. The participants were recruited from the Third People’s Hospital of the Tibet Autonomous Region, which is the province-level designated TB hospital.
Participants
Purposive and maximum variation sampling was used to select PTB patients who could provide the richest information. Patients’ medication adherence status, treatment status and geographic locations were mainly considered to provide a diverse sample. First, regarding medication adherence status, both PTB patients with adherence and those with nonadherence to the prescribed medicine were selected. Those patients who missed <10% of the total prescribed anti-TB drug doses were considered to exhibit medication adherence, while those who missed ≥10% of the total prescribed anti-TB drug doses were considered to exhibit medication nonadherence. Missing doses were reported by the patients, and the total number of prescribed doses was checked by the research team in the information system of the Third People’s Hospital of the Tibet Autonomous Region. Second, regarding treatment status, both PTB patients who were under initial treatment and those who were under retreatment were selected. Treatment status was assessed by TB doctors in the Third People’s Hospital of the Tibet Autonomous Region according to the definitions in the National TB Control Program implementation guide in China.Citation3 Third, regarding geographic location, PTB patients were chosen from different cities of Tibet, including Lhasa, Naqu, Shigaze, Shannan, Changdu, and Ali. Both patients living in urban areas and those living in rural areas were recruited.
The study inclusion criteria were as follows: duration of taking anti-tuberculosis drugs of at least one month and age between 15 and 60 years. In addition to PTB patients who were not able to speak Mandarin Chinese and those who did not agree to participate in this study, PTB patients with other diseases, such as diabetes, autoimmune deficiency syndrome (AIDS), malignant tumors and serious heart, brain, liver and kidney diseases, were excluded because they need to take drugs against diseases other than PTB, which may affect their memories of taking anti-TB drugs and the accuracy of the results.
The registry books at the Third People’s Hospital of the Tibet Autonomous Region were used to recruit participants. Out of 2044 registered TB patients between June 1, 2018, and June 30, 2019, 169 patients met the inclusion criteria and were able to be contacted. The number of participants was determined based on the principle of information saturation, which refers to when no new information can be found. After each interview, a preliminary analysis of the data was conducted to determine the next participant who would be recruited to obtain maximum information. The recruitment process was halted when there was an indication of information saturation. Finally, 17 PTB patients participated in this study, and none withdrew from the study. The 17 participants are numbered in Arabic numerals 1–17.
Interviewers
The interviewer was the first author of this article, who was not involved with clinical care at the study hospital. She was systematically trained in qualitative research by a professor for two years and had extensive interviewing experience among TB patients and medical staff. Her mother language is Mandarin Chinese. Two trained medical undergraduates, who are ethnic Tibetans but proficient in Mandarin Chinese, served as the recorders for this study. They were mainly responsible for text recording and audio recording interviews on site and for carefully observing the participants’ nonverbal behavior. When the participants spoke in dialect, the two undergraduates translated into Mandarin Chinese for the interviewer. The interviewer and the participant did not know each other before the study began, and they interacted with each other after the participant was recruited and gradually built a rapport.
Data Collection
An interview outline, which is shown in , was used to collect data. It was designed based on an extensive review of the literature and guidance of a TB expert who has worked in Tibet for 26 years. In June 2019, three participants were selected for pilot interviews. After the pilot interviews, the interview outline was revised according to analysis results of pilot interview data and suggestion of the TB expert.
Table 1 Interview Outline of Factors Influencing Medication Nonadherence to PTB Treatment in Tibet
In-depth, semistructured interviews were conducted to collect data. The formal interviews were conducted from July 11–31, 2019. Only one participant was interviewed in each interview. Ten of the seventeen participants were interviewed face to face in a single room at the pulmonary department at the Third People’s Hospital of the Tibet Autonomous Region. The interview room was private and quiet. When the interview was conducted, only the interviewer, the participant and one recorder were in the interviewing room. The other seven participants were interviewed by video with WeChat (a social software that is widely used in China) because it was not convenient for them to come to the hospital, and they determined the interview time and place on their own.
