Abstract
Although tuberculosis (TB) incidence has significantly declined in high-income, low-incidence (HILI) countries, challenges remain in managing TB in vulnerable populations who may struggle to stay on anti-TB treatment (ATT). Factors associated with non-adherence to ATT are well documented; however, adherence is often narrowly conceived as a fixed binary variable that places emphasis on individual agency and the act of taking medicines, rather than on the demands of being on treatment more broadly. Further, the mechanisms through which documented factors act upon the experience of being on treatment are poorly understood. Adopting a relational approach that emphasizes the embeddedness of individuals within dynamic social, structural, and health systems contexts, this scoping review aims to synthesize qualitative evidence on experiences of being on ATT and mechanisms through which socio-ecological factors influence adherence in HILI countries. Six electronic databases were searched for peer-reviewed literature published in English between January 1990 and May 2020. Additional studies were obtained by searching references of included studies. Narrative synthesis was used to analyze qualitative data extracted from included studies. Of 28 included studies, the majority (86%) reported on health systems factors, followed by personal characteristics (82%), structural influences (61%), social factors (57%), and treatment-related factors (50%). Included studies highlighted three points that underpin a relational approach to ATT behavior: 1) individual motivation and capacity to take ATT is dynamic and intertwined with, rather than separate from, social, health systems, and structural factors; 2) individuals’ pre-existing experiences of health-seeking influence their views on treatment and their ability to commit to long-term regular medicine-taking; and 3) social, cultural, and political contexts play an important role in mediating how specific factors work to support or hinder ATT adherence behavior in different settings. Based on our analysis, we suggest that person-centered clinical management of tuberculosis should 1) acknowledge the ways in which ATT both disrupts and is managed within the everyday lives of individuals with TB; 2) appreciate that individuals' circumstances and the support and resources they can access may change over the course of treatment; and 3) display sensitivity towards context-specific social and cultural norms affecting individual and collective experiences of being on ATT.
Introduction
The re-emergence of tuberculosis (TB) as a significant public health issue during the 1990s was linked not only to the unfolding HIV epidemic and growth of drug resistance, but to poorly run TB control programsCitation1 and “… a mood of complacency [leading] to declining investment in research and public health infrastructure” (pp 182).Citation2 From 2000 to 2018, TB disease incidence in high-income countries (HIC) fell from 18 to 11 per 100,000 population.Citation3 Elimination of TB, defined as an annual incidence <1 per million population,Citation4 became a realistic prospect in many HIC with low TB incidence.Citation5,Citation6 However, challenges to elimination remain in these settings, where TB disproportionately affects socio-economically disadvantaged and marginalized population groups with poor health literacy and access to healthcare. These include migrants, individuals with drug dependence, and those with no fixed abode.Citation7,Citation8 Many of these individuals may access the health system late and consequently experience delays in commencing anti-tuberculosis treatment (ATT). They are also less likely to complete treatment as a result of social risk factors and more likely to have drug-resistant TB (DR-TB), in turn widening the gap in health and social inequalities.Citation9–Citation11
Treatment adherence has important effects on individual outcomes, transmission, and risk of developing DR-TB,Citation12 hence the importance of early identification of those likely to struggle with accessing and remaining-on treatment. Socio-demographic factors associated with non-adherence to ATT in high-income, low-incidence (HILI) countries are well-documented;Citation13 however, adherence is often narrowly conceived as an individual act of taking medicines, which fails to take account of the broader experience of being and staying on ATT. Furthermore, mechanisms through which socio-demographic variables influence ATT-related behavior in different settings and populations are poorly understood. This is particularly the case for social and structural determinants that indirectly affect individual medicine-taking behaviors via complex causal pathways.Citation14 It is widely acknowledged that the factors influencing individuals’ ability to access and stay on treatment are multi-dimensional, often external to the health system, and beyond individuals’ control.Citation15 Yet the concept of adherence, as understood in clinical terms, is curiously detached from patients’ overall experience of being on treatment, resulting in an emphasis on the logistics of treatment-taking without addressing the broader contextual factors affecting individuals’ motivation and ability to stay on treatment.Citation16 Accordingly, current interventions to support medication adherence focus mainly on what can be delivered through routine health services, including home- or facility-based directly observed therapy (DOT) with text reminders, counselling, and medication monitoring devices.Citation17
As health systems in HIC are generally better resourced than those in high TB burden countries, greater opportunities exist to tailor services to meet the needs of individuals on treatment. Given the growing call for patient-centered and differentiated care, acknowledging the complex nature of non-adherence behavior can “help gain an optimal understanding of patient challenges and experiences, and […] avoid centering on patient performance” (pp 208).Citation18 It is vital that we move beyond essentializing traits of “non-adherent” individuals to acknowledging the demands and challenges of being on ATT and identifying effective support strategies for those struggling to follow ATT regimens. Understanding the contextual factors and mechanisms through which known determinants impact on adherence over the course of treatment will help us better fulfil World Health Organization (WHO) guidelines to provide responsive person-centered TB care.Citation19
The aim of this scoping review was to critically synthesize qualitative evidence on the mechanisms through which socio-ecological factors influence the experience of being on ATT in HILI countries. In our understanding of socio-ecological factors, we build on and expand the model proposed by Munro et al.Citation15 We sought to answer the following research questions:
What socio-ecological factors affect individuals’ experience of ATT in HILI countries and how do these inter-relate?
Through which mechanisms do these factors impact on individual adherence to ATT?
What role does context have in mediating determinants and mechanisms of ATT adherence behavior?
Methods
Theoretical Framework
Our review draws on the multi-factorial determinants of adherence to long-term medication, an approach originally proposed by WHOCitation20 and since elaborated on by researchers in socio-behavioral and ecological frameworks.Citation21 Common to these frameworks is the recognition that adherence is a complex phenomenon and not simply restricted to the act of taking or not taking medications on time, based on the advice of a medical provider.Citation16,Citation22 Authors adopting a socio-behavioral perspective highlight the web of proximate and distal influences on adherence behavior. These include characteristics of the disease, the medications, patients themselves as well as factors related to the health-care system, all of which interact in numerous intricate ways.Citation21 Drawing on these perspectives, we propose a relational approach to the experience of being on ATT. By relational, we mean that factors influencing treatment behavior are not only connected and inter-linked, but also dynamic, ie, that their influence on treatment behaviour does not remain fixed over time. Our socio-ecological classification of factors builds on the simple model proposed by Munro et alCitation15 to include treatment-related, personal, social, health systems, and structural levels. We recognize that the relative weight of factors within these levels and their influence on treatment behaviors fluctuate in importance over the course of a longer health-seeking trajectory shaped by patients’ evolving social and structural circumstances.Citation23 This approach coincides with recent discussionsCitation12 seeking to align the concept of ATT adherence with a more nuanced relational framing of medicine-taking behavior that recognizes different temporal stages at which treatment might be delayed, missed, or discontinued.Citation24
Methodological Approach
In line with our exploratory research questions, we conducted a scoping review following the approach outlined by Arksey and O’Malley.Citation25 Based on this approach, a scoping review involves five stages: (1) identifying research questions, (2) identifying relevant studies, (3) study selection, (4) data charting or extraction and (5) collating, summarizing and reporting results.Citation25 We developed search strategies, eligibility criteria for study selection, data extraction forms, and an analysis plan before commencing the review. Search strategies and extraction matrices were piloted and further refined to capture all the relevant information for the study.