Participation in the interviews was voluntary and confidential, and the researchers strove to make participation convenient for the participants. The interviewer and participants communicated in Chinese. The interviewer explained the purpose, process, necessity of recording and confidentiality of the interview. After informed consent of the participant was obtained, the interview started. The initial questions gathered data on participant characteristics including gender, age, education level, occupation, marital status, and place of residence. The subsequent questions focused on reasons for medication nonadherence or adherence. According to the participants’ answers and the interview outline, further questions were asked to obtain rich information from the participants. Each interview lasted for 30–40 minutes. Two participants were re-interviewed to supplement the data.
Data Analysis
According to uniform format and the principle of not missing a word, timeliness and double backup, the audio recordings were transcribed by six uniformly trained research team members. One audio recording was transcribed by two members, one of whom was the interviewer or the recorder. The two copies were then compared for consistency, and inconsistencies were modified according to the audio recording and text recording on site.
Colaizzi’s seven-step method was used to analyse the data. The researchers repeatedly and carefully read the transcripts. Then, significant statements were extracted from the transcribed data, and recurring viewpoints were coded. A total of 157 codes were aggregated into 10 subcategories, which were then consolidated into 4 categories. Four researchers analyzed the same data repeatedly and compared the results with the original data. Disagreements were discussed among the researchers to reach a final consensus. The principal researcher reconnected with the participants by phone and asked whether the results were consistent with their experiences. Data analysis was conducted in Chinese, and the results were translated into English. The software NVivo 12 (QSR International, Melbourne, Australia) was used to manage and analyse the data.
Results
All participants were all ethnic Tibetans and Tibetan Buddhists. The average age was 30.1 years old (range: 15–65 years). Their characteristics are shown in .
Table 2 Characteristics of the Participants (n=17)
From the participant perspective, factors influencing medication nonadherence to PTB treatment in Tibet included four aspects: patient-related factors, medication-related factors, health service-related factors and sociocultural factors. Some participants reported more than one factor. Financial burden was a factor noted by all the participants, but none stopped taking their medication because of financial burden. The results are shown in .
Patient-Related Factors
Patient-related factors include a lack of knowledge of PTB treatment, poor self-management capability, poor self-regulation capability and misperception of health condition, and the first two factors play the most important role in medication nonadherence.
Lack of Knowledge of PTB Treatment
All ten noncompliers lacked knowledge of PTB treatment. Seven of them did not know that the duration of taking medication was at least six months or longer. Six of them were unaware of the dangers of not taking their medication consistently. Therefore, they stopped taking their medication any time they wanted to. Some participants believed that PTB was incurable. Therefore, they thought it was not necessary for them to continue taking medicine. However, all of the participants admitted that their doctors had told them knowledge of PTB treatment.
“I thought maybe I should take it (the medication) for three months, three months. So, I took it for three months.” (participant 5)
“I have interrupted (the use of the medication) many times and not felt discomfort, so it is nothing if you interrupt the medicine.” (participant 1)
“Some people say that, after I took medication for a period, some people say that it (PTB) can’t be cured at all. It doesn’t make sense to keep taking medicine.” (participant 4)
In contrast, all the seven compliers had adequate knowledge of TB treatment.
“I haven’t forgotten even a single pill. I know that if I do not insist on taking medicine what the bad consequences would be. One of my relatives forgot to take the medicine and relapsed.” (participant 8)
Poor Self-Management Capability
Seven of the ten noncompliers interrupted the use of the medication because of their poor self-management capability. They could not deal with the relationship between taking medication and life events, such as the death of a family member, pregnancy and busy work. Two pregnant women continued to take medication after giving birth, but they still often forgot to take the medication after reminders from their family members.
“My mother died, and I needed to bury her, so for more than half a month, I did not take the medicine.” (participant 1)
“When I had taken the medication for 5 months, there was a fetus in my belly, and someone told me that the medicine was not good for the fetus, so I stopped. After the baby was born, Dad kept reminding me to take my medicine, but … … but, sometimes I still forgot it.” (participant 7)
“There are too many things for my job; sometimes I take the medicine at ten o’clock in the morning (dawn is at approximately 9 a.m. in Tibet), sometimes in the afternoon, sometimes at 11 at night. Sometimes I have to work overtime at night, and I am very tired when I get home; I just want to go to bed as soon as possible, and I do not eat.” (participant 12)
“This summer, I finished the medicine (that I had) but had no time to go to the epidemic prevention station (the previous name of the Center for Disease Control and Prevention) to pick up (additional) medicine; work is too busy.”(participant 10)
In contrast, three of the seven compliers never interrupted the use of the medication because of their excellent self-management capability. They overcame all sorts of difficulties and took their medication according to the doctor’s instructions.