Information Sources and Searches
Six electronic databases: CINAHL, MEDLINE, PsycINFO, ASSIA, Web of Science, and Scopus were searched by two researchers (SA, NV) independently in May 2020. The initial search included keywords related to TB, treatment, and adherence. As this yielded primarily quantitative evidence, additional search terms specific to qualitative and mixed methods were included. The final search strategy used the following keywords: “tuberculosis AND (adherence OR compliance OR concordance) AND treatment AND (qualitative OR ethnograph* OR anthropolog* OR sociol* OR phenomenol* OR narrative)”.
Inclusion and Exclusion Criteria
To capture a comprehensive range of qualitative studies relating to the experience of being and staying on ATT, we set intentionally broad selection criteria. Studies from any discipline or theoretical tradition that used qualitative and/or mixed methods to describe the experience of taking ATT or factors influencing treatment non-adherence from the perspective of adult patients, care givers, or health-care providers (HCPs) were included. We included studies published in peer-reviewed journals since January 1990 to reflect the rising incidence of TB in HIC that began in the early 1990s (and its recognition as a major public health problem by WHO in 1991).Citation1 Studies that focused on children, latent TB, adherence to ATT in low- and middle-income countries (based on the World Bank Classification 2020),Citation6 and those published before 1990 in languages other than English were excluded. To ensure inclusion of studies that documented the experience of being on ATT, even if they did not explicitly assess non-adherence behaviors, no explicit definition of adherence or non-adherence was used to screen studies for inclusion.
Study Selection
Following the removal of duplicates, three researchers (SA, NV, KK) screened titles and abstracts retrieved through database searches for relevance based on the selection criteria. However, to ensure consistency in the screening process, a random sample of 10% titles and abstracts were independently double screened by KK. The few discrepancies identified were resolved through discussion. We located and reviewed the full texts of studies that were retained following the title and abstract screening process. For studies meeting inclusion criteria, we examined reference lists for additional inclusions.
Data Extraction and Synthesis
Data were extracted using a standardized and piloted form and included the following categories: study identifiers (study author, year of publication); settings; populations; aims; methods; theoretical approaches; and factors shaping the experience of ATT, including specific reference to adherence behavior. A narrative approach was used to categorize and synthesize the data according to five socio-ecological domains relevant to the experience of taking ATT: treatment-related, personal, social, health system, and structural. We classified reported influences on individuals’ experience of ATT under these socio-ecological domains and examined, where reported and relevant, the mechanisms through which these factors influenced treatment behavior.
Results
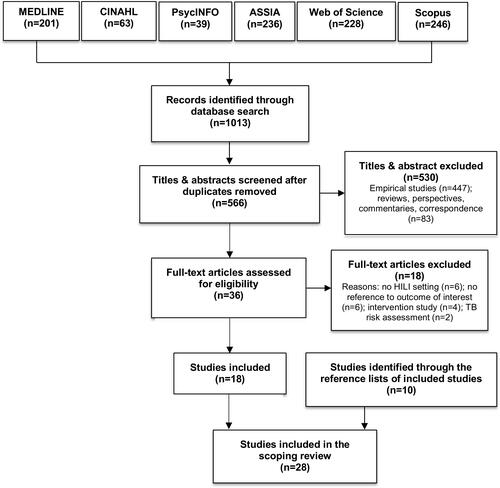
Initial database searches retrieved 1013 records. After duplicates were removed, 566 titles and abstracts were screened against eligibility criteria. Thirty-six full-text studies emerged as potentially relevant; of these, 18 did not meet eligibility criteria, and 18 studies were included in the review. An additional 10 studies were identified from searching reference lists of included studies, resulting in a total 28 included studies ().
Figure 1 Flow diagram detailing study selection process.
Characteristics of Included Studies
Over two-thirds of studies (n=19) were published after 2010 (). Studies were conducted in Europe (n=12), North America (n=11), East Asia (n=2), and Australasia (n=3). Six studiesCitation23,Citation26–Citation30 used a mixed-methods approach, the rest exclusively used qualitative methods. Studies reported on the perspectives of individuals with TB (n=15), community members (n=3), health providers (n=2), or a combination of different population groups (n=8).
Table 1 Summary Characteristics of Included Studies (n = 28)
Examining “Adherence” Within “Treatment Behavior”
Despite “adherence” being one of our search terms, only three studiesCitation28,Citation30,Citation31 offered explicit definitions of adherence. Non-adherence to ATT was defined in one study as taking less than 80% of the prescribed regimenCitation31 and loss-to follow-up was described in another as treatment interruption for 60 consecutive days or more, or for two consecutive months, or insufficient treatment duration.Citation28 One paper used the Morisky Medication Adherence Scale (not specific to TB) to assess levels of adherence.Citation32
The absence of an explicit focus on “adherence” to ATT reflects the broader approach adopted by qualitative researchers who situate the act of taking medication within the broader subjective experience of being on ATT. “Treatment behavior” is a more apt term that comprises individuals and their immediate social networks’ responses to a diagnosis, their treatment-seeking patterns and their expectations and experience of treatment regimens available to them, which may differ from those prescribed by a formal health provider. For studies that did not explicitly define adherence, the framing of non-adherence within the overall experience of being on ATT was closely related to the theoretical framing of the paper in question. Four approaches were identified: a pragmatic health services approach (n=11), critical perspectives (n=7), applied medical anthropology (n=7), and social theory (n=3) (). Disciplinary background and aim of the studies frequently dictated the level (unit) of analysis in the studies. Half the studies that adopted a pragmatic or applied approach focused on personal and treatment-related factors, whereas a third of the studies adopting theoretical and sometimes critical perspectives were more likely to situate ATT-related behavior within a broader social or structural context.
Table 2 Theoretical Framing of Papers Included
Synthesis of Results
Treatment-Related Factors
Half of the studies (n=14; 50%) reported on treatment-related factors influencing experiences of ATT. These included individuals’ responses to the number of tablets, complexity of regimens, duration of treatment and its side-effects, and potential interactions between TB and other medication. Unsurprisingly, these papers provided the most direct links between experiences of taking ATT and adherence. Several studies discussed difficulties faced by patients in adhering to lengthy treatment regimens that often required strictly routinized lifestyles.Citation26,Citation27,Citation30,Citation33–Citation36
The whole thing hit me when they sat down and spoke to me about the medication, nine months of medication, you can’t do this, and you can’t have a drink … I suddenly realized … and I felt quite depressed [former TB Patient in New Zealand, Searle et al., 2007., pp.73].Citation34
Both the pill burden and the drug regimen affected patients’ willingness to continue with the treatment:Citation26,Citation30,Citation36–Citation39
When I looked at ten tablets, I thought, on an empty stomach, I cannot [Former TB patient in Canada, Marra et al., 2004, pp.6].Citation39
I hated it (…) I felt that, I was threatened, you know, it’s like, if you didn’t take this, then you couldn’t have that, I felt like I was at school. [Former TB patient in the UK, Craig & Zumla, 2015, pp.108].Citation26
Multiple side-effects and adverse reactions were reported, including debilitating gout, general malaise, and hair loss.Citation30,Citation34,Citation35,Citation37–Citation42 This resulted in patients often questioning the physical safety of the treatmentCitation30 and their perceived health costs.Citation41 This was further compounded by the sacrifices patients felt they had to make, including prolonged abstinence from alcohol:
One glass of beer or anything I’d just feel violently ill … it would be like a minor food poisoning attack [former TB Patient, Searle et al., 2007, pp.74].Citation34
Personal Factors
Three quarters of studies (n=21; 75%) reported that the personal characteristics of individuals shaped their experiences of ATT and adherence behavior, as well as vice-versa, ie, how being on ATT affected daily lives. Here, we refer to individuals’ socio-demographic characteristics, but also their sense of agency and control, health and treatment-related knowledge, and experience of having TB and being on ATT.
Sense of Agency, Autonomy, and Control
Struggles to preserve autonomy, regain control of life, and a compromised sense of self-efficacy were linked to behavior in a few studies.Citation28,Citation39,Citation43,Citation44 Some patients blamed forgetfulness for missing treatment doses.Citation39,Citation43 Others may have more strategically “forgotten” about treatment to help them regain control or return to a “normal life”.Citation43 For example, HCPs, describing colleagues who had TB, linked non-adherence to the nature of their work:
Because they [physicians and nurses] have nightshifts … it seems difficult for them to set a particular time of the day to take medicines [HCP in Japan, Kawatsu et al., 2018, pp.8].Citation28
For patients, subscribing to a supervised treatment regimen was sometimes experienced as disempowering, as described in a study undertaken among Somali and Ethiopian migrants with TB in Norway:
I asked about [self-administering] and the nurse said, ‘No, you are not allowed to.’ So, I was annoyed. ‘I am not a child,’ I said to her. ‘I am an adult. I take the medication for my own sake and not for you [Somali man in Norway, Sagbakken et al., 2012, pp.317].Citation44
Health practitioners with TB were also more likely to reject adherence support when offered:
Oh, it’s so difficult to get them (physicians) on DOTS … they’re professionals. Why should they be checked up by us, the public health nurses? I think that’s what they think [HCP in Japan, Kawatsu et al., 2018, pp.9].Citation28
Lay Knowledge, Beliefs, and Perceptions of TB and TB Treatment
Misconceptions, incorrect or lay knowledge, and ethno-medical beliefs regarding TB etiology, transmission, and treatment outcomes were reported to negatively impact ATT-related behavior via diagnostic delays, loss-to-follow-up after sputum tests, and patients not returning for outpatient follow-up visits.Citation27,Citation31,Citation34,Citation37,Citation38,Citation40,Citation45,Citation46 Reported lay etiologies of TB included religious ideas, poisoning, cigarette and alcohol use, unsanitary conditions, poor nutrition, wearing wet clothes, colds, coughs, contact with a person with TB, and overworking,Citation38,Citation46 which in some cases led to misinterpretation of initial symptoms:
I thought it was because of the heavy load I carried. I did not report the chest pain for about three weeks. When I coughed and saw blood, then I came to the doctor [Ghanaian man in the UK, Nnoaham et al., 2006, pp.1015].Citation38
Although perceived to be curable by both modern and traditional medicine (eg, change in environment, good household sanitation, smoking cessation, exercise, or eating a balanced diet), TB was seen as potentially lethal and highly contagious,Citation46 leading to spurious practices of self-isolation and use of separate utensils and linen among some patients to protect their families.Citation45 Patients who lacked knowledge had more negative attitudes to TB and worse experiences with ATT than better informed patients.Citation40 For some individuals, however, the threat of sanctions was a “perverse incentive” that dissuaded non-adherence:
I never forget to take my pills because I don’t want to go to jail [Former TB patient in Canada, Marra et al., 2004, pp.6].Citation39
Lack of understanding about the nature of TB disease often resulted in non-acceptance, or low levels of perceived risk, and, therefore, delays in seeking help.Citation31,Citation38,Citation45 Low-risk perception, however, could also arise from good understanding and familiarity with TB, as was the case in HCPs with TB:Citation28
I think the physicians are too used to seeing diseases … like, it’s not a special event for them [HCP, cited in Kawatsu et al., 2018, pp.8].Citation28
Acceptance of the disease and its consequences, which was often achieved via support from nurses, was reported to facilitate adherence to ATT.Citation34
Lived Physiological Experience of TB and Comorbidities
Disease chronicity and a possibility of recurrence, comorbidities (HIV, diabetes), and associated general physical weakness influenced the illness experience of being on ATT, which, in turn, was reported in some studies to negatively influence adherence behaviour.Citation27,Citation29,Citation30,Citation34,Citation38 Compromised health and comorbidities worsened the experience of being a TB patient, especially when care was uneven or fragmented.Citation23 Co-infection with HIV was seen to compound patients’ health issues (eg, weight loss, cough) and increase social stigmatization, referred to in one paper as “cross-stigmatisation”:Citation38
It is always like … ’He’s got TB; he must be HIV positive’. That’s the way people look at it. I think people see that the symptoms look alike, so they just conclude that anyone with TB has HIV [Zambian man in the UK, Nnoaham et al., 2006, pp.1016].Citation38
In a US-based study, Curtis et al describe how health systems “failings” in the care of people living with HIV who injected intravenous drugs led to confusion about the risk of TB infection and need for adherence to TB preventive therapy when testing positive for latent TB.Citation27
Substance Use
Drug and alcohol use influenced ATT-related behavior and adherence.Citation26,Citation27,Citation34,Citation39 For people with TB who used drugs, drug use (eg, crack cocaine, heroin) was often prioritized over treatment; one study noted multiple episodes of self-discharge from hospital to source drugs or secure access to methadone.Citation27
Psychosocial Factors
Anxiety and worries about the consequences of having TB as well as being on treatment, self-stigmatization, and resulting social isolation and loneliness were commonly reported among individuals on treatment, which in turn compromised optimal health seeking behaviour.Citation30,Citation33,Citation34,Citation38,Citation40,Citation44–Citation47 These experiences were especially acute in marginalized groups. For example, Mexican male migrants in the US talked about the negative impact of TB stigma on constructs of masculinity and power, which led to social isolation, internalized stigma, and delayed care seeking.Citation45 Self-stigmatization resulted in patients restricting their social circles to limit exposure to discrimination or social marginalization.Citation38,Citation46
Social Factors
Seventeen of 28 (61%) papers reported on social factors influencing individuals’ experience of TB care, and specifically their ability to access and stay on treatment. Under social factors, we included any reference to social and cultural norms, values, relationships, and networks that were reported to impact positively or negatively on the experience of ATT including adherence behavior.