“I was busy with my study, but I bought medicine by myself on time. The doctor told me to keep taking medicine for six months. I thought, well, just take it for six months! He told me to eat more, which could improve my health condition, and I ate more. I hate eggs and milk, but I eat them every day. Finally, I took medication for seven months.”(participant 11)
Poor Self-Regulation Capability
Facing the psychological pressure caused by PTB, poor self-regulation capability also led to medication nonadherence. One student participant stopped taking medication because he was worried about being discriminated against by his classmates.
“I stopped taking the medicine when I went back to school. If my classmates see my medicine, they will know I have TB and look down on me.” (participant 4)
In contrast, another student participant reported that she was more worried about future employment than about being discriminated against. Therefore, she kept taking medication to make sure she was cured.
“It’s okay to take medicine at school. When I take the medicine, I avoid my classmates. If I don’t take care of my body, if I am not cured, I won’t be able to get a job. ”(participant 11)
Misperception of Health Condition
Some participants stopped taking medication either when PTB-related symptoms disappeared or when they felt well. Participants who felt well believed they had been cured and were well.
“I felt I was well. The doctor ordered me to take the medicine for six months, but I took it for three months.” (participant 4)
“After taking the medicine for a month, I didn’t feel any pain anymore and stopped.” (participant 13)
Some participants did not believe they were ill, which was another barrier to taking the medicine. Participants who were tested but had no symptoms did not believe the test results, especially when they met PTB patients who were very ill.
“After taking the medicine for more than ten days, I still did not believe the diagnosis, so I stopped taking my medicine! My other six classmates had symptoms, but I had no symptoms, no cough, no fever. ”(participant 6)
Medication-Related Factors
Side Effects
Medication side effects were a primary reason for stopping medication. Eight participants experienced side effects such as nausea, vomiting, rashes and itching, which made them severely uncomfortable or affected their daily lives. Due to the side effects as well as other reasons described below, six of them stopped taking medicine.
“After I took the medication in the morning, I kept vomiting; I vomited all day … … I ate a mouthful of food and then vomited again. I haven’t taken it since that day.”(participant 5)
Health Service-Related Factors
Poor Treatment Skills of Doctors in Primary Hospitals
The doctors in county- or district-level designated TB hospitals could not alleviate the side effects of the medication and recommended that the participants go to province-level hospitals or hospitals outside of Tibet. Most participants did not take their medicine until they arrived at the recommended hospitals. The minimum interruption time was 19 days, and the longest was one month.
“I am too itchy to take any medicine. I went to the county hospital on the 20th of last month. The doctor told me to go to the Third People’s Hospital of the Tibet Autonomous Region or Chengdu (a large city near Tibet); he could not help me. So, I never took another pill.”(participant 1)
Lack of DOT
All but one of the participants reported that they had not received any supervision from health workers while taking their medication. The only participant who was supervised was involved in a trial to improve medication compliance.
“No doctor urged me to take the medicine; no one asked me to take the medicine. I usually take it by myself.” (participant 17)
Sociocultural Factors
Effect of Traditional Tibetan Medicine
The effect of traditional Tibetan medicine was associated with nonadherence to biological anti-TB drugs. Four participants took Tibetan medicine after they experienced side effects from biological anti-TB drugs: one participant never took biological anti-TB drugs again, and the other three participants switched between traditional Tibetan medicine and biological anti-TB drugs. They believed that traditional Tibetan medicine had many advantages, such as a lack of side effects, a better taste than biological anti-TB drugs, no strict time limit for taking medicine, and no resistance. One elderly participant underwent bloodletting treatments performed by Tibetan doctors more than 40 times after stopping taking biological anti-TB medicine.