Social and Community Life
Social roles and daily lives including interactions with family, friends, peers, and other social networks affected (and in turn were affected by) the experience of having TB and being on ATT.Citation29,Citation35,Citation36,Citation39,Citation40,Citation43 Marra et al (2004) discuss the disruptive effects of ATT on daily routines, especially around alcohol and drug use, and panhandling (begging in the street) among marginalized populations in Canada.Citation39 Konradsen et al (2014) note that social pressures and responsibilities affected care-seeking behavior for TB patients in Denmark.Citation43
Social Support/Lack of Support
Social support - or the lack of it – was an important determinant of knowledge about TB, the experience of having TB, and the ability to access and stay on treatment. Lack of social support was particularly acute in marginalized groups, including migrants;Citation26,Citation29,Citation33 aboriginal or indigenous groups;Citation35,Citation36,Citation39 and people who used drugs.Citation26 For many of these individuals, living in urban areas without family support exacerbated social isolation. However, support could fluctuate over the course of treatment. Two studies illustrated the ambivalent influence of peers in dissuading care-seeking: in Canada, Marra et al (2004) describe a patient reporting that his family, despite being supportive of his condition “… told me not to take my pills anymore because they make me sick”.Citation39 Conversely, in two UK studies, Nnoaham et al (2006) and Craig and Zumla (2015) note the positive influence of advice and support from well-informed social contacts on patients’ conditions.Citation26,Citation38
Stigma
Several studies highlighted the negative impact of TB-related social stigma on individual treatment-seeking behaviour.Citation26,Citation33,Citation43,Citation46 For some migrants, stigma related to TB was marked and could result in exclusion of the individual from family and social networks.
Your family members don’t come around because they feel you are dirty, and they are afraid that they will be infected by you. They don’t want to talk to you. [Filipino patient in the USA, Yamada et al., 1999]., pp. 479].Citation46
Craig et al (2015) document how Somali migrants in the UK underwent the threat of eviction and rejection by the wider Somali community, which resulted in a loss of material and social support.Citation26 Studies on migrants’ experiences of TB in North AmericaCitation39,Citation42,Citation45,Citation46 and on aboriginal Canadians’ experiences of TB sanatoriaCitation35 also found that social stigma could persist long after the course of treatment was over. However, the experience of stigma, like social support, may differ depending on location and stage of treatment.Citation41,Citation42
Health Systems-Related Factors
Most papers (n=24; 86%) reported on health systems factors that impacted on patients’ lived experiences of TB care, including their ability to access and stay on treatment. Here, we refer to patients’ access to and utilization of health services, the organization of care and treatment regimens, perceived quality of care, and relationships with HCPs, including communication and support.
Access to TB Related Knowledge and Care
A few studies suggested that knowledge and health-seeking related to TB may be poorer among migrant groups and linked these to limited availability and accessibility of information, particularly in languages other than English.Citation40,Citation48
They knew that TB was infectious, they had to be careful. But I still felt that our Chinese community lacked information on TB. They thought about infection and didn’t know much about TB disease [HCP in Canada, Gibson et al., 2004, pp. 938].Citation40
A number of studies documented delays in diagnosis or early misdiagnosis by frontline health services, with subsequent delays in treatment and frustration and anger for patients.Citation27,Citation47,Citation49 This was sometimes exacerbated by being economically disadvantaged, socially excluded, or having a “chaotic” lifestyle, which meant that individuals often could not afford to attend for care,Citation47 were not registered with a primary care doctor,Citation49 or were reluctant to seek care.Citation27
Organization of Care
Poor understanding of the necessity of TB treatment was not always linked to knowledge but in some cases did contribute to collective negative experiences of healthcare in marginalized groups. Three studies of TB care in Canadian aboriginal and indigenous individuals clearly illustrate how traumatic memories of people with TB who were isolated from their communities and re-housed in TB sanatoria influenced contemporary perceptions of TB treatment.Citation35,Citation36,Citation50 The fear of institutional sanctions for TB patients was also present in a study in the United States (US) examining factors influencing access to care and adherence for a drug-using population:
He had heard negative stories, such as threats of detention and withholding methadone, from IDUs [intravenous drug users] in his gallery (including J.), who had been at other hospitals [Curtis et al., 1994, pp.323].Citation27
Marra et al (2004) describe isolation and boredom experienced by patients who were admitted to hospital, where “the only thing to do (…) was to eat and sleep”Citation39 and HCP use of masks and gloves made one patient feel like “a leper”. In many settings, the inflexibility of the health system and care delivery (DOT in particular) served to alienate patients: in New Zealand, van der Oest et al (2005) describe the disconnect between cultural expectations of different communities (eg, Somali immigrants, Asian immigrants, Cook Islanders, and Māori) and the responsiveness of the health system.Citation47
Interactions and Communication with HCP
The quality of relationships and communication with health-care staff impacted experiences of ATT, especially amongst marginalized groups. Uncaring and contemptuous attitudes, unfavorable treatment towards homeless people,Citation27,Citation47 immigrant and aboriginal individuals,Citation40–Citation42 or stigmatization (for example, of African patients with TB being HIV positive),Citation38 were noted in some studies. In Norway, Sagbakken et al describe the power imbalance inherent in the patient–provider relationship, noting the rigidity of treatment regimens, which gave greater power to HCPs who could threaten patients by referring to policy enforcement.Citation44
HCPs’ and patients’ conflicting beliefs and priorities were reported to have long-term effects on individuals’ views of the health system. Indigenous participants in a Canadian study expressed concerns that “present-day healthcare would be similar to the treatments they received within the sanatoriums” (pp. 1596), with HCPs often described as “people who didn’t have any knowledge of our culture” (pp. 1594).Citation35 A study from a culturally diverse clinical setting in New Zealand cites communication difficulties as a “primary contributing factor to non-adherence” (pp. 66).Citation47
Conversely, the provision of comprehensive support tailored to patient’s characteristics,Citation30 personalized care,Citation38 and comprehensive counsellingCitation51 were linked to improved adherence.
You get someone sitting next to you and trying to get your mind off things, just to talk to you, ask you about other things apart from the disease (…) it helps you to take the medication, and to look at life with a different perspective as you’re taking the medication … [TB patient in the UK, Boudioni et al., 2011, pp.272].Citation51
Two studies described how HCPs not only provided clinical guidance, adherence oversight, and “expert companionship”, but also helped TB patients with food, transport and coordinated referrals to other health and welfare services.Citation33,Citation34
Structural Factors
Eighteen (64%) papers reported on structural factors affecting individuals’ access to and experience of ATT. We defined structural factors as those social and political mechanisms that generate and reinforce social class divisions, placing individuals within hierarchies of power, prestige, and access to resources.Citation52 Here, we were concerned with both the direct and indirect influences of structural factors on individuals’ access to TB care and treatment adherence behavior.