“I was really very itchy. After the Spring Festival, I went to the Tibetan hospital. Tibetan doctors are experts! Tibetan medicine is not resistant at all, not itchy; I took it for another year.”(participant 1)
“After taking the medicine for 4 months, I took Tibetan medicine. The Western medicine tastes terrible; what’s more, I always forget. Tibetan medicine is very convenient. It doesn’t matter if you take it today but forget it tomorrow; you can continue the day after tomorrow.”(participant 9)
Lack of Family Member Support
Two participants interrupted the use of the medication because of a lack of effective support from their family members. Their family members were not able to help them when they needed help because their family members lacked knowledge of PTB treatment or were busy with work.
“When I wanted to go back to school, I discussed with my father that I didn’t want to take the medicine any more, and he agreed.” (participant 4)
“My son bought the medicine for me, but there was a period during which he was too busy to buy the medicine, so I didn’t take the medicine for about ten days.” (participant 17)
However, all the seven compliers reported that family member support played an important role in medication adherence. On an emotional level, family member support encouraged the participants and gave them a reason to continue taking medicine. On a practical level, family member support could exempt them from some family responsibility and allow them to focus on their treatment.
“At the beginning, I was very desperate: ‘Oh, mama, ah, what shall I do? Am I going to die?’ Luckily, my father stayed with me all the time; he told me everything would be okay.”(participant 11)
“Crops in my field, the housework, all of that has been done by my wife and son. I just took medicine and rested.” (participant 8)
Discrimination
Only one participant was discriminated against because of PTB and stopped taking medicine. The others reported that their neighbors and friends were still friendly and even took care of them more than usual.
“Some people in my rural community said that I had done something bad. I hope no more people know I have PTB. So, I didn’t dare to take my medicine anymore. I left the rural community and went to Lhasa. ”(participant 10)
Discussion
In Tibet, few studies have reported factors influencing medication nonadherence to PTB treatment, and this qualitative study explored this phenomenon. This study found that medication nonadherence to PTB treatment was influenced by multiple interplaying factors, and the main influencing factors were a lack of knowledge about PTB treatment, poor self-management capability, and the effect of traditional Tibetan medicine.
A lack of knowledge about PTB treatment was confirmed to be important in medication nonadherence among PTB patients in Tibet, especially when the requirements of taking medication conflicted with lifestyle, such as dealing with competing life events without taking medication and ceasing taking medication when feeling better. Similar results have been reported by previous studies.Citation10,Citation15,Citation20–Citation22 According to the provisions on the treatment management of the National TB Control Program implementation guide in China, health education on TB treatment must be carried out for TB patients.Citation3 However, not all of the participants in this study fully grasped the knowledge after receiving oral health education. Therefore, it is necessary to simultaneously distribute to patients permanently viewable PTB treatment knowledge materials (such as publicity pages and webpages), in which knowledge about the curability of PTB, the duration of taking medication, the dangers of medication nonadherence, the side effects of anti-TB drugs and how to deal with side effects are shown.
Poor self-management capability led to medication nonadherence among PTB patients in Tibet, which is a unique finding of this study. Due to the implementation of DOT in other regions, poor self-management capability has rarely been reported as a risk factor for medication nonadherence to PTB treatment in the literature in recent years. This influencing factor is unique to Tibet, in which regional DOT is lacking. The patient’s personal and lifestyle characteristics have the greatest impact on self-management.Citation23 In this study, it was shown that the participants could not handle the relationship between taking medication and life events. Therefore, in order to avoid conflict between taking medication and life events leading to nonadherence, it is important for patients to be well managed by themselves or others while taking medication. However, even under DOT, patients still interrupted taking their medication for a variety of reasons.Citation20,Citation22,Citation24,Citation25 Therefore, in the absence of DOT, it is entirely understandable that the participants in this study did not take their medication as prescribed because of poor self-management capability. However, there is a global consensus that TB patients’ medication-taking behavior must be managed. Therefore, in addition to strengthening patient knowledge of PTB treatment, on the one hand, the self-management capability of PTB patients must be strengthened; on the other hand, because DOT is difficult to implement in Tibet and has disadvantages,Citation7,Citation26 it is necessary to find feasible alternative strategies to DOT, such as video-observed treatment, wirelessly observed therapy, short message service reminders and medication reminders,Citation27–Citation30 to improve medication adherence among PTB patients in Tibet.