Policies and Funding
Three papers reported on the broader policy and financial environment as negatively affecting availability of support services for people taking ATT, particularly for socio-economically deprived individuals.Citation26,Citation27,Citation31 A UK paper described how financial restrictions placed by funders on organizations supporting homeless people impacted on their ability to support patients.Citation26 In a US-based study, anti-drugs policies were described as leading to patients’ fear of detention, with an increase in the likelihood of incarceration used to ensure treatment adherence.Citation27 Withdrawal of funding for TB services and limited power of local Health Boards to manage TB services negatively influenced local capacity to address TB in aboriginal population in one Australian study.Citation31
Legal Status of Migrants and Refugees
Six papers, focused on the experiences of migrants, cited concerns around legal status in the host country as having negative effects on individuals’ health and treatment-seeking behaviour.Citation29,Citation37,Citation44–Citation46,Citation48 Immigrants faced language barriers and barriers to employment that in turn affected health literacy and health-seeking behaviour.Citation29 Fear of deportation or expulsion from the country resulted in mistrust of the health system, which negatively affected treatment-seeking behaviour,Citation45,Citation46,Citation48 and also discouraged individuals’ ability to voice an opinion on their treatment experience, as illustrated in one poignant study of Ethiopian and Somali migrants in Norway:
People feel that this is not their country and then it is hard to protest. This [DOT] only applies for people coming from the third world [Male patient in Norway, Sagbakken et al., 2012, p.316].Citation44
Socio-Economic Marginality
Homelessness, loss of employment, and associated financial difficulties affected TB patients’ ability to access treatment and adhere to ATT.Citation23,Citation27,Citation33,Citation39 TB patients who lost their work due to TB experienced subsequent financial difficulties, but lacked confidence to look for employment opportunities because of fears of being stigmatized or marginalized by potential employers or colleagues.Citation33
Among people who used drugs in one US-based study, the absence of social housing after discharge led to homelessness and greater likelihood of continued drug use, negatively affecting care-seeking and ability to stay on treatment.Citation27 For patients in Latvia, socio-economic marginality translated into limited power and social capital to negotiate the health system, including the parameters of TB care.Citation23 In the UK, homelessness or inadequate temporary accommodation were cited as factors hindering capacity to stay on treatment.Citation26,Citation33 Patients with unstable livelihoods prioritized food over pill-taking and found it challenging to store medicine or maintain any kind of routine.
I suspect the reasons why people don’t complete treatment are to do with chaotic things in their lives. There may be all kinds of social difficulties that make it difficult for them to seek treatment [HCP in the UK, Gerrish et al., 2013, pp.2289].Citation33
Conversely, for some HCPs, working with individuals who had little power to negotiate the terms of care sometimes facilitated patients’ adherence: in Norway, HCPs conceded that implementing DOT was easier in the case of patients who were without status or permanent work.Citation44
Experience of Violence
A few papers described the impact of past experiences of segregation, violence, torture, or physical or sexual abuse on current health-seeking behavior, including treatment-related behaviors. Three Canadian papers referred to the legacy of colonization and social inequities that underpinned the problem of TB in indigenous communities, but also accounted for pervasive misconceptions and mistrust.Citation35,Citation39,Citation50 In one study, traumatic memories of TB patients being segregated in sanatoria and alienated from their communities in the past were still vivid for individuals of aboriginal origin, with negative impact on their perceptions of the TB services.Citation35 Conversely, for Cambodian refugees in New Zealand, fear and negative recollections of people who had died from TB in refugee camps and in Cambodia engendered compliance to ATT.Citation47
A UK study describes how lives “dominated by a cycle of crime” resulted in feelings of social exclusion, which in turn constrained individuals’ healthcare seeking.Citation26 However, the threat of violence as a “risk factor” for poor adherence is not necessarily visible, as demonstrated in Latvia.
For some women, we know that they probably have some money and [health] insurance and so on … but we don’t know what happens in their family. Maybe there is some violence in the family, and this is the factor that impacts later on the adherence [HCP in Latvia, Kielmann et al., 2018, pp.8].Citation23
Discussion
This review synthesized qualitative evidence on the potential mechanisms through which personal, social, health system, and structural factors influence ATT-related behavior in high-income, low-incidence countries. While our findings suggest that treatment-related and so-called “personal” characteristics of individuals were directly linked to ATT-related behavior, we also found that the qualitative studies rarely looked at “adherence” or the act of taking medicines per se in isolation. Instead, the majority of studies situated individual motivation and capacity to take ATT within a complex interplay of social relationships, health systems’ features, and structural circumstances. We depict these relational dynamics of treatment behavior among individuals on ATT in .
Figure 2 Relational dynamics of being on anti-tuberculosis treatment.
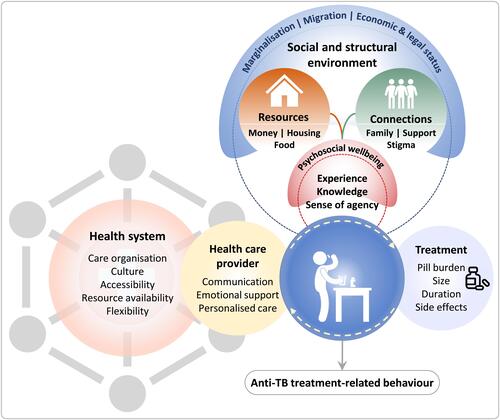
The vast majority of studies concurred on the vital role of health systems factors in shaping experiences of ATT, including adherence behavior. The key mechanisms of influence described were access to TB-related information and prior experience of health services, as well as the balance of power, cultural expectations, and trust between HCPs and patients. Next in order of frequency, studies describing the influence of personal factors drew attention to the mechanisms that led to sub-optimal adherence in given contexts, rather than emphasizing individual traits per se. They highlight the importance of treatment literacy at both individual and collective levels, but also suggest that individual agency could be compromised or thwarted through life circumstances. Social marginalization, isolation, and co-morbidities led, in a number of studies, to fragmented treatment-seeking pathways or poor treatment behavior.
Two-thirds of studies reported on the influence of structural factors including health and social policies, funding for TB services, and socio-economic conditions on the livelihoods and social positions of individuals with TB. Socio-economic marginality and limited social capital operated as mechanisms constraining individuals’ ability to effectively navigate TB services and ATT. Next in order of importance, studies reporting on social factors illustrated how the experience of being a “TB patient” was embedded within social structures rather than being merely an artefact of the health system. Finally, studies describing treatment-related barriers to ATT adherence showed that it was not only the commonly reported pill burden, lengthy duration, or side-effects of medication that were problematic, but also their disruptive effects on everyday social and working lives, livelihood strategies, and routines. This is an important consideration for HCP monitoring TB patients on treatment. Side-effects are not “just” physiological but experiential: like the tablets themselves, their “management” spills over the boundaries of being a “patient”.