Interestingly, the effect of traditional Tibetan medicine also contributed to medication nonadherence among PTB patients in Tibet. Similar findings have also been reported by studies conducted in Papua New Guinea and southern Ethiopia.Citation20,Citation31 In this study, one of the reasons for the use of traditional Tibetan medicine was that the participants wished to avoid the side effects of biological anti-TB drugs, and another was that they strongly identified with the Tibetan medicine their ancestors have used for thousands of years. Traditional Tibetan medicine is important for the Tibetan people in treating diseases they consider not serious. In Tibet, patients assessed primary care in traditional Tibetan medicine hospitals to be significantly better than that in Western medicine hospitals.Citation32 Therefore, in addition to reinforcing the patients’ perception that they should stick to their biological anti-TB drugs once they start taking them, there is a need for interventions that encourage patients to consistently seek Western medical care through the establishment of links to traditional Tibetan medicine hospitals.
Although lack of family member support was not the main reason for medication nonadherence among PTB patients in Tibet, family member support was identified as an important factor for medication adherence. It is possible that family members could provide encouragement, alleviate patients’ economic and social problems and remind them to take their medicine.Citation22,Citation25,Citation31,Citation33 Therefore, family members of patients should also be provided with knowledge about PTB treatment to improve patient medication adherence.
Other factors, such as misperception of health condition, medication side effects and discrimination, have been widely reported by previous studies.Citation24,Citation31,Citation34–Citation36 Thus, the results of this study are general, and although factors influencing medication nonadherence to PTB treatment in different settings are different, they are similar to a certain extent.
There were some limitations in this study. First, this study lacks the view of health workers. Second, there were few farmers and herdsmen included. Because most of the participants could not speak Chinese, there was a language barrier between them and the interviewer. However, both participants from urban areas and those from rural areas in six cities of Tibet were selected, and the results reflect diversity in the influencing factors.
Conclusion
Medication nonadherence to PTB treatment in Tibet is influenced by multiple interplaying factors, and the main influencing factors were a lack of knowledge of PTB treatment, poor self-management capability, and the effect of traditional Tibetan medicine. TB health workers in Tibet should provide permanently viewable PTB treatment knowledge materials to PTB patients when oral health education is conducted, find feasible alternative strategies to DOT (such as video-observed treatment, wirelessly observed therapy, short message service reminders and medication reminders) and establish links to traditional Tibetan medicine hospitals.
Abbreviations
TB, tuberculosis; PTB, pulmonary tuberculosis; DOT, directly observed treatment; DOTS, directly observed treatment, short course; WHO, World Health Organization; AIDS, autoimmune deficiency syndrome.
Data Sharing Statement
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Ethical Review Committee of the School of Medicine, Xizang Minzu University (2019015). All procedures performed in this study were in accordance with Helsinki declaration. Participants who were interviewed face to face signed written informed consent in the interview room. Participants who were interviewed by video signed written informed consent in a convenient place and sent a picture of the form to the interviewer. For participants aged < 18 years (15–17 years), written informed consent was obtained from their parents, and assent was obtained from them.
Author Contributions
JJZ designed the study, conducted the in-depth interviews, and acted as the corresponding author. YYY contributed an amount equal to JJZ in this study; YYY took part in the study design and recruited the participants. TY and PC took part in the in-depth interviews and translated participants’ Tibetan dialect into Mandarin Chinese. All authors contributed to performing the data analysis and drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to sincerely thank the participants of this study. We are also thankful for the Pulmonary Department of the Third People’s Hospital of the Tibet Autonomous Region.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- World Health Organization. Global Tuberculosis Report, 2019. Geneva: World Health Organization; 2019.
- Li B, Zhang X, Guo J, et al. Prevalence of pulmonary tuberculosis in Tibet Autonomous Region, China, 2014. Int J Tuberc Lung Dis. 2019;23(6):735–740. doi:10.5588/ijtld.18.0614
- Ministry of Health of the People’s Republic of China. National TB Control Program Implementation Guide in China. Beijing: Peking Union Medical College Press; 2008.
- Maartens G, Wilkinson RJ. Tuberculosis. Lancet. 2007;370(9604):2030–2043. doi:10.1016/S0140-6736(07)61262-8
- Hou W, Song F, Zhang N, et al. Implementation and community involvement in DOTS strategy: a systematic review of studies in China. Int J Tuberc Lung Dis. 2012;16(11):1433–1440. doi:10.5588/ijtld.12.0080
- Wang L, Zhang H, Ruan Y, et al. Tuberculosis prevalence in China, 1990–2010; a longitudinal analysis of national survey data. Lancet. 2014;383(9934):2057–2064. doi:10.1016/S0140-6736(13)62639-2
- Wei X, Hicks JP, Pasang P, et al. Protocol for a randomised controlled trial to evaluate the effectiveness of improving tuberculosis patients’ treatment adherence via electronic monitors and an app versus usual care in Tibet. Trials. 2019;20(1):273. doi:10.1186/s13063-019-3364-x
- Wolrd Health Organization. Global Tuberculosis Control: Surveillance, Planning, Financing: WHO Report 2005. Geneva: World Health Organization; 2005.
- Okethwangu D, Birungi D, Biribawa C, et al. Multidrug-resistant tuberculosis outbreak associated with poor treatment adherence and delayed treatment: Arua District, Uganda, 2013–2017. BMC Infect Dis. 2019;19(1):387. doi:10.1186/s12879-019-4014-3
- Woimo TT, Yimer WK, Bati T, Gesesew HA. The prevalence and factors associated for anti-tuberculosis treatment non-adherence among pulmonary tuberculosis patients in public health care facilities in South Ethiopia: a cross-sectional study. BMC Public Health. 2017;17(1):269. doi:10.1186/s12889-017-4188-9
- Yao S, Huang WH, van den Hof S, et al. Treatment adherence among sputum smear-positive pulmonary tuberculosis patients in mountainous areas in China. BMC Health Serv Res. 2011;11(1):341. doi:10.1186/1472-6963-11-341
- Chen S, Zhang H, Pan Y, et al. Are free anti-tuberculosis drugs enough? An empirical study from three cities in China. Infect Dis Poverty. 2015;4(1):47. doi:10.1186/s40249-015-0080-y
- Lei X, Huang K, Liu Q, Jie YF, Tang SL. Are tuberculosis patients adherent to prescribed treatments in China? Results of a prospective cohort study. Infect Dis Poverty. 2016;5(1):38. doi:10.1186/s40249-016-0134-9
- Xu W, Lu W, Zhou Y, Zhu L, Shen H, Wang J. Adherence to anti-tuberculosis treatment among pulmonary tuberculosis patients: a qualitative and quantitative study. BMC Health Serv Res. 2009;9(1):169. doi:10.1186/1472-6963-9-169
- Tang Y, Zhao M, Wang Y, et al. Non-adherence to anti-tuberculosis treatment among internal migrants with pulmonary tuberculosis in Shenzhen, China: a cross-sectional study. BMC Public Health. 2015;15(1):474. doi:10.1186/s12889-015-1789-z
- Xu M, Markstrom U, Lyu J, Xu L. Detection of low adherence in rural tuberculosis patients in China: application of morisky medication adherence scale. Int J Environ Res Public Health. 2017;14(3):E248. doi:10.3390/ijerph14030248
- Azizi N, Karimy M, Salahshour VN. Determinants of adherence to tuberculosis treatment in Iranian patients: application of health belief model. J Infect Dev Ctries. 2018;12(9):706–711. doi:10.3855/jidc.9653
- Zegeye A, Dessie G, Wagnew F, et al. Prevalence and determinants of anti-tuberculosis treatment non-adherence in Ethiopia: a systematic review and meta-analysis. PLoS One. 2019;14(1):e0210422. doi:10.1371/journal.pone.0210422
- Nellums LB, Rustage K, Hargreaves S, Friedland JS. Multidrug-resistant tuberculosis treatment adherence in migrants: a systematic review and meta-analysis. BMC Med. 2018;16(1):27. doi:10.1186/s12916-017-1001-7
- Diefenbach-Elstob T, Plummer D, Dowi R, et al. The social determinants of tuberculosis treatment adherence in a remote region of Papua New Guinea. BMC Public Health. 2017;17(1):70. doi:10.1186/s12889-016-3935-7