This scoping review lends support to our relational approach to the experience of taking ATT in three ways. First, the studies reviewed highlight the complex and dynamic interplay across multiple socio-ecological levels; individual treatment-taking behavior is rarely an isolated or self-driven phenomenon but operates through complex and inter-related mechanisms. For individuals struggling to stay on ATT, adherence was compromised by “chaotic lifestyles” and co-morbidities, including substance misuse and mental health issues. These circumstances were, in turn, often associated with structural marginality, deprivation, and social isolation that, in some cases, had collective historical antecedents. Psychosocial factors were intertwined with individuals’ social positions, their sense of community, identity, and worth. “Successful” navigation of the health system, and in particular experience of the TB care system, was contingent on meaningful exchange with HCP. This included, but was not restricted to, language and health literacy. In practical terms, the review makes the case that risk factors for “poor adherence” are seldom individual traits – but reflect rather more complex social and structural issues. A relational approach can help HCP to distinguish between practical “modifiable” barriers to adherence and disempowering circumstances that may require a different form of dialogue and support for individuals on ATT. Our review also suggests that understanding the nature of family and other social support that individuals on treatment have recourse to is vital: drawing on positive social connections can strengthen individual’s engagement with treatment regimens; however, conversely, social networks can change and become fragmented or even dissipate in the case of a TB diagnosis.Citation53
Second, in situating “adherence behavior” within the extended frame of “being on ATT”, we saw that individuals’ pre-existing circumstances, conditions, and experiences of health-seeking and the health system influenced their views on treatment and their ability to “commit” to long-term, regular medicine-taking. Personal circumstances of individuals on treatment change: the physiological experience of treatment (eg, side-effects) fluctuates alongside individuals’ relationships and their social networks, as well as their access to structural resources such as housing, income, and employment. Our review suggests that there is a need to recognize that patients’ frames of experience relevant to treatment-taking behavior may differ substantially from HCPs’ definitions and clinical pathways that are more narrowly restricted to the “window of opportunity” for professional intervention. These factors indicate the need for regular re-assessment rather than a one-off checklist approach to evaluate risk factors associated with likelihood of poor adherence.
Past experience and shared collective histories can shape individuals’ perceptions of treatment and engagement with health services. In the accounts of indigenous individuals as well as those of substance users, ATT sometimes evoked negative past experiences of social isolation and incarceration. A few studies indicated too that migrants’ histories of health-seeking in their home countries might influence willingness, agency, and communication with HCPs in the host countries. These insights suggest that eliciting and acknowledging individuals’ previous experiences of the health system, both negative and positive, may be important in the clinical consultation as these insights can help to explain treatment behavior that is perceived to be “at odds” with what is expected of individuals on ATT.
Third, the review highlights the role of context in mediating how determinants work to support or hinder adherence in different settings. By “context”, we refer to the broader political and policy features of the countries that are represented in this review, health systems models and normative care practices, and the narrower and more subtle social and cultural constructs of self, identity, and “community”. While some acute factors, such as severe side-effects or the lack of finances or housing, may operate similarly in terms of their impact on treatment behavior across a variety of settings, other factors, like health literacy, stigma, and social support, can be more complex in nature, with variable impacts on treatment adherence. This point is particularly relevant for current scenarios of TB in HILI countries, where differences in individuals’ understanding and experience of treatment for TB may be confounded by other factors such as gender, ethnicity, and co-morbidities. Practically speaking, our review suggests that HCPs need to ideally look beyond the TB diagnosis to see how these factors might shape perceptions of TB and the relative value of taking ATT (in relation to other issues faced) and the social and psychological experience of being on treatment, including taking medication.Citation53 Thus, for example, gender norms and constructs of health and agency in health-seeking may influence treatment behavior for ATT. Individuals with co-morbidities may rank TB lower in terms of the disruption caused to their lives than an illness or condition perceived to be more acute.
Strengths and Limitations
Quantitative studies and reviews looking at factors linked to ATT adherence, as well as the association of ATT adherence with treatment outcomes are frequently challenged by the lack of standardization in definitions and measurement of adherence behavior,Citation12,Citation13 as well as the limited consensus over what constitutes “clinically important” non-adherence.Citation54 The assessment of factors affecting adherence often narrowly focuses on the act of taking tablets as prescribed by a HCP, resulting in over-emphasis on individual-level cognition, agency, and responsibility for adherence. Instead, our review starts from the premise that “adherence” is primarily a clinically driven outcome that should be seen within the broader frame of treatment experience. The limitation of this approach, namely that we are unable to advocate for a precise, standardized way of assessing and measuring “adherence”, is ironically also the strength of the review. In contrast to quantitative reviews of determinants of adherence which reify the phenomenon of adherence as a discrete behavior, our qualitative review starts from the phenomenological experience of ATT, that is the subjective lived experience of being on treatment. Here, individuals’ treatment-related behavior occurs within a complex interplay of factors and processes, functions at multiple socio-ecological levels, and is shaped by individuals’ evolving social and structural circumstances.
A further potential limitation is that no quality assessment was performed. This is in line with the methodology for scoping reviews we followed.Citation25 Quality control was limited to the inclusion of peer-reviewed publications only. Additionally, the selection of papers was restricted to those published in English, which may have led to language bias.
Conclusion
Treatment adherence is conventionally understood as the extent to which individual medicine-taking behavior conforms or diverges from a time-bound regimen prescribed by a health provider. This scoping review supports a relational approach to understanding ATT adherence in HILI countries. We argue that adherence is one aspect of ATT-related behavior that occurs within an extended care-seeking trajectory as well as in a dynamic context, in which social and structural circumstances change with sometimes drastic effects on the welfare of individuals and their capacity to engage with health systems, let alone treatment regimens. To date, there has been greater emphasis placed on elucidating the challenges individuals face in staying on ATT in LMIC, not just because the numbers of individuals living with TB are far greater, but also because there is an implicit assumption that individuals with TB in HILI benefit from better access to systems with adequate resources to good care. The review highlights that this may not always be the case: TB health-seeking and treatment behavior including adherence to ATT may be compromised through hidden vulnerabilities, potentially less visible to HCP than in LMIC settings where TB is endemic. To improve person-centered clinical management of ATT, there is a need to acknowledge the ways in which ATT both disrupts and is managed within the everyday lives of individuals with TB. HCPs, through more regular dialogue with TB patients, can assess how personal circumstances, as well as support and resources available, may change over the course of treatment, and the consequences thereof for patterns of treatment-related behavior. This approach is now being taken forward within a cluster randomized trial of a manualized intervention using materials designed to assess the ongoing risk of non-adherence and provide ways to manage it over the course of treatment for TB.Citation55 Given the diversity in ethnicity and social backgrounds of individuals with TB in HILI countries, there is need for more nuanced consideration of the context-specific nature of social and cultural norms that affect individual and collective experiences of being a TB patient.
Acknowledgments
We are grateful to the wider IMPACT team for their support, in particular to Colin Campbell, Jacqui White, Mike Mandelbaum, Heinke Kunst, and Alison Rodger who contributed through ongoing discussion and comment on earlier iterations of the scoping review methodology and findings.
Disclosure
Dr Aaron S Karat reports grants from National Institute of Health Research (UK), during the conduct of the study; personal fees from The Aurum Institute (South Africa), personal fees, non-financial support from Vital Strategies (Singapore), personal fees from The University of Cape Town (South Africa), personal fees from Center for Health Policies and Studies (Moldova), personal fees, non-financial support from Bill & Melinda Gates Foundation (USA), personal fees, non-financial support from Bloomberg Philanthropies (USA), non-financial support from The Africa Health Research Institute (South Africa), non-financial support from University College London (UK), outside the submitted work. Dr Helen R Stagg reports grants from Medical Research Council, UK, nothing from National Institute for Health Research, UK, during the conduct of the study; received travel expenses from Korean CDC and Johnson and Johnson (makers of Bedaquiline), and from Latvian Society Against Tuberculosis (funding through Otsuka and Johnson and Johnson), outside the submitted work. Ms Marcia Darvell reports grants from NIHR, during the conduct of the study. Professor Robert Horne reports personal fees from Spoonful of Sugar Ltd a UCL business Company, outside the submitted work. Dr Karina Kielmann reports grants from National Institute for Health Research (NIHR) United Kingdom, during the conduct of the study.
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Lienhardt C, Glaziou P, Uplekar M, Lönnroth K, Getahun H, Raviglione M. Global tuberculosis control: lessons learnt and future prospects. Nat Rev Microbiol. 2012;10(6):407–416. doi:10.1038/nrmicro2797
- Fears R, Kaufmann S, Ter Meulen V, Zumla A, Group EW. Drug-resistant tuberculosis in the European Union: opportunities and challenges for control. Tuberculosis. 2010;90(3):182–187. doi:10.1016/j.tube.2010.03.008
- World Health Organization. Global health observatory data repository. 2020. Available from: https://apps.who.int/gho/data/node.main.1315?lang=en. Accessed September 13, 2020.
- World Health Organization. Framework towards tuberculosis elimination in low-incidence countries; 2014. Available from: https://www.who.int/tb/publications/elimination_framework/en/. Accessed September 26, 2020.
- World Health Organization. Global tuberculosis report 2019; 2019. Available from: https://www.who.int/teams/global-tuberculosis-programme/global-report-2019. Accessed September 26, 2020.
- World Bank. World Bank country and lending groups; 2020. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed September 26, 2020.
- Gupta RK, Lipman M, Story A, et al. Active case finding and treatment adherence in risk groups in the tuberculosis pre-elimination era. Int J Tuberc Lung Dis. 2018;22(5):479–487. doi:10.5588/ijtld.17.0767
- Heuvelings CC, de Vries SG, Grobusch MP. Tackling TB in low-incidence countries: improving diagnosis and management in vulnerable populations. Int J Infect Dis. 2017;56:77–80.
- Public Health England. Tackling tuberculosis in under-served populations: a resource for TB control boards and their partners; 2019. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/773730/Tackling_TB_in_Under-Served_Populations_-_a_Resource_for_TBCBs_and_partners.pdf. Accessed December 20, 2020.
- Pradipta IS, Forsman LD, Bruchfeld J, Hak E, Alffenaar J-W. Risk factors of multidrug-resistant tuberculosis: a global systematic review and meta-analysis. J Infect. 2018;77(6):469–478. doi:10.1016/j.jinf.2018.10.004
- Anderson C, Anderson SR, Maguire H, Hayward AC, Story A. Tuberculosis in London: the convergence of clinical and social complexity. Eur Respir J. 2016;48(4):1233–1236. doi:10.1183/13993003.00749-2016
- Stagg HR, Flook M, Martinecz A, et al. All nonadherence is equal but is some more equal than others? Tuberculosis in the digital era. ERJ Open Res. 2020;6(4):00315–2020. doi:10.1183/23120541.00315-2020
- Jones ASK, Bidad N, Horne R, et al. Determinants of non-adherence to anti-TB treatment in high income, low TB incidence settings: a scoping review. Int J Tuberc Lung Dis.
- Mason PH, Degeling C. Beyond biomedicine: relationships and care in tuberculosis prevention. J Bioethical Inq. 2016;13(1):31–34. doi:10.1007/s11673-015-9697-6
- Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med. 2007;4(7):e238–e238. doi:10.1371/journal.pmed.0040238
- Horne R, Cooper V, Wileman V, Chan A. Supporting adherence to medicines for long-term conditions: a perceptions and practicalities approach based on an extended common-sense model. Eur Psychol. 2019;24(1):82–96. doi:10.1027/1016-9040/a000353
- Pradipta IS, Houtsma D, van Boven JFM, Alffenaar J-WC, Hak E. Interventions to improve medication adherence in tuberculosis patients: a systematic review of randomized controlled studies. Npj Prim Care Respir Med. 2020;30(1):21. doi:10.1038/s41533-020-0179-x
- Amico KR, Mugavero M, Krousel-Wood MA, Bosworth HB, Merlin JS. Advantages to using social-behavioral models of medication adherence in research and practice. J Gen Intern Med. 2018;33(2):207–215. doi:10.1007/s11606-017-4197-5
- World Health Organization. The end TB strategy: global strategy and targets for tuberculosis prevention, care and control after 2015; 2015. Available from: https://www.who.int/tb/post2015_strategy/en/. Accessed September 13, 2020.
- World Health Organization.Adherence to long-term therapies: evidence for action; 2003. Available from: https://www.who.int/chp/knowledge/publications/adherence_full_report.pdf. Accessed May 29, 2020.
- Jaam M, Awaisu A, Mohamed Ibrahim MI, Kheir N. A holistic conceptual framework model to describe medication adherence in and guide interventions in diabetes mellitus. Res Soc Adm Pharm. 2018;14(4):391–397. doi:10.1016/j.sapharm.2017.05.003
- National Institute for Health Care Excellence. Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence. Clinical guideline CG76; 2009. Available from: https://www.nice.org.uk/Guidance/CG76. Accessed March 18, 2021.
- Kielmann K, Vidal N, Riekstina V, et al. Treatment is of primary importance, and social assistance is secondary: a qualitative study on the organisation of tuberculosis (TB) care and patients’ experience of starting and staying on TB treatment in Riga, Latvia. PLoS One. 2018;13(10):e0203937. doi:10.1371/journal.pone.0203937
- Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications: new taxonomy for adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705. doi:10.1111/j.1365-2125.2012.04167.x
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi:10.1080/1364557032000119616
- Craig GM, Zumla A. The social context of tuberculosis treatment in urban risk groups in the United Kingdom: a qualitative interview study. Int J Infect Dis. 2015;32:105–110. doi:10.1016/j.ijid.2015.01.007
- Curtis R, Friedman SR, Neaigus A, Jose B, Goldstein M, Des Jarlais DC. Implications of directly observed therapy in tuberculosis control measures among IDUs. Public Health Rep. 1994;109(3):319–327.