- Gebreweld FH, Kifle MM, Gebremicheal FE, et al. Factors influencing adherence to tuberculosis treatment in Asmara, Eritrea: a qualitative study. J Health Popul Nutr. 2018;37(1):1. doi:10.1186/s41043-017-0132-y
- Sahile Z, Yared A, Kaba M. Patients’ experiences and perceptions on associates of TB treatment adherence: a qualitative study on DOTS service in public health centers in Addis Ababa, Ethiopia. BMC Public Health. 2018;18(1):462. doi:10.1186/s12889-018-5404-y
- Schulman-Green D, Jaser SS, Park C, Whittemore R. A metasynthesis of factors affecting self-management of chronic illness. J Adv Nurs. 2016;72(7):1469–1489. doi:10.1111/jan.12902
- Skinner D, Claassens M. It’s complicated: why do tuberculosis patients not initiate or stay adherent to treatment? A qualitative study from South Africa. BMC Infect Dis. 2016;16(1):712. doi:10.1186/s12879-016-2054-5
- Tadesse T, Demissie M, Berhane Y, Kebede Y, Abebe M. Long distance travelling and financial burdens discourage tuberculosis DOTs treatment initiation and compliance in Ethiopia: a qualitative study. BMC Public Health. 2013;13(1):424. doi:10.1186/1471-2458-13-424
- World Health Organization. Global Tuberculosis Report 2014. Geneva: World Health Organization; 2014.
- Story A, Aldridge RW, Smith CM, et al. Smartphone-enabled video-observed versus directly observed treatment for tuberculosis: a multicentre, analyst-blinded, randomised, controlled superiority trial. Lancet. 2019;393(10177):1216–1224. doi:10.1016/S0140-6736(18)32993-3
- Browne SH, Umlauf A, Tucker AJ, et al. Wirelessly observed therapy compared to directly observed therapy to confirm and support tuberculosis treatment adherence: a randomized controlled trial. PLoS Med. 2019;16(10):e1002891. doi:10.1371/journal.pmed.1002891
- Bediang G, Stoll B, Elia N, Abena JL, Geissbuhler A. SMS reminders to improve adherence and cure of tuberculosis patients in Cameroon (TB-SMS Cameroon): a randomised controlled trial. BMC Public Health. 2018;18(1):583. doi:10.1186/s12889-018-5502-x
- Liu X, Lewis JJ, Zhang H, et al. Effectiveness of electronic reminders to improve medication adherence in tuberculosis patients: a cluster-randomised trial. PLoS Med. 2015;12(9):e1001876. doi:10.1371/journal.pmed.1001876
- Gugssa Boru C, Shimels T, Bilal AI. Factors contributing to non-adherence with treatment among TB patients in Sodo Woreda, Gurage Zone, Southern Ethiopia: a qualitative study. J Infect Public Health. 2017;10(5):527–533. doi:10.1016/j.jiph.2016.11.018
- Wang W, Shi L, Yin A, et al. Primary care quality between traditional Tibetan medicine and western medicine hospitals: a pilot assessment in Tibet. Int J Equity Health. 2015;14(1):45. doi:10.1186/s12939-015-0174-y
- Da Silva RD, De Luna FDT, De Araujo AJ, et al. Patients’ perception regarding the influence of individual and social vulnerabilities on the adherence to tuberculosis treatment: a qualitative study. BMC Public Health. 2017;17(1):725. doi:10.1186/s12889-017-4752-3
- Fang XH, Dan YL, Liu J, et al. Factors influencing completion of treatment among pulmonary tuberculosis patients. Patient Prefer Adherence. 2019;13:491–496. doi:10.2147/PPA.S198007
- Tesfahuneygn G, Medhin G, Legesse M. Adherence to anti-tuberculosis treatment and treatment outcomes among tuberculosis patients in Alamata District, northeast Ethiopia. BMC Res Notes. 2015;8(1):503. doi:10.1186/s13104-015-1452-x
- Gideon K. Factors Influencing Clients Adherence to Tuberculosis Treatment in Birim South. School of Public Health, University of Ghan; 2019.