- Kawatsu L, Uchimura K, Ohkado A, Kato S. A combination of quantitative and qualitative methods in investigating risk factors for lost to follow-up for tuberculosis treatment in Japan – are physicians and nurses at a particular risk?. PLoS One. 2018;13(6):e0198075. doi:10.1371/journal.pone.0198075
- Pujol-Cruells A, Vilaplana C. Specific interventions for implementing a patient-centered approach to TB care in low-incidence cities. Front Med. 2019;6:273. doi:10.3389/fmed.2019.00273
- Shiratani KN. Psychological changes and associated factors among patients with tuberculosis who received directly observed treatment short-course in metropolitan areas of Japan: quantitative and qualitative perspectives. BMC Public Health. 2019;19(1):1642. doi:10.1186/s12889-019-8001-9
- Grace J, Chenhall R. A rapid anthropological assessment of tuberculosis in a remote aboriginal community in Northern Australia. Hum Organ. 2006;65(4):387–399. doi:10.17730/humo.65.4.69egxry83x2v03r8
- Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi:10.1097/00005650-198601000-00007
- Gerrish K, Naisby A, Ismail M. Experiences of the diagnosis and management of tuberculosis: a focused ethnography of Somali patients and healthcare professionals in the UK. J Adv Nurs. 2013;69(10):2285–2294. doi:10.1111/jan.12112
- Searle A, Park J, Littleton J. Alliance and compliance in tuberculosis treatment of older Pakeha people in Auckland, New Zealand. Int J Tuberc Lung Dis. 2007;11(1):72–77.
- Moffatt J, Mayan M, Long R. Sanitoriums and the Canadian colonial legacy. Qual Health Res. 2013;23(12):1591–1599. doi:10.1177/1049732313508843
- Macdonald ME, Rigillo N, Brassard P. Urban aboriginal understandings and experiences of tuberculosis in Montreal, Quebec, Canada. Qual Health Res. 2010;20(4):506–523. doi:10.1177/1049732309360538
- Wannheden C, Westling K, Savage C, Sandahl C, Ellenius J. HIV and tuberculosis coinfection: a qualitative study of treatment challenges faced by care providers. Int J Tuberc Lung Dis. 2013;17(8):1029–1035. doi:10.5588/ijtld.12.0446
- Nnoaham KE, Pool R, Bothamley G, Grant AD. Perceptions and experiences of tuberculosis among African patients attending a tuberculosis clinic in London. Int J Tuberc Lung Dis. 2006;10(9):1013–1017.
- Marra CA, Marra F, Cox VC, Palepu A, Fitzgerald JM. Factors influencing quality of life in patients with active tuberculosis. Health Qual Life Outcomes. 2004;2(58):58. doi:10.1186/1477-7525-2-58
- Gibson N, Cave A, Doering D, Ortiz L, Harms P. Socio-cultural factors influencing prevention and treatment of tuberculosis in immigrant and aboriginal communities in Canada. Soc Sci Med. 2005;61(5):931–942. doi:10.1016/j.socscimed.2004.10.026
- Wieland ML, Weis JA, Yawn BP, et al. Perceptions of tuberculosis among immigrants and refugees at an adult education center: a community-based participatory research approach. J Immigr Minor Health. 2012;14(1):14–22. doi:10.1007/s10903-010-9391-z
- Joseph HA, Waldman K, Rawls C, Wilce M, Shrestha-Kuwahara R. TB perspectives among a sample of Mexicans in the United States: results from an ethnographic study. J Immigr Minor Health. 2008;10(2):177–185. doi:10.1007/s10903-007-9067-5
- Konradsen H, Lillebaek T, Wilcke T, Lomborg K. Being publicly diagnosed: a grounded theory study of Danish patients with tuberculosis. Int J Qual Stud Health Well-Being. 2014;9(1):23644. doi:10.3402/qhw.v9.23644
- Sagbakken M, Bjune GA, Frich JC. Humiliation or care? A qualitative study of patients’ and health professionals’ experiences with tuberculosis treatment in Norway: humiliation or care? Scand J Caring Sci. 2012;26(2):313–323. doi:10.1111/j.1471-6712.2011.00935.x
- Zuniga JA, Munoz SE, Johnson MZ, Garcia A. Tuberculosis treatment for Mexican Americans living on the U.S.-Mexico border. J Nurs Scholarsh. 2014;46(4):253–262. doi:10.1111/jnu.12071
- Yamada S, Caballero J, Matsunaga DS, Agustin G, Magana M. Attitudes regarding tuberculosis in immigrants from the Philippines to the United States. Fam Med. 1999;31(7):477–482.
- van der Oest C, Chenhall R, Hood D, Kelly P. Talking about TB: multicultural diversity and tuberculosis services in Waikato, New Zealand. N Z Med J. 2005;118(1216):62–72.
- Kulane A, Ahlberg BM, Berggren I. “It is more than the issue of taking tablets”: the interplay between migration policies and TB control in Sweden. Health Policy (New York). 2010;97(1):26–31. doi:10.1016/j.healthpol.2010.02.014
- Craig GM, Joly LM, Zumla A. ‘Complex’ but coping: experience of symptoms of tuberculosis and health care seeking behaviours - a qualitative interview study of urban risk groups, London, UK. BMC Public Health. 2014;14(1):618. doi:10.1186/1471-2458-14-618
- Komarnisky S, Hackett P, Abonyi S, Heffernan C, Long R. “Years ago”: reconciliation and first nations narratives of tuberculosis in the Canadian Prairie Provinces. Crit Public Health. 2016;26(4):381–393. doi:10.1080/09581596.2015.1067672
- Boudioni M, McLaren S, Belling R, Woods L. Listening to those on the frontline: service users’ experiences of London tuberculosis services. Patient Prefer Adherence. 2011;5:267–277. doi:10.2147/PPA.S20361
- Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Social determinants of health discussion paper 2 (policy and practice). World Health Organization; 2010. Available from: https://apps.who.int/iris/bitstream/handle/10665/44489/9789241500852_eng.pdf?sequence=1&isAllowed=y. Accessed January 22, 2021.
- Karat AS, Jones AS, Abubakar I, et al. “You have to change your whole life”: a qualitative study of the dynamics of treatment adherence among adults with tuberculosis in the United Kingdom. J Clin Tuberc Mycobact Dis. 2021;23:100233 doi:10.1016/j.jctube.2021.100233.
- Vernon A, Fielding K, Savic R, Dodd L, Nahid P. The importance of adherence in tuberculosis treatment clinical trials and its relevance in explanatory and pragmatic trials. PLOS Med. 2019;16(12):e1002884. doi:10.1371/journal.pmed.1002884
- Stagg HR, Abubakar I, Campbell CN, et al. IMPACT study on intervening with a manualised package to achieve treatment adherence in people with tuberculosis: protocol paper for a mixed-methods study, including a pilot randomised controlled trial. BMJ Open. 2019;9:e032760.
- Sagbakken M, Frich JC, Bjune GA, Porter JD. Ethical aspects of directly observed treatment for tuberculosis: a cross-cultural comparison. BMC Med Ethics. 2013;14:25. doi:10.1186/1472-6939-14-25
- Kelly P. Isolation and stigma: the experience of patients with active tuberculosis. J Community Health Nurs. 1999;16(4):233–241. doi:10.1207/S15327655JCHN1604_3
- Kielmann K, Vidal N, Karat AS, Stagg HR, Lipman M, on behalf of the IMPACT study group (NIHR 16/88/06). Supporting adherence to treatment for tuberculosis (TB): a relational view. Int J Tuberc Lung Dis. 2019;22(11):S385.
